Nomore Nyengerai 1, Maxwell Mhlanga 2*
- Department of Public Health, University of Zambia
- Centre of Gender Equity, University of Global Health Equity, Zimbabwe
* Corresponding author: Maxwell Mhlanga., Centre of Gender Equity, University of Global Health Equity. Rwanda. E-mail: mmhlanga@ughe.org
Nomore Nyengerai, Maxwell Mhlanga
Review article
DOI:10.32549/OPI-NSC-107
Submitted: 27 May 2024
Revised: 26 June 2024
Accepted: 26 June 2024
Published online: 2 July 2024
License: This article is licensed under the Creative Commons Attribution - Non Commercial - No Derivatives 4.0 (CC BY NC ND 4.0) international license.
Abstract:
Immunization is one of the most cost-effective nursing interventions aimed at reducing ill health and premature death among children. Despite tremendous efforts by governments, vaccination coverage remains low, especially in developing countries. Masvingo district is one of the districts with low vaccination coverage in the country.
Cite this article
ABSTRACT
Introduction: Immunization is one of the most cost-effective nursing interventions aimed at reducing ill health and premature death among children. Despite tremendous efforts by governments, vaccination coverage remains low, especially in developing countries. Masvingo district is one of the districts with low vaccination coverage in the country.
Objectives: This study sought to assess immunization coverage, identify determinants of vaccination coverage and assess factors associated with low full immunization coverage in Masvingo district, Zimbabwe.
Methods: An analytical cross-sectional study design was conducted between January 2019 and February 2019. Masvingo province was purposively selected due to its low vaccination coverage (60.3%) according to the Zimbabwe Demographic and Health Survey 2015. WHO cluster sampling was used to select households. A total of 354 children and their mothers residing in Masvingo district were recruited for the study. Pre-tested interviewer-administered questionnaires were used to collect data. Bivariate analysis was employed to assess factors associated with low vaccination coverage.
Results: An estimated 89.5% of children aged 12-23 months were fully vaccinated by card or mothers’ recall. Factors significantly associated with full vaccination coverage rates (P<0.001) included birth order, distance to the nearest health facility, waiting time, place of birth, number of Antenatal care visits, possession of a vaccination card, place of residence, mother/caregiver’s highest level of education, household expenditure per month, and overall knowledge of the vaccination schedule. After controlling for all these factors, only household expenditure per month (P=0.001), having a vaccination card (P=0.047), and overall knowledge of the vaccination schedule (P=0.002) were statistically significant predictors of full vaccination coverage rates.
Conclusion: Although full vaccination coverage is improving, it is still below the Global Vaccine Action Plan target. Factors associated with low full vaccination coverage include marital age, marital status, level of education, religion, household expenditure, distance to the health center, waiting time, and Antenatal Care and Post-natal Care care utilization. There is no single factor solely responsible for low vaccination coverage; rather, it is influenced by a combination of multiple factors. Nursing interventions at community level should focus on increasing community mobilization strategies that foster saturation coverage to achieve herd immunity for all vaccine preventable child diseases.
Keywords: Vaccination coverage, utilization, children, cross-sectional study, community mobilization, vaccination hesitancy
INTRODUCTION
In 1974, the World Health Organization (WHO) launched the Expanded Programme on Immunization (EPI) and nurses have played a pivotal role in the success of this programme and in promoting universal health coverage through the primary health care approach. The aim of the EPI was to administer life-saving vaccines to all eligible children across the globe. At that time, only six diseases—pertussis, poliomyelitis, tuberculosis, tetanus, measles, and diphtheria—were targeted [1]. Vaccination is regarded as the most economical child survival intervention, improving children’s quality of life while preventing sickness, disability, and death from vaccine-preventable illnesses [1]. According to UNICEF, each dollar spent on vaccination brings about USD 44 in economic benefits through therapeutic cost savings and productive time loss [2]. Nurses are at the centre of successful child vaccination programmes through as they are the ones who implement the Expanded programme of immunisation at both health facility and community level.
According to WHO, the proportion of children vaccinated against the six vaccine-preventable diseases was around 5% initially. This figure has increased to over 80% during the past four decades [3]. This improvement follows the integration of immunization services into broader public health services by many governments. The Global Vaccine Action Plan (GVAP) was launched in 2012 by WHO and partners, with the primary goal of ensuring equitable access to vaccines, thereby preventing avoidable child illnesses, disability, and death. The coverage level set by GVAP for countries is 90% and above for DTP3 and a minimum of 80% in each district by the year 2020 [3]. WHO highlighted that only 123 countries managed to achieve this target by 2017 [1].
Despite the remarkable increase in global vaccination coverage, it still falls below the target set by GVAP [1]. Due to inequitable distribution of nursing and general health services, including immunization, many children, particularly in developing countries, remain unvaccinated. WHO and UNICEF predict that two in every 20 children are left unvaccinated, while 20% of children do not receive all required vaccine doses. In 2017 alone, around 19.9 million children did not receive all three doses of DTP3 during their first year of life. Additionally, about 33.3% of children under 5 years old die from diseases that could be prevented by vaccines [1].
The government of Zimbabwe, through the Ministry of Health and Childcare, introduced the Zimbabwe Expanded Programme on Immunization (ZEPI) in 1982 [4]. Initially, the government adopted the WHO recommendation of vaccination against only six diseases. As research continued and new vaccines were developed, the government made great strides in incorporating them into routine immunization [4]. In 1999, the Hepatitis B vaccine was introduced, followed by the Pentavalent vaccine (DTP-HB-Hib) in 2008. Haemophilus influenzae was included as part of the Pentavalent vaccine. To combat pneumonia, the Pneumococcal Conjugate Vaccine (PCV) was introduced in 2012, followed by the Rotavirus vaccine in 2014 to fight diarrheal diseases [4]. The second dose of the measles vaccine, including the rubella component, was introduced in 2015. In 2018, the government rolled out the Human Papillomavirus (HPV) vaccine nationwide for girls aged 10 to 14 years following a successful pilot project started in 2014.
