Nurses’ knowledge of Diagnostic-Therapeutic Care Pathways (DTCP): A cross-sectional study
Ubaldino Ubaldi1*, Valentina Accinno2, Margherita Ascione3, Concetta Pane4
- Department of Ageing, Neurological, Orthopaedic and Head and Neck Sciences C.E.M.I, IRCCS - Fondazione Policlinico Gemelli - Rome (Italy)
- Department of Women's and Children's Health Sciences and Public Health DH Clinical Pharmacology, IRCCS - Fondazione Policlinico Gemelli - Rome (Italy)
- Integrated Operative Unit Maternal and Childhood Coordination - ASL Napoli 3 SUD, Naples (Italy)
- Integrated Operative Unit Maternal and Childhood Coordination - ASL Napoli 3 SUD, Naples (Italy)
*Corresponding Author: Ubaldino Ubaldi, Clinical Nurse, IRCCS - Fondazione Policlinico Gemelli - Rome. Nurses Department of Ageing, Neurological, Orthopaedic and Head and Neck Sciences C.E.M.I
Cita questo articolo
ABSTRACT
Introduction: Management by processes and clinical care pathways are now fundamental and indispensable requirements for quality improvement in healthcare organisations. The basic idea is to design a system that allows for continuous improvement in the way in which the key player in healthcare, i.e. the patient, is managed. If this were to happen, the best experiences to date tell us, it would definitively improve outcomes, efficiency and appropriateness. Moreover, patients perceive and appreciate this difference, allowing health professionals to operate at their best.
Objective: To assess the knowledge and application of the DTCPs by the nursing staff.
Materials and methods: The cross-sectional study took place in the period between June and September 2019 at the Operative Units of digestive surgery, hepatobiliary surgery, breast surgery and gynaecological surgery of the “Fondazione Policlinico Gemelli IRCCS in Rome”. A questionnaire was administered only to permanent nurses.
Results: A total of 64 questionnaires were administered of which 27 were correctly completed (response rate 42.1%) and considered valid for analysis. The sample of respondents was predominantly female (74.07%), 81.48% held a Bachelor's degree and 40.74% held a Master's degree. 55.56% knew what DTCPs were, but there was no in-depth knowledge of them in the sample. In fact, 55.56% knew whether there were active DTCPs in their region; 7.41% that nurses cannot participate in DTCPs and only 11.11% that nurses cannot participate in the review of individual DTCPs, while 59.26% were aware of the professional figures involved in the drafting and review of DTCPs. 25.93% knew what the diagnostic phase was based on and 14.81% that there were no active memoranda of understanding with public or private facilities in the diagnostic phase. Finally, only 25.93% were aware that the user could not be used in the evaluation of the outcome.
Conclusions: Although the interviewees were familiar with clinical care pathways, for most of them there had never been active involvement, they agreed on user involvement instead.
Keywords: nursing care, clinical care pathways, patient safety, diagnostic-therapeutic care pathways
INTRODUCTION
The reorganisation of the hospital network (Ministerial Decree 70/2015) and the reorganisation of Primary Care (Law 189/2012 - Balduzzi Decree) have brought about a profound and structural change in patient care and treatment in the Italian National Health Service [1-2]. The reorganisation of Primary Care, with the establishment of the AFTs (Regional Functional Aggregations) and the UCCPs (Complex Units of Primary Care), has meant tackling the problem of chronicity, with patient care, according to the Chronic Care Model and the model of integrated and structured Clinical Networks. It is a process of structural change and as such entails the need for a new culture in the definition, management and verification of the process of taking care of chronic patients: all this represents the real 'Reform'. The operational tool for treating chronic patients and co-morbidities is the Diagnostic-Therapeutic Care Pathways (DTCPs), which therefore represent the lintel of the new system [3-4].
Clinical/healthcare pathways predefine an optimal scheme of the sequence of behaviours in relation to the diagnostic, therapeutic and care pathway to be activated in the face of a typical clinical situation, in order to maximise the effectiveness and efficiency of activities [5]. DTCPs represent multidisciplinary care management technologies that map activities in a healthcare pathway, which are now considered fundamental and indispensable requirements for improving the quality of healthcare organisations in accordance with the logic of clinical governance [6]. The aim is to increase the quality of care across the continuum, improving risk-adjusted patient outcomes, promoting patient safety, increasing user satisfaction and optimising the use of resources [7].
In the entirety of its definition, construction, implementation and monitoring phases, it makes it possible to structure and integrate activities and interventions involved in the active and global care of citizens presenting health problems through a process approach, in a multidisciplinary context and on different areas of intervention (hospital, region, etc.), making it possible to assess the appropriateness of the activities carried out with regard to the objectives, the reference recommendations (Guidelines, good practices) and available resources [8]. It also allows for a measurement of activities and a comparison of results with specific indicators, leading to an improvement in each intervention in terms of effectiveness and efficiency. The need to find a shared theoretical and operational reference on what is meant by 'diagnostic therapeutic care pathway' is common among those who, at different levels and with different roles, deal with the planning of healthcare and social-health services and for those who work in them [9-10] .
The organisation of care by DTCPs is indirectly referred to by the 'Gelli' Legislative Decree (No 24/2017), the aim of which is to improve the quality of the National Health System, seeking to do so also by acting on the pillar of appropriateness of healthcare intervention, in particular, Article 5 of the aforementioned law regulates the way in which the healthcare profession is exercised, obliging healthcare professionals (doctors, nurses, physiotherapists, etc.) to adhere to the use of official guidelines and good clinical care practices [11]. Hence the need to investigate nurses' knowledge of DTCPs.
Objective
Assessing nurses' knowledge and perceptions of DTCPs
MATERIALS AND METHODS
The cross-sectional study was conducted during June-September 2019 at the Operative Units of digestive surgery, hepatobiliary surgery, breast surgery and gynaecological surgery at the “Fondazione Policlinico Gemelli Istituto di Ricovero e Cura a Carattere Scientifico in Rome (IT)”. Authorisation was requested and obtained from SITRA (Servizio Infermieristico Tecnico Riabilitazione Aziendale - Company Rehabilitation Technical Nursing Service) to proceed with the administration of a questionnaire, filled out anonymously, to the nurses on duty in the above-mentioned operational units.
