La Ode Alifariki1*, Sri Susanty2, Heriviyatno Julika Siagian3, Daryono Daryono4
1Department of Epidemiology, Medical School, Halu Oleo University, Kendari, Indonesia
2Department of Nursing, Medical School, Halu Oleo University, Kendari, Indonesia
3Department of Medical Surgical Nursing, College of Science and Technology, Sembilanbelas November University, Kolaka, Indonesia
4Nursing Department, Health Polytechnic Ministry of Health Jambi, Indonesia
Corresponding author: La Ode Alifariki, Kampus Hijau Bumi Tridharma, Anduonohu, Kec. Kambu, Kota Kendari, Sulawesi Tenggara 93232, Indonesia. Orcid: https://orcid.org/0000-0003-4120-7465. Email: ners_riki@yahoo.co.id
Cite this article
ABSTRACT
Background & Aim: The body of literature on QoL has steadily grown over recent years, spurred by the promotion of research and the cross-cultural adaptation and validation of assessment instruments in different languages. However, limited information exists on the most commonly used instruments against the backdrop of current demographic and epidemiological trends. The aim this study to evaluate QoL assessment instruments used in hypertensive patients.
Methods & Materials: This review was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. Databases used including Sciencedirect, Cochrane library, Pubmed, Proquest, and the Wiley Online Library, utilizing keywords that are tailored to the Mesh Terms. Systolic Blood Pressure (SBP) value at least 140 mmHg and/or Diastolic Blood Pressure (DBP) value at least 90 mmHg, or the patient had a history of hypertension and was administered with antihypertensive drugs, English version, observational studies that presented Health-Related Quality of Life (HRQoL) scores in hypertensive individuals using varied assessment tools (WHOQoL BREF, SF-36, MINICHAL, etc) where these tools assess the situation of the patient’s quality of life based on the domain of life (physiological, psychological, social interaction, etc.) in the form of numbers, and published between January 2000 to December 2021 were inclusion criteria of the study. Relevant studies were read critically, analyzed, and described in detail. Survey data were processed in the form of comparative tables.
Results: A total of 2,287,348 references were found through databases, and for the final screening, twenty-two articles were finally designated as articles to be reviewed. The SF-36 (SF-8, SF-12), WHOQoL BREF, MINICHAL, and PECVEC are assessment tools used in the studies included in this review. The SF-36 was the most widely used tool in the studies included in this review. One of the critical domains to assess is spiritual, where none of the studies included this domain.
Conclusion: The SF-36 is the most frequently used assessment tool. However, this form is a general form that is not explicitly intended to assess the quality of life in hypertension only. The spiritual domain is one of the important items that need to be included in the QoL assessment tool.
Keyword: Quality of life, assessment tool, hypertension
INTRODUCTION
Hypertension is one of the most common chronic diseases that threaten the health of human beings. Poor adherence to treatment and low control rate of hypertension are the risk factors for coronary heart disease, stroke, and renal insufficiency, causing a great disease burden worldwide [1–3]. For a long time, the evaluation for the health condition of hypertension patients is usually based on the control of patients’ blood pressure (BP) or the degree of damage to the target organ [4–6]. As the medical model has changed from the biological medical model to the biological–psychosocial medical model, it is difficult to comprehensively and accurately assess chronic diseases (such as hypertension) in terms of incidence, death rate, cure rate, and life expectancy. Thus, the health-related quality of life (HRQoL) has gradually arisen with great attention in the world [7–9].
Quality of Life (QoL) is a broad ranging concept affected in a complex way by the person’s physical health, psychological state, level of independence, social relationships, personal beliefs and their relationship to salient features of their environment[10]. Health related QoL (HRQoL) is emerging as an important outcome in hypertension and can be adversely affected by hypertension itself and side-effects of antihypertensive drugs. However reports of HRQoL among hypertensive individuals have been conflicting, with some studies finding worse HRQoL among hypertensive compared to the general population, while Moum T et al reported no impact of hypertension on HRQoL in some / all domains. There is a paucity of studies reporting QoL in Indian hypertensive patients [8,11,12]. Assessing QoL is of essence, as this concept serves as an indicator in clinical trials for specific diseases, assesses the physical and psychosocial impact that the disorders may have on affected individuals, allowing a better knowledge about the patient and their adaptation to their unhealthy condition. Roca-Cusachs et al reported that hypertensive patients had a significant reduction in QoL compared to normotensive patient [13,14].
Scales measuring HRQoL of hypertensive patients include EuroQOL five-dimension questionnaire, WHO QoL-100 (the well-being questionnaire), SF-36 (the Medical Outcomes 36 Item Short-form Health Survey), and so on. SF-36 is the most widely used scale for assessing HRQoL, which has high reliability. In addition, SF-12, the shorter form of SF-36, is an effective alternative to the SF-36 in hypertension. Although many articles showed a significantly lower HRQoL of hypertension patients, some still present no difference in many domains [7,15,16].
Another quality of life assessment form that is starting to be widely used is MINICHAL. MINICHAL, an assessment tool focusing on people with hypertension, was formed in 2002 by a group from Spain [13], and it was shown to be effective in the measurement of HRQoL of elderly people with hypertension linked to the supplementary health sector and evidenced a lower impairment in HRQoL among the elderly practicing physical activity [17].
The body of literature on QoL has steadily grown over recent years, spurred by the promotion of research and the cross-cultural adaptation and validation of assessment instruments in different languages. However, limited information exists on the most commonly used instruments against the backdrop of current demographic and epidemiological trends. In light of the above, the aim of this study was to evaluate QoL assessment instruments used in hypertensive patients.
METHODS
Review Protocol
This integrative review was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement [18]. The current study tries to evaluate QoL assessment instruments used in hypertensive patients from articles that have been published in the period January 2000 to December 2021.
Searching strategy
Relevant articles were searched and collected using Sciencedirect, Cochrane library, Pubmed, Proquest, and the Wiley Online Library, with a publication time between 2000 and 2021. The search keywords were adjusted according to the Mesh terms for health research. The keywords used vary, depending on the search engine used. In general, the keywords focus on Quality of life OR HRQoL AND Hypertension AND Measurement AND Assessment tool OR WHOQoL OR SF-36 OR MINICHAL. Summary of keywords used in each databases are reported in table 1.