In Zimbabwe, children are considered fully vaccinated if they receive the following: BCG at birth or first contact, three doses of oral polio vaccine, three doses of Pentavalent, three doses of PCV, two doses of Rotavirus vaccine, and a single dose of measles [4]. These doses should be administered during the first year of life. The Multiple Indicator Cluster Survey (MICS) of 2014 revealed that only 69.2% of children aged 12 to 23 months were fully vaccinated at the time of the survey, and 5% were unvaccinated [5]. Similarly, the Zimbabwe Demographic and Health Survey (ZDHS) of 2015 found that only 73% of children in the same age group were fully vaccinated, while 9.8% were unvaccinated [6]. Despite differences in survey methodologies, both highlighted inadequacies in meeting the GVAP targets for DTP3 (90%) and measles-rubella (95%). This leaves the country vulnerable to outbreaks of vaccine-preventable diseases. Except for BCG, the Multiple Cluster Survey of 2014, all other vaccine coverages were far below the GVAP target [6].
According to both the Multiple Indicator Cluster Survey and the Demographic Health Survey, Masvingo province had the lowest vaccination coverage in the country, with 78.1% and 60.3% respectively [6]. The 2015 Demographic Health Survey revealed that Masvingo province recorded the highest proportion (20.7%) of unvaccinated children.
In Zimbabwe, children are vaccinated through static and outreach services conducted by community nurses and primary health care nurses. According to the Ministry of Health and Childcare, all primary course vaccines should be administered during the first year of life. BCG is given at birth or the first contact, while the other three sets of vaccines are administered from 6 weeks to 14 weeks at four-week intervals. Thereafter, the measles-rubella vaccine is given at 9 months. Given the vulnerability of children under 2 years to various illnesses, polio and measles vaccines are administered at 18 months to boost their immune systems. Extra doses are typically given during campaigns.
The Global Alliance for Vaccines (Gavi) and partners initiated the EPI programme in 1974 to expand immunization services and prevent avoidable illnesses and deaths in children. From 1974 to 2014, global coverage of EPI services increased from 5% to 80% [3]. Although global coverage shows an increasing trend, it remains below the GVAP targets [1]. Consequently, many children, especially in developing countries, are either unvaccinated or partially vaccinated. WHO and UNICEF of 2018 report that two out of every 20 children are left unvaccinated, while one does not complete all recommended vaccine doses [1]. WHO estimates that approximately 19.9 million children did not receive the DTP3 vaccine, and around 33.3% of children under the age of 5 die from vaccine-preventable illnesses [1].
The government of Zimbabwe identified three diseases (pneumonia, diarrhoea, and measles) as among the top five causes of avoidable and premature death in children under 5 years. This implies that the vaccination programme is a critical child survival activity that can improve children’s quality of life [7]. The government and EPI partners provide technical, financial, and coordination support to expand, improve, and intensify the EPI programme. Various initiatives have been implemented to improve immunization coverage, including health worker training, providing vehicles for EPI activities, supplying cold chain equipment, and implementing strategies like Reach Every Child (RED), My Village My Home, and Child Health Days [8]. However, despite these initiatives, vaccination coverage decreased from 90% in 2014 to 87% in 2017 [9]. Masvingo district’s coverage has remained persistently low, consistent with findings from MICS of 2014 and DHS of 2015 [5-6]. Although several studies have explored factors linked to low vaccination coverage, none have been conducted specifically in Masvingo district. Given the persistent low immunization coverage in Masvingo district, determining the factors associated with this low performance is critical. The findings will inform health promotion messaging and ultimately generate demand and utilization of immunization services.
Objective: This study sought to assess immunization coverage, identify determinants of vaccination coverage and assess factors associated with low full immunization coverage in Masvingo district, Zimbabwe.
MATERIALS AND METHODS
Study setting and design
This study was carried out in Masvingo district, Zimbabwe. The district is 292 km to the south of Zimbabwe’s capital, Harare and is bordered by Gutu district on the north, Chiredzi district south, Zaka and Chivi districts on the east and west respectively. The latest data based on 2012 census projections showed that its’ population is approximately 224,209 and 7,041 are under-5-year-old children [4].
An analytical cross-sectional study was conducted between January 2019 and February 2019. Masvingo province was purposively selected because she had the lowest (60.3%) vaccination coverage according to ZDHS (2015) [6]. WHO cluster sampling was used for selecting the households.
Study population and sampling
The source population of this study were all children within 12 to 23 months age group with their parents residing in Masvingo district. The study population consisted of 354 children within this age group whose mothers/caregivers were sampled.
Case definition: A Case was any child aged 12 to 23 months residing in Masvingo district full immunised between January 2019 and February 2019 confirmed by a child health card/ mother recall.
Sample Size and Sampling Methodology
Masvingo province has the lowest (60, 3%) vaccination coverage according to ZDHS thus was purposively samples [6]. Also, the province had the highest percentage (20.7%) of unvaccinated children with 12 months to 23 months. Furthermore, the administrative data from 2005-2017 revealed that Masvingo district was one of the persistent low performers in the province.
The sample size required was determined using single proportion population formula with 5% margin of error assumption (D), 95% confidence level (), and the immunization coverage assumed between 60% in Masvingo to 87% in Matabeleland North as per ZDHS 2015. Therefore, we we hypothesized a prevalence p = 73%, so that the hypothesized prevalence is within the range [68%, 78%]. The required sample size for this study was computed as follows:
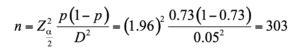
where n = minimum estimate sample size Zα/2 at 95% CI is 1.96; D =margin of error- 5%; hypothesized a prevalence of fully immunized coverage p = 73%. Finally, the sample size was enlarged to 354 mothers to reduce possible statistical biases due data loss.