The distribution took place after an interview with the nursing coordinators, providing verbal information on the questionnaire and confirmation of the processing of the data in aggregate form, not resulting in any distribution by name. After the distribution of the questionnaires to the nurses in the operating units by the coordinators, the latter collected them and placed them in a single container, which was then returned to the authors of the study.
All nurses who took part in the study well understood and signed the consent form, in which the purpose of the study and the methodology of conducting it were explained, and the personal data processing form.
The questionnaire, created ad hoc, was structured after a thorough literature search and listed in Appendix A, after the references section. The questionnaire was validated on a sub-sample of 10 nurses from the investigated sample, i.e. the questionnaire was submitted to them twice, at a minimum time interval of three days, and the statistical correlation between the two sets of answers was assessed, using the two-proportion test, with the two answers being statistically correlated if p-value >0.05 (i.e. the answers given, particularly with regard to the DTCP, were consistent at two different time points).
The questionnaire consists of 21 multiple-choice items structured as follows:
- 5 items on biographical characteristics: years of service, assigned operational unit, gender, educational qualification, post basic training;
- 16 items on DTCPs: what is a DTCP; participation of nurses in DTCP training courses; existence of DTCPs in their region and which types; whether clinical audits are planned and how often and others.
Informed consent was signed by all patients included in this study and anonymity was guaranteed. No economic incentives were offered or provided for participation in this study. The study was performed following the ethical considerations of the Helsinki Declaration[12].
Inclusion and exclusion criteria
All nurses of both sexes with a permanent contract type, who speak and understand Italian well, were included in this study, while all nurses temporarily assigned by the cooperatives (fixed-term and/or temporary assignment) were excluded from the study. However, this is a sample study with probabilistic sample selection (the only common element of inclusion is the existence of an open-ended contract).
Statistical analysis
Data was presented as numbers or percentages for categorical variables. Continuous data is expressed as the mean ± standard deviation (SD), or median with Interquartile Range (IQR).
A binomial test was performed to compare two mutually exclusive proportions or percentages in groups. The chi square test and Fisher's exact test were performed to evaluate significant differences in proportions or percentages between two groups. Particularly Fisher’s exact test was used where the chi-square test was not appropriate. The multiple comparison chi-square tests were used to define significant differences between percentages. In this case, if the chi-square test was significant (α level: 0.05), the residual analysis with the Z-test was performed. All tests with p-value(p) <0.05 were considered significant. The statistical analysis was performed by Matlab statistical toolbox version 2008 (MathWorks, Natick, MA, USA).
RESULTS
A total of 64 questionnaires were administered, 13 in digestive surgery, 14 in hepatobiliary surgery, 21 in breast surgery and 16 in cancer surgery. Only 27 questionnaires (42.8%) were returned and completed. Specifically:
- digestive surgery, 13 questionnaires delivered, 5 returned completed (38.4%).
- general surgery - hepatobiliary, 14 questionnaires delivered, 9 returned completed (64.2%);
- retroperitoneal cancer surgery, 21 questionnaires delivered, 6 returned completed (28.5%);
- gynaecological oncology, 16 questionnaires delivered, 7 returned and completed (43.7%);
In Table 1 below, we have reported the characteristics of our sample of nurses

Table 1. Characteristics of the 27 subjects participating in this study Items 1-5 of the questionnaire
Table 1 shows that the sample has a length of service ranging from 11 to 20 years (44%), is predominantly female (74%) and holds a bachelor’s degree (81%), while 40.7% of the respondents hold a Master's degree.
Table 2 shows the interviewees' knowledge of the Diagnostic-Therapeutic Care Pathway (DTCP).


Table 2. Knowledge of the interviewees about the DTCP. Items 6-15 of the questionnaire. The correct answer is indicated in bold and with an asterisk.
Table 3 shows the interviewees’ knowledge of the DTCP Protocols.

Table 3. Knowledge of the interviewees about the DTCP Protocols. Items 16-18 of the questionnaire The correct answer is indicated in bold and with an asterisk.
Table 4 shows the monitoring associated with the DTCP
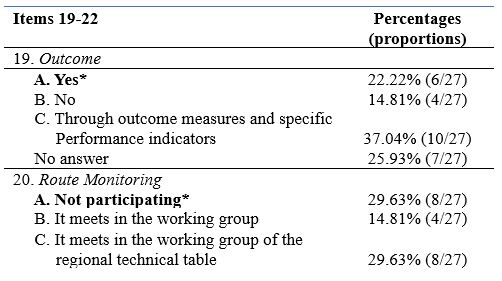

Table 4. Knowledge of the interviewees about the monitoring associated with the DTCP. Items 19-22 of the questionnaire The correct answer is indicated in bold and with an asterisk.
Finally, Table 5 shows all the statistical tests performed in this study


Table 5. Statistical tests performed in this study. Unanswered questions were not considered in the statistical analysis for each item. The correct answer in the questionnaire is indicated in bold
From Table 5, it can be seen that in our sample, there was no significant difference by seniority of service (p=0.368) and by medical area (p=0.730), while there was a significant presence of female gender (74.07%, p<0.0001) and of subjects with a Bachelor's degree (81.48%, p<0.0001). On the other hand, with regard to postgraduate education, subjects with a Master's degree were significantly more present (40.74%, p<0.0001), together with the option 'Other' (25.93%, p=0.0013).
With regard to knowledge of DTCP courses, the most frequent answer was Answer A: 'DTCP describes the pathway that a person with health problems takes between one or more health organisations and defines the best sequence of actions necessary to achieve the health objectives identified a priori' (55.56%, p<0.0001), whereas when asked about participation in DTCP courses, the answer 'No' was the significantly most frequent (74.08%, p<0.0001). Regarding knowledge of active DTCP courses in one's region, the most frequent answer was 'YES' (55.56%, p<0.0001).
When asked about knowledge of which DTCPs were active (Item 9) and of DTCPs for neurodegenerative diseases (Item 10), there was no significant difference between the answers.