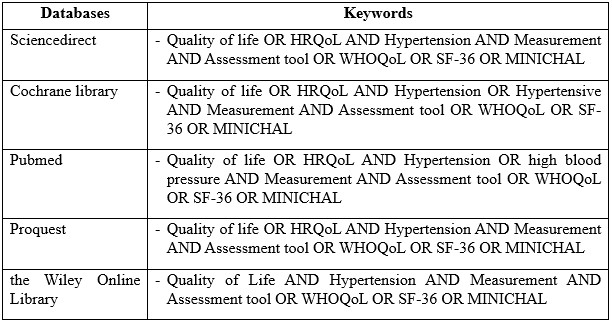
Table 1. Search string in databases
Study eligibility
Inclusion criteria: Hypertension is defined as Systolic Blood Pressure value at least 140 mmHg and/or Diastolic Blood Pressure value at least 90 mmHg, or the patient had a history of hypertension and was administered with antihypertensive drugs. Language was restricted to English. All observational studies that presented Health Related Quality of Life (HRQoL) scores in hypertensive individuals using varied assessment tools (WHOQoL BREF, SF-36, MINICHAL, etc) where these tools assess the situation of the patient’s quality of life based on the domain of life (physiological, psychological, social interaction, etc.) in the form of numbers, published between January 2000 to December 2021. In addition, we manually searched the cited reference of potentially eligible articles and published reviews.
Studies were excluded if they were carried out in special groups (armies, a pasturing area, etc.) and cannot represent the general population; they compared HRQoL of individuals randomized to different antihypertensive agents or placebo or other interventions.
Study selection and data analyses
After a further authentication of the articles, cross sectional, and case-control study design were chosen for final analysis. Relevant studies were read critically, analyzed, and described in detail. The methodological quality of studies was evaluated using National Institute of Health (NIH) for observational cohort and cross sectional studies. The checklist has 14 questions including Q1: Was the research question or objective in this paper clearly stated?; Q2: Was the study population clearly specified and defined?; Q3: Was the participation rate of eligible persons at least 50%?; Q4: Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants?; Q5: Was a sample size justification, power description, or variance and effect estimates provided?; Q6: For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured?; Q7: Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed?; Q8: For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome?; Q9: Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants?; Q10: Was the exposure(s) assessed more than once over time?; Q11: Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants?; Q12: Were the outcome assessors blinded to the exposure status of participants?; Q13: Was loss to follow-up after baseline 20% or less?; Q14: Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)? relating to the research question, selection of study subjects, statistical analysis and measurement and selection of timeframe between exposure and outcome to see an effect. The quality grading of studies was done as Good (G) if the overall rating was at least 70%, Fair (F) if rating was at least 50% and poor (P) if the rating was less than 50% . The table assists in identifying the key characteristics of each study included in this review, with quality of life in patients with hypertension theme.
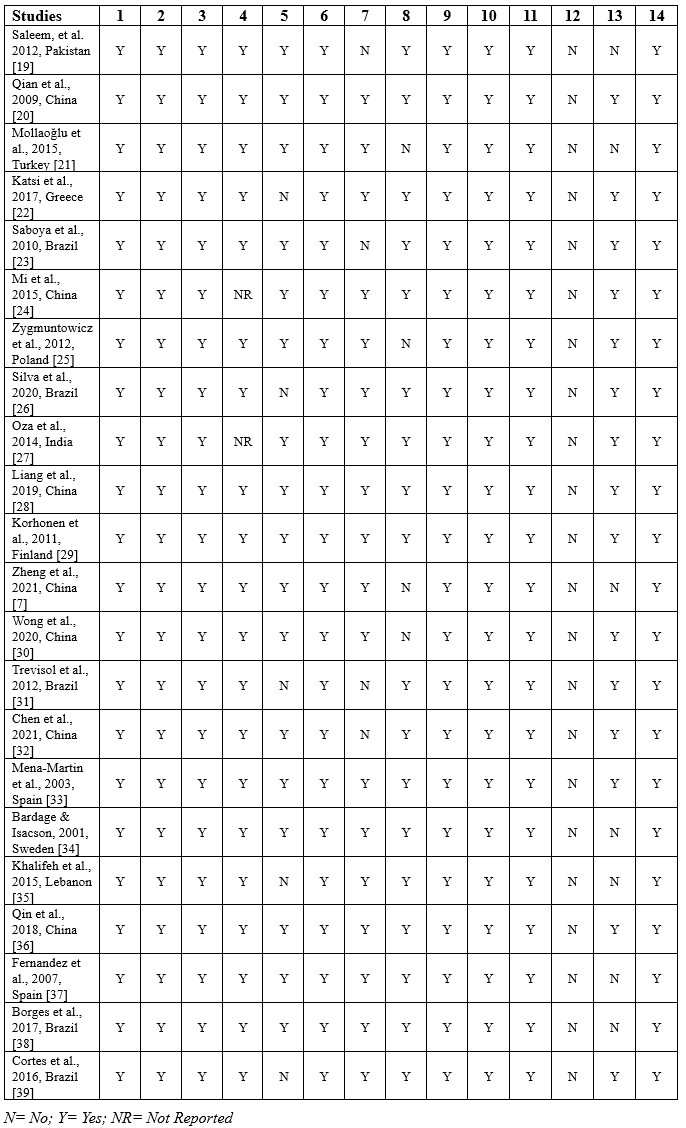
Table 2. Summary of quality assessment
RESULTS
Search Results
Combining the output of the searches in the various databases, a total of 2,287,348 references were found. After duplicates were removed, 1,918,891 potentially relevant references remained from the database searches. 1,918,854 articles removed by reasons of irrelevant, review/report, not full text, book chapter. 22 articles were finally designated as articles to be reviewed. The main focus of this integrative review is the evaluation of quality of life assessment tools used in hypertensive patients.
The authors developed tables for data analysis with the study design, participants characteristics including the number, assessment tools used, domain of measurements, measurement method, and the main results of Quality of Life assessment tools. PRISMA flow chart for study selection, can be seen in figure 1.