Sampling was done in accordance to WHO’s multistage cluster sampling [9]. The district was divided into three clusters namely Masvingo South, North and central. Then, fifteen villages were selected from each cluster making a total of 45 villages from all clusters using lottery method. The total sample size was allocated proportionally to villages depending on the number of 12-23 months old children. The first child from each village was selected randomly and the rest of the children were selected from subsequent households until the sample size is fulfilled. In case of two and above eligible children in a household, the investigator will randomly select one child.
Inclusion and Exclusion Criteria
Inclusion Criteria
- All mothers/caregivers aged 16 years and above.
- Mothers/caregivers of children aged 12-23 months residing in Masvingo district for at least 12 months prior to data collection date.
- Adults willing and able to give informed consent to take part.
Exclusion Criteria
- All mothers aged 15 years and below
- All mothers/ caregivers of children below the age of 12 months and those above 23 months.
- Mothers/ caregivers of children residing outside Masvingo district or has been in Masvingo district for a period less than 12 months.
- Mothers/caregivers who were unwilling to participate or incapacitated to give consent.
Data Collection
The survey was conducted in Masvingo district from January to February 2019. The investigator collected information on demography, vaccination status, health services utilisation and other relevant information using interviewer-administered structured questionnaires. The questionnaires were developed from review of immunisation literature, adapted from Zimbabwe Demographic Health Survey and WHO questionnaires for immunisation coverage.
The questionnaire was evaluated for test-retest reliability with 10 people randomly selected at Zaka rural health centre who were from non-participating villages. The test-retest assessments were 5 days apart. Participants were not told that they would be re-tested to minimise bias. Item completion of the questions and percentage agreement between test–retest assessments was calculated for each question and it was in the range of 90-100% for all questions. Based on these results the questionnaire was adopted for use in the study.
Face and construct validity was enhanced through subjecting the questionnaire to review by Experts public health and aligning the research instrument to the conceptual framework that informed behaviour and immunisation services uptake.
The questionnaires were pretested at Gutu Mission Hospital to check for acceptability of the data collection tool, to estimate response rate, questions that are difficult to answer and estimating the length of time to complete the questionnaire so that adjustments were made to the data collection tools. The pretested study area was not included into his study.
Dependent variable
In this study, the vaccination status of the child was the dependent variable. According to Ministry of Health and Child Care ZEPI policy, children are said to be fully vaccinated when given BCG (one dose), Polio, PCV and Pentavalent (three doses each), Rotavirus (two doses) and Measles Rubella (one dose) during the first year of life [6]. In this analysis, fully vaccination status was a dummy variable derived from summing up all the above stated vaccines as per Zimbabwe Expanded Programme on Immunisation schedule. The information on antigens given and dates of administration was extracted from children’s vaccination records or mothers’ recall if records were not available. In cases where vaccination records were absent, the caregiver was asked to report the period and number of doses for each antigen given in order to ascertain the vaccination status of the child. In a bid to minimise recall bias, recalling techniques like period of administration, route and site of administration were included in the instruments.
The vaccination dates were recorded against each antigen from the vaccination card or caregiver’s recall. Vaccination dates were checked against the recommended ZEPI schedule. In cases where the vaccination date was wrongly or not recorded, the antigens were considered as not administered. Children with 12 months to 23 months’ vaccination status were categorised as fully immunised and partially or unvaccinated. The child was considered partially/ incompletely vaccinated when one or more doses were missed. Children who did not receive any antigen were classified as unvaccinated.
Independent variables
The demographic and socio-economic characteristics of the child, mother, health systems, and utilization were the independent variables. These included the sex, age, and birth order of the child; the age, education level, occupation, and marital status of the mother; religion; distance from the health facility; travel time; health facility utilization; place of residence (rural-urban); and communication and knowledge of the immunization schedule.
Data Analysis
In this analysis, SPSS version 20 and STATA 15 were used for capturing, cleaning and tabularisation of all the data collected using questionnaires. The descriptive data was presented in tables as figures as frequencies and percentages. The chi-square test or Fisher’s exact test were performed to evaluate significant differences in proportions or percentages between the two groups. Fisher’s exact test was used where the chi-square test was not appropriate.
Univariate analysis was employed to describe distribution of children’s full vaccination status by characteristics of child, mother and health system and utilisation. Predictors for the vaccinations of the children were assessed by dichotomizing outcome variable (child vaccination status) into fully vaccinated and not fully vaccinated. Predictor variables having a p-value < 0.05 were taken into a multivariable logistic regression analysis to see associations between dependent and independent variables. All independent variables identified to significantly associate with the vaccination statuses of the children at bivariate analysis (p-value < 0.05) were taken into a multivariable analysis. We used the “ENTER” approach for multi-variable regression analysis to assess the association between children’s full vaccination status and factors associated with their vaccination status. Finally, all p-values were always two-sided and all tests with p-value (P) < 0.05 were considered significant.
Ethical Considerations
The investigators obtained ethical approval from the Ethics Committee of the University of Lusaka and the Medical Research Council of Zimbabwe approval number MRCZA/2099, approved on 11 January 2019.
The permission to collect data was sought from Masvingo Provincial Medical Director and Masvingo District Medical Officer respectively.
A written consent was obtained from all participants prior to each interview session.
All the participants were assured that they can withdraw from the process whenever they wanted with no disadvantage to their care.
Privacy and confidentiality were maintained throughout the study process. Measures to ensure confidentiality where clients were told that no information shall be shared to other people and privacy were carried out.