In Item 11, concerning 'nurse participation', Answer C: 'partly' was the most frequent (55.56%, p<0.0001), similarly for Item 12 (Answer C: 70.37%, p<0.0001).
With regard to the clinical audit (Item 13), there was no significant difference between the various answers. In contrast, for audit cadence (Item 14), Answer D: '1/year' was the most frequent (55.56%, p<0.0001).
With regard to knowledge of published audits (Item 15), there was no significant difference between the various answers.
With regard to Item 16 (Other professional figures), the significantly more frequent answer was Answer C: 'all professional, rehabilitation medical figures provided in the multidisciplinary teams specific to that clinical condition' (59.26%, p<0.0001).
For Item 17 (DTCP phases), the most frequent answer was 'YES' (48.15%,p=0.0084). Similarly for Item 18 (SI: 51.85%, p<0.0001).
There was no significant difference between the responses associated with Items 19, 20 and 21, whereas for Item 22 (user involvement), the 'YES' response was the significantly more present (48.15%, p=0.0084),
DISCUSSION
The cross-sectional study was conducted with the aim of exploring and assessing the knowledge of DTCPs by nurses in service at the Fondazione Policlinico Gemelli (IRCCS) assigned to the Operative Units of digestive surgery, hepatobiliary surgery, breast surgery and gynaecological surgery through the administration of a questionnaire.
Almost half of the nurses interviewed to date, despite having completed a Bachelor's and a Master's degree, are not aware of the importance of DTCPs in terms of quality of care and the achievement of health outcomes: all organisations, including health care organisations, are composed of a series of processes or sets of actions, oriented towards creating value for those who know and use them [13]. It is likely that the study of Guidelines, Protocols, Procedures and DTCPs undertaken in the 1st year programme should also be taken up in the following years in the degree course, combining theory with practice.
Almost all of the nurses (74.08%), who participated in the study, were never involved in participating in the drafting of such pathways, without considering the importance of a broadly participatory approach of all components (management and technical-professional) of the organisation and the use of decision-support techniques (use of scientific evidence, audits between professionals) [14].
Healthcare institutions can use DTCPs and promote evidence-based practice to benefit quality and reduce costs [15]; however, research suggests that compliance with the use of DTCPs is low [16].
Another barrier could be resistance to the practice of change in working environments
[17], however with a proper implementation and evaluation process, change in healthcare is achievable [18].
The nurses' thoughts on user involvement are significant: in the light of these results, it can be stated that the attempt to introduce a multidisciplinary logic in healthcare organisations is hindered by the very peculiarity of the context, which is of a professional nature, in which management cannot impose itself on professionals, but must instead involve them. The task of management today is to succeed in creating those conditions that actively involve health professionals in spontaneously innovating clinical practice [19].
CONCLUSION
The implementation of DTCPs can offer the patient timely and real continuity of care, through the identification of qualified care and the integration of all professional figures. The study conducted included the assessment of nurses' knowledge on DTCPs. The results obtained show a gap in nurses' knowledge of DTCPs and this preliminary study provides several insights to improve the knowledge of DTCPs among nurses in order to ensure better continuity of patient care.
Strengths and Limitations of the study
The study has some limitations. In particular, the sample examined is a monocentric and small sample; a larger sample could have provided additional insights, reducing the possibility of statistical bias.
The study could be a preliminary step to a larger one including other operating units, not previously taken into account, so as to offer new insights given the importance of the topic for nurses.
Funding
This research did not receive any form of funding.
Conflict of interest
The authors declare that they have no conflicts of interest associated with this study.
REFERENCES
- Decreto Ministeriale 2 aprile 2015 n. 70 Regolamento recante definizione degli standard qualitativi, strutturali, tecnologici e quantitativi relativi all'assistenza ospedaliera. (G.U. 4 giugno 2015, n. 127)
- LEGGE 8 novembre 2012, n. 189Conversione in legge, con modificazioni, del decreto-legge 13 settembre 2012, n. 158, recante disposizioni urgenti per promuovere lo sviluppo del Paese mediante un piu' alto livello di tutela della salute. (12G0212) (GU n. 263 del 10-11-2012 - Suppl. Ordinario n. 201)
- Casati G., Panella M., Di Stanislao F., Gestione per processi professionali e percorsi assistenziali, terza edizione, Roma Ancona, Marzo 2005.
- Casati G., Vichi M.C., Il percorso assistenziale del paziente in ospedale, McGraw-Hill Companies SRL, Milano, 2002.
- Specchia M.L., Poscia A., Volpe M., Parente P., Capizzi S., Cambieri A., De Belvis A.G., Does Clinical Governance Influence the appropriateness of hospital stay? Bio Med Central Health Services Research, Aprile 2015.
- Broda et Al., Clinical Pathway: un metodo per il miglioramento della qualità in ambito ospedaliero, Scuola di Specializzazione di Igiene e Medicina Preventiva, Università di Torino.
- Janicek M., Casi clinici ed evidence – based medicine, Roma 2001.
- Atwal A., Caldwell K., Do multidisciplinary integrated care pathways improve interprofessional collaboration, Scandinavian Journal of Caring Sciences, 16(4):360-7,2002.
- Croce D., Sebastiano A., Castiglioni Rusconi M., Carenzi A., I PDT/PDTA nelle organizzazioni sanitarie: una meta-analisi della letteratura internazionale, economia e management “s.d” pp38-39 [online]Casati G., La gestione per processi in sanità, QA Vol 13. 1, (2002).
- Casati G., Vichi C. Il percorso assistenziale del paziente: partener di Sanità & Management Consulting Srl. Giornale di tecniche nefrologiche & dialitiche, anno XV n 2., S. Donato Milanese, Milano 2002.