Figure 1. PRISMA flowchart for Study selection
Characteristics of the studies
The studies included in this review are from several countries globally, including China (n=7), Brazil (n=5), and one study each in Pakitan, Turkey, Greece, Lebanon, Sweden, Spain, Finland, and India. The study design used mainly was cross-sectional, which focused on the relationship between hypertension and the quality of life. The assessment tools used vary, including WHOQoL-BREF, SF-36, SF-12, SF-8, MINICHAL, and PECVEC. Several studies used a control group to compare the quality of life of people with hypertension with people who did not suffer from hypertension. Self-reported and face-to-face interviews measure the quality of life through a questionnaire format. Several studies included in this review also did not determine the degree of hypertension which was the inclusion criteria in the study conducted. Overall, 140 mmHg for systolic blood pressure is the standard for patients with hypertension.
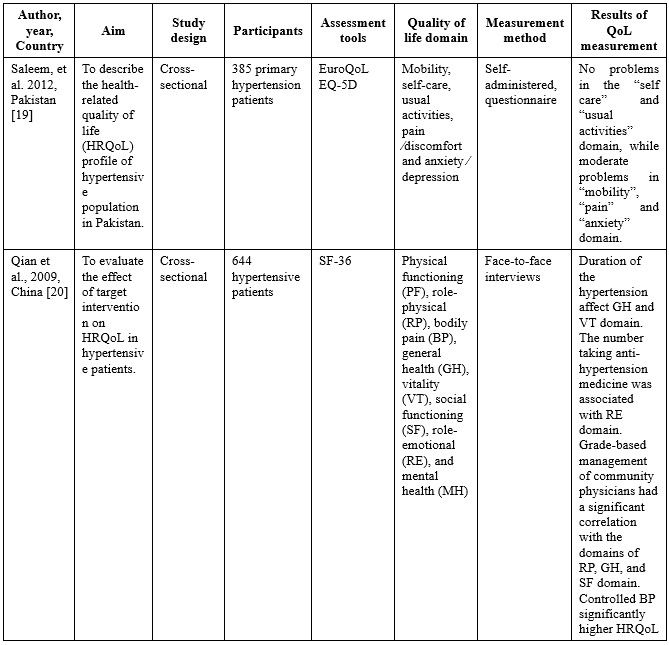
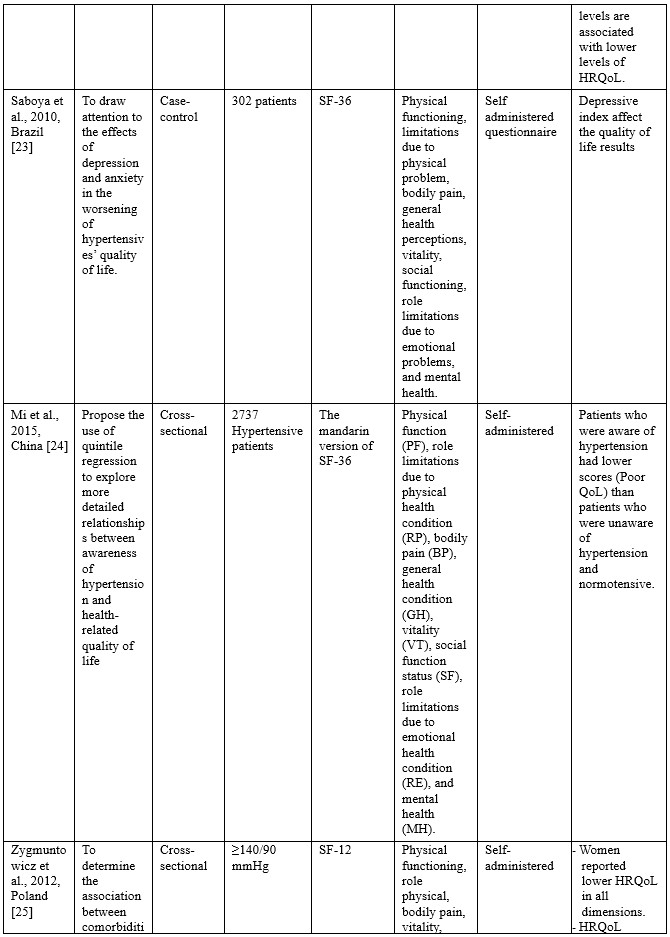
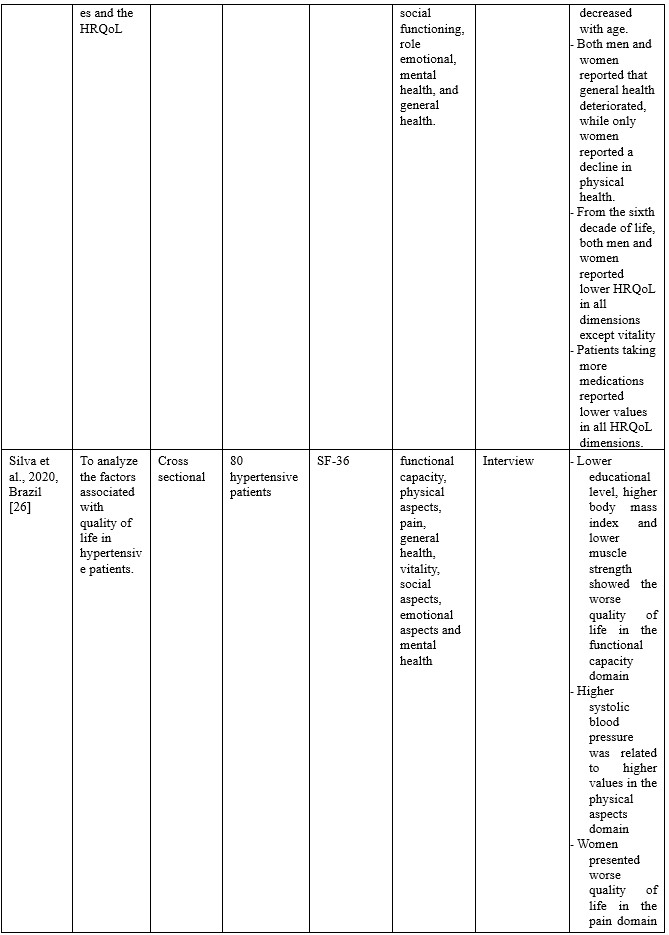
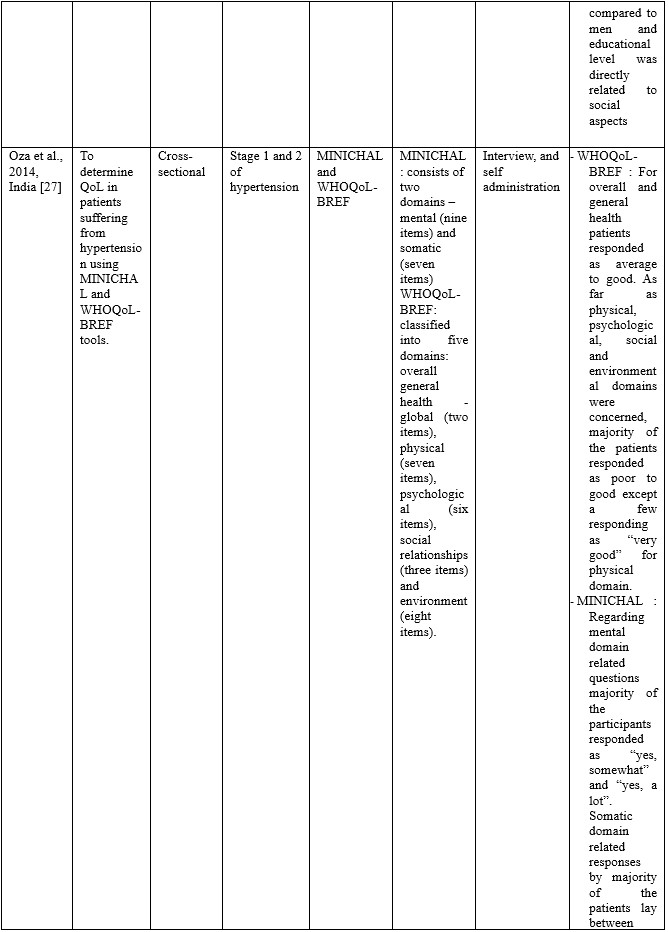
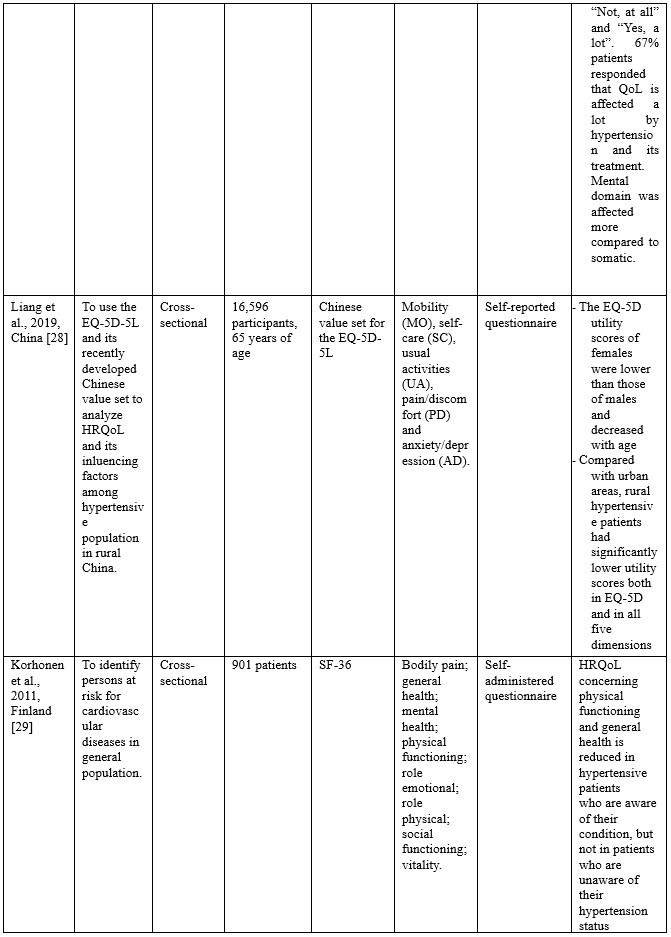

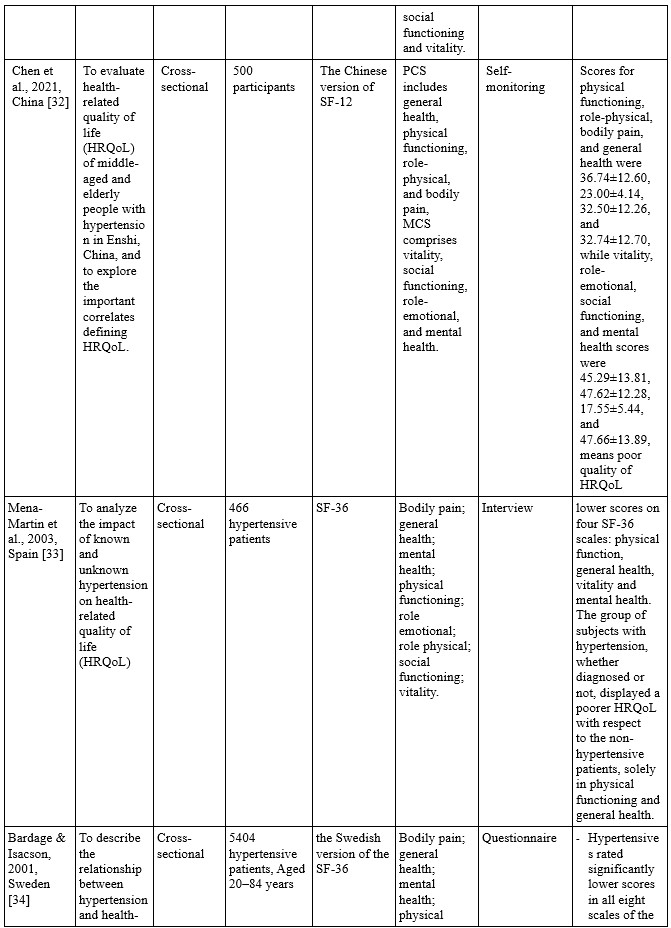
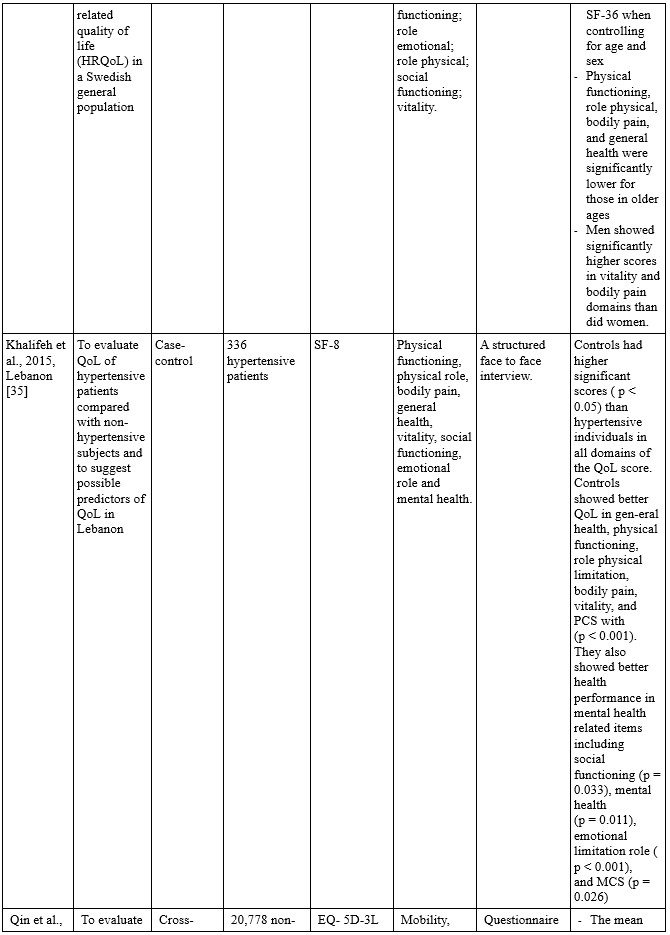

Table 3. Characteristics of the studies included
Quality of Life Domains
Based on the assessment tool used, the assessment domains for hypertension sufferers include general health, physical, psychological, social relationship, and environment (WHOQoL-BREF), mobility, self-care, usual activities, pain/discomfort, and anxiety/depression (EuroQoL EQ 5D), Physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional, and mental health (SF-36, SF-12, SF-8), mental, and somatic (MINICHAL), the physical, psychological, and social dimensions (PECVEC). Most studies conducted in non-English countries translate the assessment items into the language of each country to make it easier for participants to answer the question items in each assessment tool.
QoL measurement results
In general, the assessment results of the quality of life in patients with hypertension on all the assessment tools used show a low score, which means the quality of life is low. The results of the quality of life assessment based on each assessment tool can be described as follows:
In studies using the 5D EQ, the problems found in the quality of life domain include mobility, pain, anxiety [19], while other studies indicate a decrease in scores in all domains in the 5D EQ [7,28,30]. Meanwhile, for the study conducted by Qin et al. [36], which compared the quality of life between patients with hypertension and those without hypertension, it was found that only the pain/discomfort dimension showed a very significant difference in scores.
In the studies using SF-36, -12, and -8, it was found that the duration of suffering from hypertension affected general health and vitality dimensions. The amount of consumption of antihypertensive drugs is related to the role emotional dimension, and controlled blood pressure has a significantly better effect on the quality of life, especially in the domains of role-physical, social functioning, and role emotional [20]. One study revealed that physical health and mental health domains had a strong positive influence on adherence to hypertension therapy [21]. Studies in Greece revealed that women had lower BP, SF, RE, and VT scores. Increased age was independently associated with lower scores on PF and RE [22,25]. Saboya et al. [23] found that the depression index affects the quality of life outcomes. One study in China revealed that patients who were aware of hypertension had lower scores (Poor QoL) than patients who were unaware of hypertension and normotensive [24]. Lower educational level, higher body mass index, and lower muscle strength showed the worse quality of life in the functional capacity domain. Higher systolic blood pressure was related to higher values in the physical aspects domain. Women presented worse quality of life in the pain domain than men, and educational level was directly related to social aspects [26]. Decreases in physical functioning and general health scores occurred in hypertensive patients aware of their condition [29]. A study in Brazil found that patients with hypertension had a lower quality of life than normotensive participants in all measurement domains [31,32,34,35]. Another study in Spain noted that people with hypertension had a low quality of life, especially in physical function, general health, vitality, and mental health.