RESULTS
Full vaccination coverage rate in Masvingo district
A total of 354 caregivers and their children participated in this study. The full vaccination rate among children aged 12 to 23 months in Masvingo District was found to be 89.3% (316). The full vaccination coverage rate by vaccination card was 88.1% (312) (Table 1).
| Variable (n=354) | Full immunisation status | No vs Yes
p-value (test) |
|
| No (%) | Yes (%) | ||
| Possession of a vaccination card
No Yes- card not seen Yes- card seen |
10 (26.3) 7 (18.4) 21 (55.3) |
4 (1.3) 5 (1.6) 307 (97.2) |
<0.001* (F) |
| Ever had a vaccination card
Yes No |
26 (68.4) 12 (31.6) |
316 (100.0) 0 (0.0) |
<0.001* (F) |
| *=significant test, F= Fisher’s exact test | |||
Table 1. Presumed factors associated with vaccination coverage rates
Out of 37 caregivers whose children missed one or more vaccines, the majority 15 (28%) cited
religious reasons, long walking distance to the vaccination site 11 (20%), and unavailability of the vaccine 10 (19%) as the major causes of missing the vaccines.
Fear of side effects and inconvenience of vaccination time contributed 11 and 7 percent respectively. Other reasons cited were mobility to neighboring countries in search of greener pastures (15%).
Summary of reasons for missing any vaccines are presented graphical on figure—below.
Figure 1. Reasons for missing any vaccine among 12-23 months age group in Masvingo district
Socio-demographic characteristics of the study participants
Of the 354 children aged 12 to 23 months included in the study, 152 (42.9%) were males and 202 (57.1%) were females. The mean age was 16.6 months (SD = 0.17). Most (66.9%) of the children were of the 1st-2nd birth order, 27.2% (96) were of the 3rd-4th birth order, and 5.9% (21) were of the 5th birth order or higher. The majority, 73.4%, lived in rural areas, while 26.6% resided in urban areas.
The majority of children, both fully immunized and not, were in the 16–20-month age group. Among those not fully immunized, 55.2% were males. About 84% of the children not fully immunized lived in rural areas and were mainly of the 3rd-4th birth order.
The majority of caregivers in both groups were aged 18-24 years and were married: 92.1% in the
not fully immunized group and 94.0% in the fully immunized group. There was a statistically significant association between caregivers’ highest level of education and the child’s immunization status (p<0.001). Most caregivers in both groups were not employed outside the home.
Regarding household expenditure, the majority of those with not fully immunized children spent
less than 50 USD per month (84.2%), whereas the majority of those with fully immunized children spent 50-500 USD per month. Most children not fully immunized (78.9%) belonged to apostolic religious groups, while the majority of fully immunized children (88.6%) were non-apostolic. There was a statistically significant association between immunization status and religion (P<0.001). Additionally, the majority of caregivers with not fully immunized children were non-professional health workers, compared to 56.6% of caregivers with fully immunized children who were professionals.
Tables 2 and Table 3 below present the socio-demographic characteristics of the study participants by immunization status.
| Variable (n=354) | Full immunisation status | No vs Yes
p-value (test) |
|
| No | Yes | ||
| Child’s age group in months
12 – 15 16 – 20 21 – 23 |
14 (36.8) 15 (39.5) 9 (23.7) |
129 (40.8) 146 (46.2) 41 (12.9) |
0.20 (C) |
| Sex
Male Female |
21(55.2) 17 (44.8) |
131(41.5) 185 (58.5) |
0.10 (C) |
| Residence
Rural Urban |
32 (84.2) 6 (15.8) |
228 (72.2) 88 (27.8) |
0.11 (C) |
| Child’s birth order
1st-2nd 3rd-4th 5th and above |
13 (34.2) 19 (50.0) 6 (15.8) |
224 (70.9) 77 (24.4) 15 (4.7) |
<0.001* (C) |
| Maternal/caregiver age group in years
Less than 18 18 – 24 25 – 40 40+ |
2 (5.3) 21 (55.2) 14 (36.8) 1 (2.6) |
8 (2.5) 179 (56.6) 124 (39.2) 5 (1.6) |
0.79 (F) |
| Marital status
Married Never married |
35 (92.1) 3 (7.9) |
297 (94.0) 19 (6.0) |
0.65 (F) |
| Mothers’ Highest level of education
Primary Secondary Tertiary |
22 (57.9) 16 (42.1) 0 (0.0) |
47 (14.9) 238 (75.3) 31(9.8) |
<0.001* (F) |
| *=significant test; C=chi-square test; F= Fisher’s exact test | |||
Table 2. Socio-demographic characteristics of participants by immunisation status.
| Variable (n=354) | Full immunisation status | No vs Yes
p-value (test) |
|
| No | Yes | ||
| Work outside home
Yes No |
1 (2.6) 37 (97.4) |
53 (16.8) 261(82.6) |
0.021* (C) |
| Household expenditure in USD
Less than $50 $50-500 Above $500 |
32 (84.2) 6 (15.8) 0 (0.0) |
65 (20.6) 243 (76.9) 8 (2.5) |
<0.0001* (F) |
| Religion
Apostolic Non-Apostolic |
30 (78.9) 8 (2.1) |
36 (11.4) 280 (88.6) |
<0.0001* (C) |
| Occupation
Professional Non-professional |
1 (14.3) 6 (85.7) |
30 (56.6) 23 (43.3) |
0.049* (F) |
| *=significant test; C=chi-square test; F= Fisher’s exact test | |||
Table 3. Socio-demographic characteristics of participants by immunisation status
Health services accessibility and utilization
Regarding the distance from the health facility, a greater proportion (55.3%) of children who were
not fully immunized lived more than 10 km from the nearest facility, whereas the majority (58.2%) of those fully immunized lived within 5 km of the nearest clinic. The association between distance from the health facility and immunization status was very significant (P<0.001). The majority of caregivers in both groups perceived that the waiting time at the health facility was too long, and there was a significant association between immunization status and perceived waiting time at the health facility (P<0.001). All children who were fully immunized had caregivers who had attended ANC, and the association between ANC attendance and immunization status was very significant (P<0.001). Mothers who had attended more than four ANC visits were least likely to have their children not fully immunized (P<0.001). The majority (98.1%) of caregivers whose children were fully immunized had delivered at a health institution, and the association between place of birth and immunization status was very significant (P<0.001). Women who had four PNC visits and had a discussion with nurses about vaccination were more likely to have their children vaccinated (P<0.001), (Table 4).