- LEGGE 8 marzo 2017, n. 24 “Disposizioni in materia di sicurezza delle cure e della persona assistita, nonché in materia di responsabilità professionale degli esercenti le professioni sanitarie.” (17G00041) (GU Serie Generale n.64 del 17-03-2017)
- World Medical Association; “Dichiarazione di Helsinki della World MedicalAssociation: principi etici per la ricerca biomedica che coinvolge gli esseri umani”; 2013; Volume 5:Issue 10; e1000059
- ARESS (Agenzia Regionale per i Servizi Sanitari della Regione) Piemonte, Raccomandazioni per la costruzione dei PDTA e PIC nelle aziende sanitarie della Regione Piemonte, 2007
- Noto G, Raschetti R, Maggini M,. Gestione integrata e percorsi assistenziali. Roma: Il Pensiero Scientifico Editore. 2011
- Every N., Hochman J., Becker R., Kopecky S., & Cannon C. Critical pathways: A review. Circulation, 10, 461. 2000
- Kinsman, L. Clinical pathway compliance and quality improvement. Nursing Standard, 18, 33–35. 2004
- Seckel M., & Miller, K. Potential barriers to implementing practice alerts. AACN Reseach Work Group. 2005–2006
- Goudreau K. Notes from the board. Clinical Nurse Specialist, 20, 215–216. 2006.
- Kingston, M., Krumberger, J., & Peruzzi, W., Enhancing outcomes: Guidelines, standards, and protocols AACN Clinical Issues: Advanced Practice in Acute and Critical Care, 11, 363–374. 2000.
Appendix A
COGNITIVE QUESTIONNAIRE ON NURSES' PERCEPTIONS OF DTCPs.
Dear colleague,
We are two nurses who work at the Fondazione Policlinico Gemelli and we are conducting a cognitive survey, with the aim of surveying the knowledge of health workers on the subject of Diagnostic-Therapeutic Care Pathways.
We ask you to take a few minutes of your time to answer the questions in the questionnaire, assuring you that the results will be treated absolutely anonymously and used for statistical purposes only.
Thank you for your participation.
1. Years of service:
A. less than 10
B. 11-20
C. More than 20
2. In which area are you assigned?
A. critical area
B. medicine
C. surgery
D. Other......
3. Gender:
A. M
B. F
4. Basic qualification:
A. Qualifying title
B. University diploma
C. Bachelor's degree
5. Post-basic training (multiple answers possible)
A. Advanced training courses.....................................................
B. Master's degree (one or more) .............................................
C. Master's/Specialist Degree
D. Level II Master's degree (one or more).............................................
E. Other...........................
6. What is a Diagnostic-Therapeutic Care Pathway (DTCP)?
A. The DTCP describes the 'journey' that a person with health problems takes between one or morehealth organisations and defines the best sequence of actions necessary to achieve thehealth objectives identified a priori.
B. The DTCP is a set of guidelines, protocols and procedures
C. The DTCP is a structured pathway of healthcare acts
7. Have you ever participated in DTCP training courses?
A. Yes
B. No
C. I have never been contacted
8. Are there active DTCPs in your region?
A. Yes
B. No
C. In the planning stage for implementation
9. If you answered 'Yes' to the previous question, which one?
A. Single integrated rehabilitation pathway for the stroke patient
B. Pathway for the care and rehabilitation of patients with disorders of consciousness due to severe acquired brain injury
C. Diagnostic and therapeutic care pathway for chronic obstructive pulmonary disease
D. Definition of the pathway for early detection of suspected cases of DSA and indication for diagnosis and certification
E. Operational guidelines for the implementation in the regional network of social and health services and integrated pathways for adults with SLA
F. Operational guidelines for the prevention, diagnosis, treatment and care of people with dementia
G. Other DTCPs …………………………………………………………………………………………………………………………………………………………………
10. In your Regional Health Agency, have DTCPs been activated that may affect Neurodegenerative and Neurodevelopmental diseases?
A. Yes
B. No
C. They are in the planning stage
11. Does the professional figure of the nurse participate, and to what extent, in the drafting of the specific DTCP?
A. Yes
B. No
C. Partially
D. Participates in specific regional technical tables as a representative of the professional association
12. Does the nurse participate, and to what extent, in the review of individual DTCPs?
A. Yes
B. No
C. Only partially
13. Are clinical audits of individual DTCPs planned?
A. YES
B. NO
C. Partially
14. How often are specific audits planned for each DTCP?
A. One/month
B. One/every two months
C. One/semester
D. One/year
E. Other...
15. Are the DTCPs published on the company website or in the appropriate sections and therefore consultable by the various professionals?
A. YES
B. No
C. Only partially
16. What other professional figures are envisaged in the drafting/revision of individual DTCPs?
A. Only doctors
B. Only physiotherapists
C. All the professional, medical and rehabilitation figures foreseen in the multidisciplinary teams specific to that clinical condition
17. The DTCP envisages a Diagnostic phase and a Therapeutic-Assistance phase: are PACC, PIC and Day Service envisaged in the diagnostic phase?
A. Yes
B. No
18. Are memoranda of understanding currently in place with accredited public and/or private healthcare facilities in the Diagnostic phase?
A. Yes
B. No
C. Partially (please specify)………………………………………………….
19. In DTCPs, is the outcome used, and in what way, as a check on the effectiveness, efficiency, cost-effectiveness and appropriateness of the Pathway?
A. Yes
B. No
C. Through outcome measures and specific performance indicators set out in individual documents
20. To what extent does the nurse participate in pathway monitoring activities?
A. Not participating
B. Meetings in the working group
C. Meeting in the working group of the regional technical table
21. Are teleconsultation, telemonitoring and teleassistance activities provided for within the individual DTCPs?
A. Yes
B. No
C. In part (specify)………………………………………………….
22. Is user involvement in outcome assessment foreseen in the DTCPs?
A. Yes
B. No
Authorisation for data processing for statistical purposes consent
□ ………………………………………………………….
□ ………………………………………………………….
![]() This work is licensed under a Creative Commons
This work is licensed under a Creative Commons
Attribution-NonCommercial-NoDerivatives 4.0 International License.