Another measurement used MINICHAL, which consists of two domains, namely mental state and somatic manifestations. Oza et al. [27] found that the mental domain had more impact than the somatic domain. Meanwhile, in a study in Brazil, it was found that women have a better quality of life compared to men in the mental state domain.
DISCUSSION
This integrative review was carried out as our first step in conducting future projects to measure the quality of life of people with hypertension. Differences in culture, race, economic situation, geographical location, and so on in the world underlie our thinking to explore the possibility of imbalances in the assessment tool used internationally and has been tested for validity. However, some of the literature in this study has modified the item assessment tool used primarily for language. We realize that it is not enough to generalize its reliability and feasibility, especially in Indonesia and other countries in the Asian continent, which has extreme contrasts in culture with countries on the continent of Europe, America, and others.
The WHOQoL-BREF is one of the most commonly used generic Quality of Life (QoL) questionnaire which was developed simultaneously across a broad range of member countries, assuring that it could be used more multi-culturally and multi-lingually than any other existing QoL tool. It emphasises subjective response rather than objective life condition, with assessment made over the preceding two weeks [25]. WHOQoL-BREF consists of four main domains including physical health, psychological, social relationship, and environment. The aspects included in these domains include the physical health domain consisting of Activities of daily living, Dependence on medicinal substances and medical aids, Energy and fatigue, Mobility, Pain and discomfort, Sleep and rest, and Work Capacity [40]. The psychological domain consists of Body image and appearance, Negative feelings, Positive feelings, Self-esteem, Spirituality / Religion / Personal beliefs, thinking, learning, memory, and concentration. The social relationship domain consists of Personal relationships, Social support, and Sexual activity. Domain environment consists of financial resources, Freedom, physical safety and security, health and social care: accessibility and quality, Home environment, Opportunities for acquiring new information and skills, Participation in and opportunities for recreation/leisure activities, Physical environment (pollution/noise/traffic/climate), and Transport [41,42].