| Variable (n=354) | Full immunisation status | No vs Yes
p-value (test) |
|
| No | Yes | ||
| Distance from health facility
Less than 5km 5- 10km Above 10km |
7 (18.4) 10 (26.3) 21 (55.3) |
184 (58.2) 105 (33.2) 27 (8.5) |
<0.001* (C) |
| Waiting time at facility
Too long Reasonable |
20 (52.6) 18 (47.4) |
296 (93.7) 20 (6.3) |
<0.001*(C) |
| ANC attendance
Yes No |
31(81.6) 7 (18.4) |
316 (100.0) 0 (0.0) |
<0.001* (F) |
| Number of ANC visits
No visit 1-3 visits 4+ visits |
7 (18.4) 24 (63.2) 7 (18.4) |
0 (0.0) 86 (27.2) 230 (72.8) |
<0.001*(F) |
| Place of birth
Health institution Non-Health institution |
25 (65.8) 13 (34.2) |
310 (98.1) 6 (1.9) |
<0.001*(F) |
| Number of PNC visits attended
None Less than 4 4 visits |
7 (18.4) 26 (68.4) 5 (13.2) |
0 (0.0) 51 (16.1) 265 (83.9) |
<0.001*(F) |
| Discussion with nurse about vaccination
Yes N0 |
22 (57.9) 16 (42.1) |
305 (96.5) 11(3.5) |
<0.001*(C) |
| *=significant test; C=chi-square test; F= Fisher’s exact test | |||
Table 4. Summary of health services access and utilisation
Information, communication and knowledge
In relation to information and communication, results showed a statistical significant association between source of health information and immunisation status (P<0.001). The most frequent sources of information mentioned were health workers (79.9%), community leaders (92.9%), radios (42.1%) and Village Health Workers (30.8%). The results of the study revealed that the television and the newspapers were the least frequently used sources of information with 16.4% and 4% respectively. Regarding mothers’/ caregivers’ knowledge of schedule for immunization, the majority, 318 (89.8%) gave the correct timelines for all antigens while 36 (10.2%) had limited or no knowledge. Most of the respondents were well versed with vaccination schedule for BCG (95.4%) and Measles (94.4%). Despite these high knowledge levels, 14 (4%) indicated that they know nothing about the immunization schedule. Children born to mothers with partial knowledge on the vaccination schedule (71.1%) were less likely to be fully immunised whereas those born to fully knowledgeable mothers were more likely to be fully vaccinated (P<0.001) (Table 5).
| Variable (n=354) | Full immunisation status | No vs Yes
p-value (test) |
|
| No | Yes | ||
| Knowledge of vaccination schedule | |||
| OPV
No dose 1-2 doses 3 doses |
10 (26.3) 7 (18.4) 21 (55.3) |
4 (1.3) 5 (1.6) 307 (97.2) |
<0.001 (F) |
| PENTAVALENT
No dose 1-2 doses 3 doses |
10 (26.3) 8 (2.1) 20 (52.6) |
4 (1.3) 5 (1.6) 307 (97.2) |
<0.001* (F) |
| PCV
No dose 1-2 doses 3 doses |
10 (26.3) 11 (28.9) 17 (44.7) |
4 (1.3) 5 (1.6) 307 (97.2) |
<0.001*(F) |
| MEASLES
No dose 2 doses |
10 (26.3) 28 (73.7) |
7 (2.2) 310 (97.8) |
<0.001* (C) |
| Overall Knowledge level
Partial knowledge Full knowledge |
27 (71.1) 11 (28.9) |
9 (2.8) 307 (97.2) |
<0.001* (C) |
| *=significant test; C=chi-square test; F= Fisher’s exact test | |||
Table 5. Knowledge of vaccination schedule
Predictors of full vaccination coverage rate in Masvingo district
The study did a multivariate binary regression analysis to determine the predictors of full vaccination coverage rate in Masvingo district. All factors that had a statistical significant association with immunisation status were controlled for and these included birth order, mothers’ level of education, spouse’s level of education, work outside home, household expenditure per month, religion, having a vaccination card, distance to the clinic, time to reach health facility, waiting time at outreach and overall knowledge level on immunisation schedule. Only household expenditure per month (AOR=18.77, 95% CI = 3.13-11.21), having a vaccination card (AOR=11.78, 95% CI = 1.03-13.41) and overall knowledge on vaccination schedule (AOR=10.01,
95% CI = 2.32-43.25) were statistically significant predictors of full vaccination coverage rates
(Table 6).
| Immunisation status and: | Coefficient | Adjusted Odds ratio (AOR) | AOR CI at 95% | p-value |
| Birth order | 1.15 | 2.14 | 0.58 – 7.84 | 0.25 |
| Mother’s level of education | -0.05 | 0.96 | 0.17 – 5.33 | 0.96 |
| Spouse’s level of education | 1.08 | 2.64 | 0.46 – 15.30 | 0.28 |
| Work outside home | 1.92 | 11.91 | 0.95 – 14.90 | 0.051 |
| HH expenditure per month | 3.21 | 18.77 | 3.13 – 11.21 | 0.001* |
| Religion | 1.66 | 4.92 | 0.75 – 32.47 | 0.098 |
| Having a vaccination card | 1.99 | 11.78 | 1.03 – 13.41 | 0.047* |
| Distance to the clinic | -0.71 | 0.09 | 0.01 – 68.56 | 0.48 |
| Time to reach clinic | 0.82 | 16.06 | 0.02 – 12.56 | 0.41 |
| Waiting time at outreach | 0.86 | 2.46 | 0.32 – 19.04 | 0.39 |
| Overall knowledge on vaccination | 3.09 | 10.01 | 2.32 – 43.25 | 0.002* |
| * =significant test | ||||
Table 6. Predictors of full vaccination coverage rate in Masvingo district.