THE IMPACT OF HEALTH EDUCATION ON KNOWLEDGE, ATTITUDE, PRACTICE, AND PREVENTION OF IRON DEFICIENCY ANEMIA AMONG ADOLESCENT FEMALES: A SYSTEMATIC REVIEW
Sarinah Siregar*1, Asni Johari2, Muhammad Rusdi2, Syahrial2
1Health Polytechnic, Jambi Ministry of Health, Jambi, Indonesia
2 Jambi University, Indonesia
Corresponding author: Sarinah Siregar, Prof DR GA Siwabessystreet, No.42, Buluran Kenali, Kec. Telanaipura, Kota Jambi, Jambi 36122, Phone :+62 813-6685-5307
Email: sarinah.siregar.poltekkes@gmail.com
Cita questo articolo
ABSTRACT
Introduction: Women in reproductive age are at high risk of iron deficiency anemia during the menstrual cycle. Adequate knowledge, attitudes, practices, and prevention towards anemia are necessary. There is a dearth of information on the evaluation of study characteristics and the overall quality of evidence of intervention studies in improving knowledge, attitudes and practices of anemia among adolescents.
Aim: The purpose of this study is to examine the impact of health education interventions on the knowledge, attitudes, practices, and prevention towards anemia in adolescent girls. Therefore, the review question are “What health education methods are best used to improve knowledge, attitudes, practices, and prevention of adolescent?”, “What is the effect of health education interventions on anemia in adolescent girls?”
Methods: This systematic review was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols) Checklist whichinvolved studies published between 2000 to 2021 through the databases of PubMed, ScienceDirect, Willey online Library, Cochrane, in English version. Study quality assessed using the National Institutes of Health (NIH) on controlled intervention studies. The risk of bias of the studies included assessed using The Cochrane Risk of Bias Assessment Tool.Data of the studies included were synthesized thematically in order to understand the effectiveness of mobile application. At identification stage, there are 1,414 publications were discovered through backward searching of relevant papers. The full-text screening was conducted on 34 articles and the finding 22 articles failed to meet eligibility criteria at the full-text screening stage, and only 12 articles were finally eligible for further analysis. There are twelve studies included in this study, strengthening the components of health education and increasing Iron-Folic Acid (IFA) knowledge among adolescent girls is beneficial in reducing iron deficiency anemia in adolescent girls
Results: The results of the review article showed that health education interventions, giving iron supplements and multivitamins were effective in overcoming iron deficiency anemia in adolescent girls. Educational interventions also increase the knowledge of young women about iron deficiency anemia
Conclusions: Health Education intervention for the treatment of iron deficiency anemia among adolescent female improved their knowledge, attitude, practice,and prevention
Keywords: adolescent girl, health education, iron deficiency anemia, anemia
INTRODUCTION
Anemia is a medical complication in which the number and size of red blood cells, or the hemoglobin concentration, falls below the reference range. It has the potential consequence of impairing or reducing the capacity of the blood to transport oxygen throughout the body [1–3]. Anemia is resulting from both poor nutritional status and/or poor health condition. Globally the most significant cause of anaemia is iron-deficiency (ID). The onset of anemia secondary to iron deficiency is generally assumed to account 50% of anemia occurred in the world [4].
Women of reproductive age (adolescent girls) are at a high-risk group so that 25% of students suffer iron deficiency anemia during the menstrual cycle [5,6]. Because in a period of growth and development, they need iron every day is more than 3 times that of young men [7]. The results study by Gunatmaningsih [8] showed that respondents in a period of menstruating have 1.842 times greater risk of anemia, the duration of menstruation is a predictor of anemia [9]. Blood loss during menstruation can lead the iron deficiency anemia. The amount of blood lost during one menstrual period ranges from 20-25 cc, iron loss 12.5-15 mg/month, or 0.4-0.5 mg/day. If this is added to the basal loss of 1.25 mg/day, then the total amount of iron lost is 1.25 mg/day. The volume of blood that comes out more than 80 ml occurs in adolescents who have long menstrual periods [10]. Menstrual problems can interfere the school activities and daily activities too [11].
Another factor that can exacerbate anemia in adolescent girls is the lack of iron intake, where iron in adolescent girls is needed to accelerate growth and development. The results of Shalini's research in India found that the intake of iron-rich foods low was 72% [12]. Tangerang indicated that the total iron intake in girls aged 10–12 years who suffered from anemia was only 5.4 mg/day or 25%, which is lower than the daily requirement of 20 mg/day according to the 2013 Nutritional Adequacy Ratio (RDA) [13].
Anemia causes fatigue, decreased learning concentration that impact learning achievement, can reduce work productivity [14] and quality of life in adults [15]. Anemia can reduce the body's resistance so which can increase the risk of infection. The high prevalence of anemia among adolescents if not handled properly will continue into adulthood and contributed greatly to the increase in maternal mortality (MMR), the risk of giving birth to babies with low birth weight (LBW), and stunting [14,16].
WHO (2014), has a target in 2025 to reduce the prevalence of anemia in women of childbearing age by 50% [5]. In WHO (2011) recommendations for the prevention of anemia for adolescent girls and women of childbearing age by focusing on promotive and preventive activities, through efforts to increase consumption of nutrients that contain lots of Fe, provide blood-added tablets, and increase fortification of foodstuffs with iron and acid folate. Blood supplement tablets are iron folate tablets where each tablet contained 200 mg of ferrous sulfate as well as 60 mg of elemental iron and 0.025 mg of folic acid [17].
A few studies have shown that supplementation of tablets containing 200 mg of ferrous sulfate and 0.25 mg of folic acid that increases in average Hb in adolescent girls after being given treatment [18,19]. The results of the Singh RS research (2018), effective nutritional counseling and supplements play an important role in preventing nutritional deficiencies, such as anemia [20]. Education/counseling to parents increases the cure rate for anemia in preschool-aged children, through increasing adherence to IFA consumption [21]. Adolescence also is an unique point of intervention as people of this age group are more receptive to changes in lifestyle that may determine their life course later [22]. Previous studies showed that adolescents have poor knowledge, attitudes and practices about malnutrition and dietary intake [23],[24],[25],[26]. Providing them with knowledge about iron deficiency could prevent them from anemia and the impact later in life. Enhancing health education interventions on knowledge, attitudes and practices, especially among adolescents, is potentially important in reducing anemia and mitigating short and long term consequences associated with health outcomes and those of their future offspring. There is a dearth of information on the evaluation of study characteristics and the overall quality of evidence of intervention studies in improving knowledge, attitudes and practices among adolescents especially in Asia region. Since the mid-1800s, when nursing was first acknowledged as a unique discipline, the responsibility for teaching has been recognized as an important role of nurses as caregivers. The focus of nurses’ teaching efforts is on the care of the sick and promotion of the health of the well public. In accordance to this review topic, a nurse has a great responsibility to teach people regarding nutritional anaemia. This systematic review aimed to examine the impact of health education interventions on the knowledge, attitude, practice, and prevention of iron deficiency anemia among Asian adolescent girls. This review provides an overview of the importance of educational interventions, and nurses may play an important role in educating families about anaemia and empowering them to achieve the best possible outcomes for adolescent.