The 3-level version of EQ-5D (EQ-5D-3L) was introduced in 1990 by the EuroQol Group. The EQ-5D-3L essentially consists of 2 pages: the EQ-5D descriptive system. The EQ-5D-3L descriptive system comprises the following five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each dimension has 3 levels: no problems, some problems, and extreme problems. The patient is asked to indicate his/her health state by ticking the box next to the most appropriate statement in each of the five dimensions. This decision results into a 1-digit number that expresses the level selected for that dimension. The digits for the five dimensions can be combined into a 5-digit number that describes the patient’s health state. The 5-level EQ-5D version (EQ-5D-5L) was introduced by the EuroQol Group in 2009 to improve the instrument’s sensitivity and to reduce ceiling effects, as compared to the EQ-5D-3L. The EQ-5D-5L essentially consists of 2 pages: the EQ-5D descriptive system. The descriptive system comprises five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each dimension has 5 levels: no problems, slight problems, moderate problems, severe problems and extreme problems. The patient is asked to indicate his/her health state by ticking the box next to the most appropriate statement in each of the five dimensions. This decision results in a 1-digit number that expresses the level selected for that dimension. The digits for the five dimensions can be combined into a 5-digit number that describes the patient’s health state [28,43,44].
The Short Form (SF) -36, -12, -8 is a health status profile originally designed to measure health status of patients and outcomes of patients. Health status could be compared between groups of patients by type of intervention, disease, or type of health insurance. The original target population was individuals living in the community. The SF-36 is used today in outpatient settings and with community-dwelling older adults. The 36 questions on the SF-36 are meant to reflect 8 domains of health, including physical functioning, physical role, pain, general health, vitality, social function, emotional role, and mental health. The categories of physical role and emotional role reflect performance at the activity and participation levels [45,46].
MINICHAL consists of the short version of Calidad de Vida em la Hipertensión Arterial (CHAL), developed and validated in Spain. This is a self-administered instrument comprised of 16 items divided into the Mental Status (1 to 10) and Somatic Manifestations (11 to 16) dimensions. The mental domain includes questions one to nine and score ranges from 0 to 27 points. The somatic domain includes questions 10 to 16 and score ranges from 0 to 21 points. Last question is related to the overall impact of hypertension on the QoL. The score scale is Likert scale with four possible answers (0 = No, not at all; 1 = yes, somewhat; 2 = yes, a lot; 3 = yes, very much). Total points range from 0 (best level of health) to 51 (worst level of health) [47,48].
PECVEC considers the physical, psychological and social dimensions of QoL. Patients performance and well-being are assessed in each dimension. The physical dimension is measured according to two scales: lists of symptoms (17 items) and physical functions (eight items). The psychological dimension is measured according to three scales: psychological function (eight items), positive state of mind (five items) and negative state of mind (eight items). The social dimension is measured according to two scales: social function (six items) and social well-being (five items). The items are Likert-scaled from 0 (worst) to 4 (best) [37,49].
Quality of life is a reflection of holistic aspects of human well-being. Holistic health care includes biological, psychological, sociological, and spiritual aspects, so to assess the quality of life of a person with hypertension, it is obligatory to fully represent the items from the holistic aspect of the assessment. Differences in culture, economic status, race, geographical situation make it difficult to generalize an assessment tool.
In the results of the QoL measurement, there are several differences in the problems that most bother hypertensive patients. Studies that measured QoL using the 5DEQ showed that the most disturbing domains were mobility, pain, and anxiety. However, in another study, the pain was the main difference between hypertensive and non-hypertensive patients. There are possible factors that play a role in influencing the 5DEQ score in patients with hypertension, as shown in a study in China in the community during the COVID 19 pandemic, where the most frequently reported problems were pain/discomfort, followed by anxiety/depression, and self-care were the least frequently reported problem. The study also revealed that Men were more likely to report problems in mobility than women. Meanwhile, the above 60 years group reported the most problems in mobility, usual activities, pain/discomfort, and anxiety/depression [50].
In the results of the QoL measurement, there are several differences in the problems that most bother hypertensive patients. Studies that measured QoL using the 5DEQ showed that the most disturbing domains were mobility, pain, and anxiety. However, in another study, the pain was the main difference between hypertensive and non-hypertensive patients. There are possible factors that play a role in influencing the 5DEQ score in patients with hypertension, as shown in a study in China in the community during the COVID 19 pandemic, where the most frequently reported problems were pain/discomfort, followed by anxiety/depression, and self-care were the least frequently reported problem. The study also revealed that Men were more likely to report problems in mobility than women. Meanwhile, the above 60 years group reported the most problems in mobility, usual activities, pain/discomfort, and anxiety/depression [50].
CONCLUSION
Overall, the existing assessment tools have been recognized for their validity and reliability. The SF-36 is the most frequently used assessment tool, because it is considered the easiest to use and in accordance with conditions in several regions of the world. However, this form is a general form that is not explicitly intended to assess the quality of life in hypertension only. Holistically, the existing assessment tools have not touched the spiritual domain, where this domain in some countries is an essential factor in daily life.
Limitations
Our main limitation is access to reputable databases, as this is our main barrier in all articles assessing hypertensive patients’ quality of life using various tools. The results of this review is probably suitable only in Indonesia and some Asian countries which have similar cultural issue.
Acknowledgement
We would like to express our gratitude to all parties, particularly the dean of the medical college of Haluoleo University and the dean of Science and Technology College of Sembilanbelas November University.
Conflict of interest
There is no conflict of interest.
Authors’ contribution
All authors equally contributed to preparing this article.