DISCUSSION
Full vaccination coverage rates
Based on the results of this study, full vaccination coverage by both card and mother’s recall was found to be 89.5%. This coverage is much higher compared to the provincial coverage of 78.1% [5], 65.4% [7], 60.3% [6], and 85% [10]. The finding was also higher than the 64% rate that had been reported in the previous 2011 ZDHS report [11]. These variances may be attributed to different methods used, areas covered, data quality issues, and denominator differences. Children with vaccination cards were more likely to be fully vaccinated (P<0.001).
In line with Meleko’s finding in 2015, this study established that more children (82.6%) with vaccination records/cards were fully vaccinated compared to those without [12]. Similar studies conducted in Ghana, Bangladesh, and India after the peak of the COVID-19 pandemic reported full vaccination coverage rates for children 12-23 months that ranged from 67% to 88% [13-15]. This suggests that vaccination cards, which contain vital information such as milestones and vaccination schedules, act as reminders to parents. Low vaccination among those without cards may be attributed to mothers’/caregivers’ recall bias. Similar to previous studies [7, 12], this study revealed variations in antigens given at the same period, such as OPV 3 and DTP 3. These variations suggest missed opportunities due to stock-outs, poor screening, and data quality issues. Policymakers should ensure and monitor that vaccination cards are distributed freely, reaching even the remotest mother-child pairs to promote high full vaccination coverage rates in Masvingo.
Socio-Demographic Characteristics of the Study Participants
This study assessed the association of full vaccination with the index child’s sex, age, birth order, and place of residence. No evidence suggested that the child’s sex influenced vaccination status, consistent with findings from ZDHS of 2015, Mukungwa in 2015, and studies in Ethiopia and Indonesia [6-7]. However, birth order was a significant predictor; higher birth orders were associated with lower vaccination rates, as seen in previous studies. This trend may reflect decreased enthusiasm and increased resource competition with higher birth orders.
Place of residence also showed a significant association with full vaccination. Contrary to Mukungwa’s findings, this study found that children in rural areas were more likely to be fully vaccinated than those in urban areas (OR=0.48, 95% CI = 0.01-0.93). This may be due to the increased number of urban poor who cannot afford health services.
Factors significantly associated with full vaccination status included maternal age, marital status, mother’s education, spouse’s education, household expenditure, and religion. Marital status was a key determinant, with married mothers more likely to fully vaccinate their children (OR=1.33, 95% CI = 1.12-5.56), possibly due to additional resources and support from spouses. Similar studies in low to medium income countries showed the same trends even after the Covid-19 pandemic [13-15].
Education level also positively influenced vaccination rates. Educated mothers are more likely to seek health services, though other factors still play a role. Fathers’ education similarly impacted vaccination status, likely due to their ability to make informed health decisions. This aligns with findings by Meleko and others, which reported that children of literate fathers were 2.42 times more likely to be fully vaccinated [12].
Employment type significantly affected vaccination rates. Children of non-professional workers were less likely to be fully vaccinated compared to those of professional health workers. Monthly household expenditure also correlated with vaccination status; children in households spending less than $50 per month were less likely to be fully vaccinated. This underscores the need for community health insurance models to enhance equity in health service access.
Economic status, measured by household expenditure, was another predictor of full vaccination. Wealthier families exhibited better health-seeking behaviors, despite free vaccination services in Zimbabwe, suggesting that indirect costs like transportation influence vaccination decisions.
Religious affiliation also impacted vaccination coverage. The study found that 54.5% of children from apostolic sect families were partially or unvaccinated, compared to 97% from other Christian denominations. Despite efforts to raise health awareness among apostolic sect members, some still prefer faith healing over modern medical interventions, confirming Mukungwa’s findings [12].
Health Service Accessibility and Utilization
Distance to the nearest health facility, waiting time, place of delivery, antenatal care (ANC) and postnatal care (PNC) clinic services utilization, and having a vaccination card were found to influence the likelihood of full vaccination. Children born to mothers who walk more than 10 km to a health facility are 13 times less likely to be fully vaccinated than those who walk less than 10 km (OR=13.22, 95% CI = 5.77-17.01). This finding aligns with studies by UNICEF, Mukungwa, and Legesse and Dechasa, which identified long walking distances as a barrier to immunization [7, 16-17].
Contrary to Ayano (2015), this study found no significant association between travel time and full vaccination status [18]. However, mothers who deemed waiting times reasonable were 13 times more likely to fully immunize their children (OR=13.32). This result highlights the importance of reducing wait times, particularly during busy seasons.
Antenatal care utilization strongly correlates with full vaccination status. Mothers who attended at least four ANC visits were more likely to fully vaccinate their children, consistent with studies by Mukungwa, Sunguti et al., and Herliana and Douiri [7,12,19]. The World Health Organization recommends at least four ANC visits, during which mothers receive education on child care and immunization. This study found that 97% of women who attended four or more ANC visits fully vaccinated their children, compared to 73.7% who attended fewer visits.