MATERIAL AND METHODS
Review Protocol
We used the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement 2020 in conducting this study [27]. The study analyzed the effectiveness of health education in preventing anemia among adolescent females based on peer-reviewed studies published from 2000 to 2021. The participants, intervention, comparator, outcome, and study design (PICOS) criteria outlined in Table 1 were used to select studies for inclusion in this review.
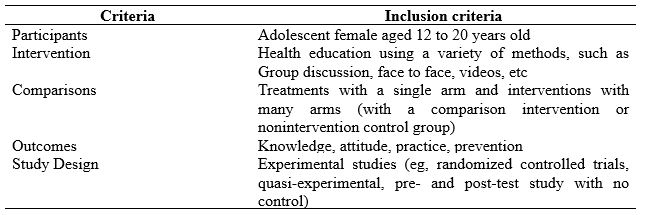
Table 1. Studies Criteria based on PICOS
Searching strategy
Databases used in collecting relevant literature include Sciencedirect, Cochrane library (Central), Pubmed, and the Wiley Online Library. We could not use other databases due to limited access or are not free access. The defined keywords adhere to the Mesh term for health research. The keywords being used are varied because they are tailored to the search engine. The keywords focus on nutritional education, empowering, Educational intervention, peer education, health promotion OR Health information AND iron deficiency anemia OR anemia AND adolescent girls OR female students. A summary of keywords combination used in each database used is reported in Table 2.
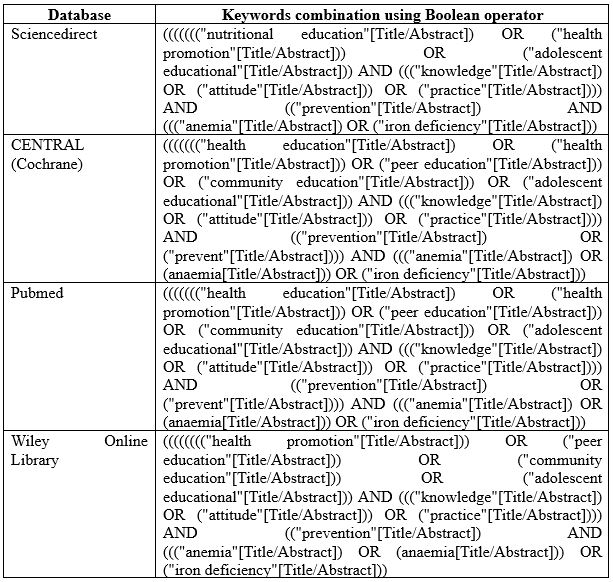
Table 2. Search strings in databases
Eligibility Criteria
We included all studies with evidence reporting the effectiveness of educational interventions in reducing and preventing iron deficiency anaemia, published from January 2000 to December 2021, written in English, and published in peer-reviewed journals. All studies using adolescent female or female students in either school or community-based settings are included in this review. Health education in any methods, intervention duration of three days at minimum, and followed up on a week, month, or year are also included in this study. Studies that reported incomplete information were excluded from duplicate publications, systematic reviews, commentaries, and letters to editors that did not provide primary data.
Information Source
After compiling keywords that match the Mesh terms, the next step is to start searching the database with free access status. The time span determined by the authors has been mutually agreed upon and is considered sufficient to describe the theme raised. Literature searches on Sciencedirect were conducted in June 2021, Cochrane library in November and December 2021, Pubmed in May 2021, and the Wiley Online Library in December 2021. We also carried out a hand search of articles, comments, letters to editors, and proceedings. The articles obtained are then collected into separate folders, for further screening. We also got several articles from the results of a bibliography search in the article.
Selection Process
Two authors independently screened each record (title/abstract), disagreement between the authors resolved by first author. Screening is done by adjusting the title, objectives, and conclusions. Other required information is obtained from the main body of the study. The screening focus was based on the inclusion criteria of this systematic review.
Study Quality
Methodologically, article quality assessment used tools from the National Institutes of Health (NIH) on controlled intervention studies. There is an assessment sheet for assessing the methodology and compliance with the inclusion criteria of this study. Scores <30% of the criteria were classified as "poor", scores between 30 and 70% were classified as "moderate", and scores >70% were classified as "good" study quality. We agreed to include articles that fall into the "fair" and "good" categories.
Risk of bias
The Cochrane Risk of Bias Assessment Tool was used to evaluate the types of bias in each of the studies. The Cochrane Collaboration Risk of Bias Tool scale contains 12 items, which assess the internal and external validity of studies. The review evaluated and rated the 12 items. Items rated ‘yes’ were scored as ‘1′, while no or unable to determine or unclear or non-applicable were all scored as ‘0′. Higher scores and percentages indicate a lower risk of bias. The level of bias within each category for each study was rated as ‘high risk’ or ‘low risk’. Each criterion had equal weight, or the same value; the total score was calculated as the percentage of the maximum value obtained. Studies with scores above the mean score were considered to have a low risk of bias, while studies below the mean value are considered to have a high risk of bias.
Data Extraction and synthesis
An independent author (SS, AJ) conducted the extraction. Discrepancies among those two authors are resolved by consensus after consulting with other investigators (MR) when failed to meet an agreement.
The extraction items consist of First author/year, country, study design (Quasi-experimental, Randomized Controlled Trial), sample size, age, type of intervention, outcomes.
RESULTS
Study Selection
A systematic electronic search identified that 1,414 publications were discovered through backward searching of relevant papers. The full-text screening was conducted on 34 articles. A total of 22 articles failed to meet eligibility criteria at the full-text screening stage, and only 12 articles were finally eligible for further analysis. The search results follow the PRISMA 2020 flow diagram (Fig. 1).