REFERENCES
1. Sudayasa IP, Alifariki LO, Rahmawati, Hafizah I, Jamaludin, Milasari N, et al. Determinant juvenile blood pressure factors in coastal areas of Sampara district in Southeast Sulawesi. Enfermeria Clinica. 2020;30(Supplement 2):585-588. doi: 10.1016/j.enfcli.2019.07.167.
2. Susanty S, Sukurni S, Siagian HJ. Analisis Bibliometrik Penelitian Pengobatan Herbal Penderita Hipertensi di Indonesia Menggunakan VOS-Viewer. Jurnal Keperawatan Silampari. 2022;5(2):764–71.
3. Sari AP, Lubis R. Determinant of Hypertension, Obesity and Smoking on Stroke Events in Hospital Patients at Regional General Hospital of Rokan Hulu Riau District, 2018 (Epidemiology and Public Health). Britain International of Exact Sciences (BIoEx) Journal. 2020;2(1):384–9.
4. Bangu, Siagian,H.J,Alifariki,L.O T. Differences of sodium consumption pattern hypertension sufferer in coastal and highland communities in Wakatobi islands. revista bionatura. 2021;6(2).
5. Suzanne Oparil, Maria Czarina Acelajado, George L. Bakris, Dan R. Berlowitz R, Cífková, Anna F. Dominiczak, Guido Grassi, Jens Jordan, Neil R. Poulter A, Rodgers and PKW. Hypertension. Physiology & behavior. 2016;176(1):100–106.
6. Kurnianto A, Kurniadi Sunjaya D, Ruluwedrata Rinawan F, Hilmanto D. Prevalence of Hypertension and Its Associated Factors among Indonesian Adolescents. International Journal of Hypertension. 2020;2020.
7. Zheng E, Xu J, Xu J, Zeng X, Tan WJ, Li J, et al. Health-related quality of life and its influencing factors for elderly patients with hypertension: evidence from Heilongjiang Province, China. Frontiers in public health. 2021;9:176.
8. Xiao M, Zhang F, Xiao N, Bu X, Tang X, Long Q. Health-related quality of life of hypertension patients: a population-based cross-sectional study in Chongqing, China. International Journal of Environmental Research and Public Health. 2019;16(13):2348.
9. Susanti N, Siregar PA, Falefi R. Determinan kejadian hipertensi masyarakat pesisir berdasarkan kondisi sosio demografi dan konsumsi makan. Jurnal Ilmiah Kesehatan (JIKA). 2020;2(1):43–52.
10. Atan G. Relationship between demographic features, adherence to treatment and quality of life of hypertension patients in Turkey. International Journal of Caring Sciences. 2017;10(3):1624–32.
11. Eom A-Y. Influencing factors on health related to quality of life in hypertension patients. Journal of Korean Biological Nursing Science. 2009;11(2):136–42.
12. Xie Z, Liu K, Or C, Chen J, Yan M, Wang H. An examination of the socio-demographic correlates of patient adherence to self-management behaviors and the mediating roles of health attitudes and self-efficacy among patients with coexisting type 2 diabetes and hypertension. BMC Public Health. 2020;20(1):1–13.
13. Badia X, Roca-Cusachs À, Dalfó A, Gascón G, Abellán J, Lahoz R, et al. Validation of the short form of the Spanish Hypertension Quality of Life Questionnaire (MINICHAL). Clinical therapeutics. 2002;24(12):2137–54.
14. Bahari G, Scafide K, Krall J, Mallinson RK, Weinstein AA. Mediating role of self‐efficacy in the relationship between family social support and hypertension self‐care behaviours: A cross‐sectional study of Saudi men with hypertension. International journal of nursing practice. 2019;25(6):e12785.
15. Ye R, Liu K, Zhang Z, Gong S, Chen X. Health-related quality of life of hypertension in China: a systematic review and meta-analysis. Journal of Cardiovascular Medicine. 2018;19(8):430–8.
16. Zhang Y, Zhou Z, Gao J, Wang D, Zhang Q, Zhou Z, et al. Health-related quality of life and its influencing factors for patients with hypertension: evidence from the urban and rural areas of Shaanxi Province, China. BMC health services research. 2016;16(1):1–9.
17. Pequeno NPF, de Araújo Cabral NL, Marchioni DM, Lima SCVC, de Oliveira Lyra C. Quality of life assessment instruments for adults: a systematic review of population-based studies. Health and quality of life outcomes. 2020;18(1):1–13.
18. Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement (Chinese edition). Journal of Chinese Integrative Medicine. 2009;7(9):889–96.
19. Saleem F, Hassali MA, Shafie AA, Awad GA, Atif M, ul Haq N, et al. Does treatment adherence correlates with health related quality of life? Findings from a cross sectional study. BMC public health. 2012;12(1):1–7.
20. Qian Y, Zhang J, Lin Y, Dong M, Xu M, Qian Y, et al. A tailored target intervention on influence factors of quality of life in Chinese patients with hypertension. Clinical and Experimental Hypertension. 2009;31(1):71–82.
21. Mollaoğlu M, Solmaz G, Mollaoğlu M. Adherence to therapy and quality of life in hypertensive patients. Acta Clinica Croatica. 2015;54(4).
22. Katsi V, Kallistratos MS, Kontoangelos K, Sakkas P, Souliotis K, Tsioufis C, et al. Arterial hypertension and health-related quality of life. Frontiers in Psychiatry. 2017;8:270.
23. Saboya PP, Bodanese LC, Zimmermann PR, Gustavo A da S, Macagnan FE, Feoli AP, et al. Lifestyle intervention on metabolic syndrome and its impact on quality of life: a randomized controlled trial. Arquivos brasileiros de cardiologia. 2016;108:60–9.
24. Mi B, Dang S, Li Q, Zhao Y, Yang R, Wang D, et al. Association between awareness of hypertension and health-related quality of life in a cross-sectional population-based study in rural area of Northwest China. Medicine. 2015;94(29).
25. Zygmuntowicz M, Owczarek A, Elibol A, Olszanecka-Glinianowicz M, Chudek J. Blood pressure for optimal health-related quality of life in hypertensive patients. Journal of hypertension. 2013;31(4):830–9.