Place of delivery also significantly influenced full vaccination status. Mothers who gave birth at health facilities were 27 times more likely to vaccinate their children (OR=26.67; 95% CI: 16.74-36.55). This finding aligns with previous studies and highlights the importance of health facility deliveries, where vaccination is initiated before discharge and mothers receive guidance on future vaccinations.
Postnatal care follow-up visits were another strong predictor of full vaccination. This study revealed that 98% of mothers who attended the recommended four PNC visits fully vaccinated their children, compared to 60.7% among those who attended fewer visits. PNC clinics provide opportunities for health professionals to administer due and overdue vaccines and discuss child health issues.
Discussions about vaccination with health professionals during pregnancy significantly influenced full vaccination status. Children of mothers who had such discussions were more likely to be fully vaccinated, consistent with findings by from similar studies [13-15,17]. These discussions positively impact mothers’ health-seeking behaviors, leading to increased demand and utilization of
immunization services and higher full vaccination coverage for children aged 12-23 months.
Communication, Information, and Knowledge
Though there was a significant association between the source of information and full vaccination,
the majority (79.9%) of mothers and caregivers received information about immunization from health workers and community leaders. This is likely due to the fact that most (73.4%) study participants were from rural areas where access to electronic and print media was limited. The study revealed a significant association between mothers’ and caregivers’ knowledge about the vaccination schedule and the full vaccination status of the index child. This result is consistent with previous studies which found that knowledge about vaccination was a significant determinant of the full vaccination status of index children [12,18]. It also aligns with findings by Xeuatvongsa et al., which showed that low full vaccination coverage was mainly due to limited knowledge about immunization [20].
Predictors of full immunisation coverage
After controlling for birth order, mothers’ level of education, spouse’s level of education, work outside the home, household expenditure per month, religion, having a vaccination card, distance to the clinic, time to reach the health facility, waiting time at outreach, and overall knowledge level on the immunisation schedule, only household expenditure per month (AOR=18.77, 95% CI = 3.13–11.21), having a vaccination card (AOR=11.78, 95% CI = 1.03–13.41), and overall knowledge of the vaccination schedule (AOR=10.01, 95% CI = 2.32–43.25) were statistically significant predictors of full vaccination coverage rates. These factors should be fully addressed in the community health strategy to improve full immunisation coverage rates in Masvingo district.
These results are crucial for nursing. Understanding these factors enables nurses to identify barriers
to immunization, which is essential for preventing childhood diseases. Enhanced vaccination
coverage ensures community health, reduces morbidity and mortality rates, and lowers healthcare costs by preventing outbreaks. Moreover, insights from this study can guide nurses in developing targeted interventions, educational campaigns, and policy recommendations to improve vaccination rates, ultimately leading to better health outcomes for children and the broader community. This aligns with nursing’s core mission of promoting public health and disease prevention.
Limitations
In the absence of vaccination records, information about the index child’s vaccination status was obtained from the mothers’ or caregivers’ recall. Thus, the accuracy of the information relied on the mothers’ or caregivers’ ability to precisely remember the vaccination period and antigens given to the child. Additionally, the accuracy depended on the mothers’ or caregivers’ honesty. This information is subject to recall bias. This study was a cross-sectional survey and could only assess the association between various risk factors and full vaccination coverage but not causal inferences. Similarly, there are chances that the coverage rates could have changed significantly between the time the study was conducted and now since in between the Covid-19 pandemic struck and pandemics have always been associated with reduction in vaccination coverage rates.
Strength
One person collected the data for this study, eliminating the chances of inter-observer biases. Most of the mothers and caregivers had vaccination cards available, enhancing the accuracy of the data.
CONCLUSION
This study assessed factors linked to low full vaccination coverage among children aged 12-23 months in Masvingo district, finding a coverage rate of 89.5%, higher than previous estimates but still below GVAP targets for some vaccines like measles. Socio-demographic factors such as birth order, place of residence, family and maternal factors, and household expenditure significantly influenced vaccination. Accessibility to health facilities, waiting times, antenatal and postnatal care utilization, and possession of a vaccination card were also crucial. Effective outreach and integrated approaches, including educational programs and promoting maternal and child health activities, are essential to improving vaccination coverage and should be prioritized in nursing strategic planning for effective community mobilization. Health system strengthening measures should also consider strengthening the supply chain for vaccines and effective distribution strategies to improve access to vaccination services. It is crucial that community nursing interventions employ innovative approaches to ensure saturation coverage and easy accessibility of maternal and child services to address barriers to full coverage.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Conflict of interest
The authors report no conflict of interest.
Authors’ contribution
Nomore Nyengerai: Development of the original draft; Maxwell Mhlanga: Review of the manuscript, data analysis and discussion.
Acknowledgements
We would want to acknowledge Masvingo Provincial Medical Directorate for allowing us to carry out our research at their institution.
REFERENCES
- WHO and UNICEF. (2018) Progress and Challenges of Achieving Universal Immunisation Coverage, 2017 WHO/UNICEF Estimates of National Immunisation Coverage, Data. Available online: https://www.who.int/teams/immunization-vaccines-and-biologicals/immunization-analysis-and-insights/global-monitoring/immunization-coverage/who-unicef-estimates-of-national-immunization-coverage. Accessed on 19 February 2019- WHO, Geneva.
- (2018) Immunisation Coverage. Available online: http://www.who.int/news-room/fact-sheets/detail/immunization-coverage ( Accessed on 14 October 2019)
- Ministry of Health and Child Care. (2018): Zimbabwe Expanded Programme on Immunisation- revised Policy Document, Ministry of Health and Child Care: Harare. Available on: https://extranet.who.int/countryplanningcycles/sites/default/files/planning_cycle_repository/zimbabwe/zimbabwe_epi_cmyp_2015 – 2019_0.pdf (Accessed on 10 January 2021.