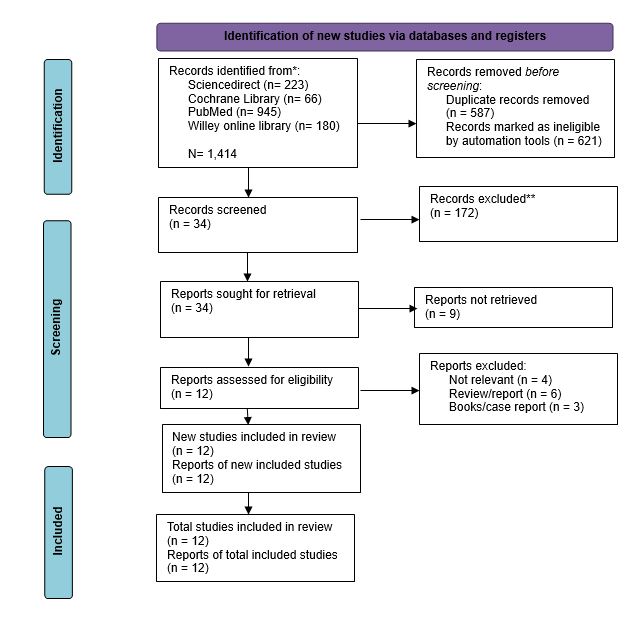
Figure 1. PRISMA flow diagram for literature search
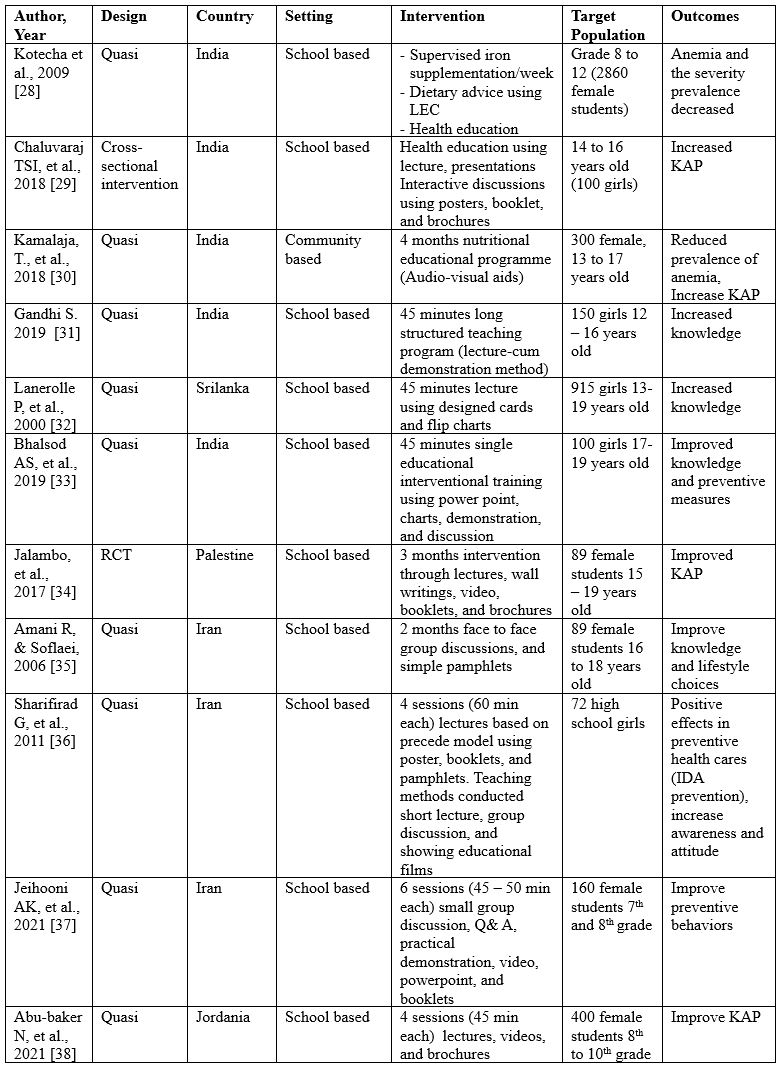
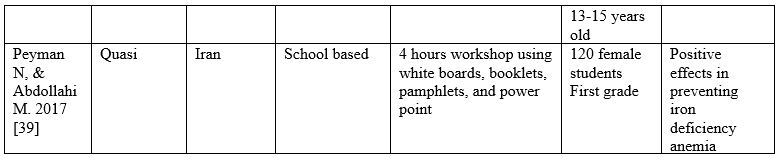
Table 3. Characteristics of the studies included
Study characteristics
Of the 12 studies that met the criteria for this review, 5 were studies conducted in India, 4 were studies in Iran, and one was conducted in Sri Lanka, Jordan, and Palestine. The study designs used were also quite varied, but most of the studies used a quasi-experimental design with a case-control approach (n= 10), and each study used an RCT and cross-sectional intervention design.
Quality Assessment
Assessment of the methodological quality of studies resulted in 6 studies with a good quality score [38] and 6 studies with a fair quality score [28].