26. Silva GO, Andrade-Lima A, Germano-Soares AH, Lima-Junior D de, Rodrigues SLC, Ritti-Dias RM, et al. Factors Associated with Quality of Life in Patients with Systemic Arterial Hypertension. International Journal of Cardiovascular Sciences. 2020;33:133–42.
27. Oza BB, Patel BM, Malhotra SD, Patel VJ. Health related quality of life in hypertensive patients in a tertiary care teaching hospital. J Assoc Physicians India. 2014;62(10):22–9.
28. Liang Z, Zhang T, Lin T, Liu L, Wang B, Fu AZ, et al. Health-related quality of life among rural men and women with hypertension: assessment by the EQ-5D-5L in Jiangsu, China. Quality of Life Research. 2019;28(8):2069–80.
29. Korhonen PE, Kivelä S-L, Kautiainen H, Järvenpää S, Kantola I. Health-related quality of life and awareness of hypertension. Journal of hypertension. 2011;29(11):2070–4.
30. Wong ELY, Xu RH, Cheung AWL. Health-related quality of life in elderly people with hypertension and the estimation of minimally important difference using EQ-5D-5L in Hong Kong SAR, China. The European Journal of Health Economics. 2020;21(6):869–79.
31. Trevisol DJ, Moreira LB, Fuchs FD, Fuchs SC. Health-related quality of life is worse in individuals with hypertension under drug treatment: results of population-based study. Journal of human hypertension. 2012;26(6):374–80.
32. Chen Q, Ran L, Li M, Tan X. Health-related quality of life of middle-aged and elderly people with hypertension: A cross-sectional survey from a rural area in China. Plos one. 2021;16(2):e0246409.
33. Mena-Martin FJ, Martin-Escudero JC, Simal-Blanco F, Carretero-Ares JL, Arzua-Mouronte D, Herreros-Fernandez V. Health-related quality of life of subjects with known and unknown hypertension: results from the population-based Hortega study. Journal of hypertension. 2003;21(7):1283–9.
34. Bardage C, Isacson DGL. Hypertension and health-related quality of life: an epidemiological study in Sweden. Journal of clinical epidemiology. 2001;54(2):172–81.
35. Khalifeh M, Salameh P, Al Hajje A, Awada S, Rachidi S, Bawab W. Hypertension in the Lebanese adults: Impact on health related quality of life. Journal of epidemiology and global health. 2015;5(4):327–36.
36. Qin Y, Guo Y, Tang Y, Wu C, Zhang X, He Q, et al. Impact of hypertension on health-related quality of life among different age subgroups in Shanghai: the subpopulation treatment effect pattern plot analysis. Journal of human hypertension. 2019;33(1):78–86.
37. Cuevas Fernandez FJ, Marco Garcia MT, Rodriguez Alvarez C, Iglesias Giron MJ, Aguirre‐Jaime A. Is there an association between physical exercise and the quality of life of hypertensive patients? Scandinavian Journal of Medicine & Science in Sports. 2007;17(4):348–55.
38. Borges JWP, Moreira TMM, Schmitt J, Andrade DF de, Barbetta PA, Souza ACC de, et al. Measuring the quality of life in hypertension according to Item Response Theory. Revista de Saúde Pública. 2017;51.
39. de Souza Côrtes DC, Arantes AA, Mendonça APP, dos Santos Silva J. Quality of life and hypertension. International Journal of Cardiovascular Sciences. 2016;29(6):512–6.
40. Ganesh Kumar S, Majumdar A, Pavithra G. Quality of life (QOL) and its associated factors using WHOQOL-BREF among elderly in urban Puducherry, India. Journal of clinical and diagnostic research: JCDR. 2014;8(1):54.
41. Ha NT, Duy HT, Le NH, Khanal V, Moorin R. Quality of life among people living with hypertension in a rural Vietnam community. BMC public health. 2014;14(1):1–9.
42. Melchiors AC, Correr CJ, Pontarolo R, Santos F de O de S, Souza RA de P. Quality of life in hypertensive patients and concurrent validity of Minichal-Brazil. Arquivos Brasileiros de cardiologia. 2010;94(3):357–64.
43. Zhang L, Guo X, Zhang J, Chen X, Zhou C, Ge D, et al. Health-related quality of life among adults with and without hypertension: A population-based survey using EQ-5D in Shandong, China. Scientific reports. 2017;7(1):1–7.
44. Wong ELY, Xu RH, Cheung AWL. Health-related quality of life among patients with hypertension: population-based survey using EQ-5D-5L in Hong Kong SAR, China. BMJ open. 2019;9(9):e032544.
45. Côté I, Grégoire J-P, Moisan J, Chabot I. Quality of life in hypertension: the SF-12 compared to the SF-36. Journal of Population Therapeutics and Clinical Pharmacology. 2004;11(2).
46. Chua R, Keogh AM, Byth K, O’Loughlin A. Comparison and validation of three measures of quality of life in patients with pulmonary hypertension. Internal medicine journal. 2006;36(11):705–10.
47. Schulz RB, Rossignoli P, Correr CJ, Fernández-Llimós F, Toni PM de. Validation of the short form of the Spanish hypertension quality of life questionnaire (MINICHAL) for Portuguese (Brazil). Arquivos brasileiros de cardiologia. 2008;90:139–44.
48. Soutello ALS, Rodrigues RCM, Jannuzzi FF, São-João TM, Martinix GG, Nadruz Jr W, et al. Quality of life on arterial hypertension: Validity of known groups of MINICHAL. Arquivos Brasileiros de Cardiologia. 2015;104:299–307. doi: 10.5935/abc.20150009. Epub 2015 Feb 27. PMID: 25993593; PMCID: PMC4415866.
49. Fernández-López JA, Fernandez-Fidalgo M, Martin-Payo R, Rödel A. Job stress and quality of life of primary care health-workers: evidence of validity of the PECVEC questionnaire. Atencion Primaria. 2007;39(8):425–31.
50. Ping W, Zheng J, Niu X, Guo C, Zhang J, Yang H, Shi Y. Evaluation of health-related quality of life using EQ-5D in China during the COVID-19 pandemic. PLoS One. 2020 Jun 18;15(6):e0234850. doi: 10.1371/journal.pone.0234850. PMID: 32555642; PMCID: PMC7302485.
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.