- Ministry of Health and Child Care, (2015). Report on Evaluation of Coverage Achieved during Zimbabwe Measles/Rubella and Vitamin A Catch Up Campaign combined with Assessment of Routine Immunization: Part II Coverage Survey: Routine Immunization, December 2015, MoHCC National Expanded Programme on Immunization: Harare. Available online: https://www.unicef.org/zimbabwe/media/356/file/Factors%20Influencing%20Vaccine%20Hesitancy%20and%20Immunization%20Coverage%20in%20Zimbabwe.pdf. Accessed on 13 October 2018).
- Zimbabwe National Statistical Agency, (2015). Multiple Indicator Cluster Survey 2014, Harare: ZIMSTAT. Available online: https://microdata.worldbank.org/index.php/catalog/2527. Accessed on 13 October 2018).
- ZIMSTAT & ICF International. (2016). Zimbabwe Demographic and Health Survey: Key Indicators, Rockville, Maryland, USA: ZIMSTAT and ICF International. Available online: https://www.dhsprogram.com/pubs/pdf/FR322/FR322.pdf. Accessed on 18 October 2018.
- Mukungwa, T. (2015). Factors Associated with Full Immunization Coverage amongst Children aged 12-23 Months in Zimbabwe, African Population Studies 29(2): 1761-1774. DOI:https://doi.org/10.11564/29-2-745
- Ministry of Health and Child Care. (2014) Zimbabwe Expanded Program on Immunization Comprehensive Multi-Year Plan 2015-2019, Government of Zimbabwe: Harare, p4. Available online: https://www.sida.se/en/publications/expanded-programme-on-immunization-in-zimbabwe. Accessed on 21 October 2018.
- (2015) Vaccination Surveys Cluster Surveys: Reference Manual, Version 3 Working Draft, updated July 2015. Available online: https://www.technet-21.org/en/topics/data/vaccination-coverage-surveys-technical-resources. Access on 15 October 2018.
- Zimbabwe National Statistics Agency. (2012) Zimbabwe Population Census 2012: National Report, ZIMSTAT, Harare. Available online: https://www.dhsprogram.com/pubs/pdf/FR322/FR322.pdf. Accessed on 18 October 2018.
- Kriss JL, Goodson J, Machekanyanga Z, Shibeshi ME, Daniel F, Masresha B, Kaiser R. Vaccine receipt and vaccine card availability among children of the apostolic faith: analysis from the 2010-2011 Zimbabwe demographic and health survey. Pan Afr Med J. 2016 May 11;24:47. DOI: 10.11604/pamj.2016.24.47.8663.
- Meleko, A., Geremew, M. & Birhanu, F. (2017) Assessment of Child Immunization Coverage and Associated Factors with Full Vaccination among Children Aged 12–23 Months at Mizan. DOI: 10.1155/2017/7976587
- Akanpaabadai EA, Adiak AA, Nukpezah RN, Adokiya MN, Adjei SE, Boah M. Population-based cross-sectional study of factors influencing full vaccination status of children aged 12- 23 months in a rural district of the Upper East Region, Ghana. BMC Pediatr. 2024 Mar 8;24(1):168. DOI: 10.1186/s12887-024-04662-w.
- Khanam M, Jahan NA. Determinants of Full Vaccination Coverage among Children Aged 12-23 Months in Bangladesh: A Comparison between High- and Low-Performing Divisions. Int J Pediatr. 2024 May 15;2024:7787593. DOI: 10.1155/2024/7787593.
- Islam T, Mandal S, Chouhan P. Influence of socio-demographic factors on coverage of full vaccination among children aged 12-23 months: a study in Indian context (2015-2016). Hum Vaccin Immunother. 2021 Dec 2;17(12):5226-5234. DOI: 10.1080/21645515.2021.1977056.
- Sunguti, J., Neave, P. & Taylor, S. (2016). Family factors associated with immunization uptake in children aged between twelve and fifty-nine months: a household survey in Kakamega Central district, Western Kenya Healthcare in Low-resource Settings 2016. DOI :10.4081/hls.2016.5447
- Phukan, R., Barman, M. and Mahanta, J. (2008). Factors Associated with Immunization Coverage of Children in Assam, India: Journal of Tropical Pediatrics Vol. 55, No. 4. DOI: 10.1093/tropej/fmn025
- Legesse, E. & Dechasa, W. (2015). An assessment of child immunization coverage and its determinants in Sinana District, Southeast Ethiopia BMC Pediatrics (2015) 15:31. DOI: https://doi.org/10.1186/s12887-015-0345-4
- Ayano, B. (2015) Factors Affecting Fully Immunization Status of Children Aged 12- 23 Months in Hosanna Town, South Ethiopia. J Preg Child Health 2: DOI :10.4172/2376-127X.1000185
- Herliana, P., & Douiri, A. (2017). Determinants of immunisation coverage of children aged 12–59 months in Indonesia: a cross-sectional study. BMJ open, 7(12), https://bmjopen.bmj.com/content/7/12/e015790
- Xeuatvongsa, A., Hachiya, M., Miyano, S., Mizoue, T. and Kitamura, T. (2017) Determination of factors affecting the vaccination status of children aged 12–35 months in Lao People’s Democratic Republic.(Online). DOI: 10.1016/j.heliyon.2017.e00265
- Aman Town, Bench Maji Zone, Southwest Ethiopia Hindawi International Journal of Pediatrics Volume 2017. DOI: https://doi.org/10.1155/2017/7976587
- Gelaye SS, Yenit MK, Baraki AG. Rural Vaccination Coverage Among Children Aged 12-23 Months Was Higher Than the Urban Counterparts: A Comparative Cross-Sectional Study in Pawi District, Ethiopia. Pediatric Health Med Ther. 2021 Mar 19;12:119-127. DOI: 10.2147/PHMT.S299064.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