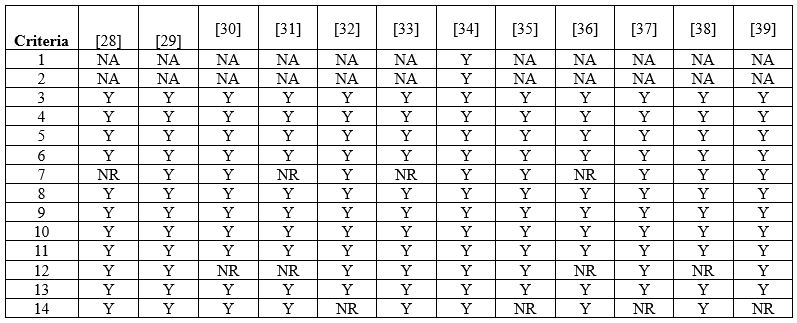
Table 4. Summary of studies quality assessment based on NIH
*Y: yes; NA: not applicable; NR: not reported
Risk of Bias
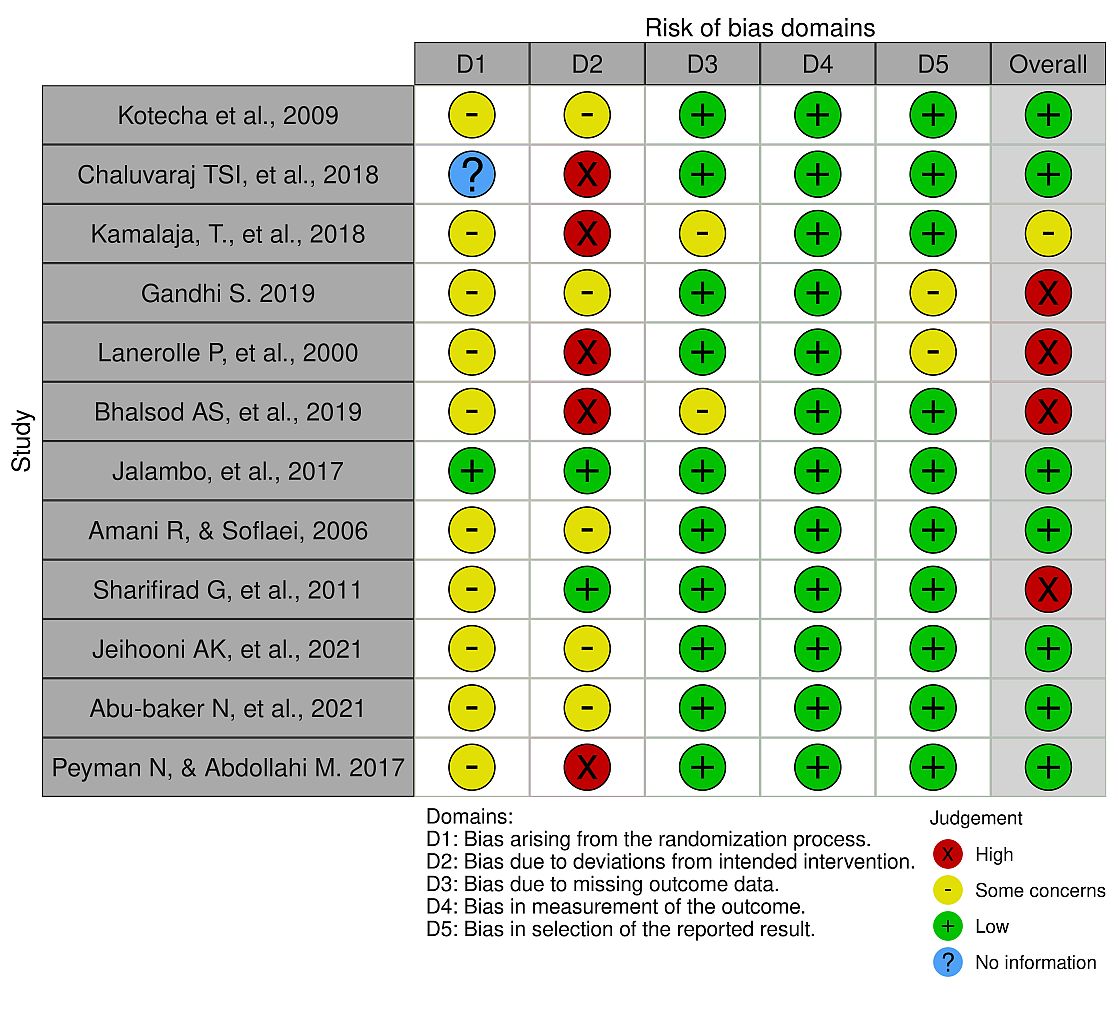
Figure 2. The Risk of Bias summary
Study setting and participants
Only 1 out of 12 studies met the inclusion criteria using a community-based setting [30]. Participants involved in the whole study were in the age range between 12-19 years old (First grade to twelfth grade), which was categorized into adolescence. Furthermore, for the gender of the participants, many of the studies we excluded were using male and female participants.
Types of intervention
The following interventions alone or in any combination were reviewed, such as Health education [28–31,33,36], Nutrition education [32,34,35,37,38], health information [39], and micronutrient supplementation (Iron) and dietary advice [28,32,34]. The shortest intervention duration was 45 minutes [29,31–33] while the longest duration was three months [34].
Types of Outcomes
We included all studies that met the inclusion criteria and limited access to relevant studies in other databases meant that we could not continue this review in the meta-analysis. For primary outcomes determined are Knowledge [31–33,35], Attitude, practice [29,30,34,38]. Meanwhile, secondary outcomes include decreased anaemia prevalence [28,30], improved prevention behaviour [33,36,37,39].
Knowledge, Attitude, Practice
In their study, Chaluvaraj et al. explained that despite numerous health education sessions in school, most female adolescents lack knowledge about anemia, its causes, prevention, and management. The study's overall findings indicated that female adolescents' knowledge, attitudes, and practices were moving in a desirable direction after the intervention. Adolescent healthcare services and facilities must be improved. Comprehensive nutritional education about anemia and its consequences for adolescents can pay considerable dividends in women's future lives [29].
According to the Kamalaja et al. study, rural adolescent girls lack essential health, food, and nutrition information. It could be due to a lack of purchasing power, access to nutritious food, false beliefs and taboos, and a lack of mass media such as TV, radio, and newspapers. Those methods provide information on good nutrition and a lack of government and non-government programs available for the health and well-being of adolescents. The health and nutrition education intervention significantly impacted subjects' nutrition knowledge [30].
Adolescent girls in the Gandhi study had moderately sufficient knowledge, attitude, practice of anemia prior to the teaching program. The majority (76.6 percent) of the adolescent children's knowledge became adequate after the structured video teaching program. Furthermore, there was no correlation between knowledge level and selected demographic variables such as age, gender, education, family type, father's job, mother's job, and monthly income [31].
Balshod et al. discovered that a single educational session significantly improves adolescent girls' knowledge of anemia. Such education interventions are to be carried out regularly in order to improve their knowledge. It encourages them to live healthy lifestyles, preventing anemia and other micronutrient deficiencies [33].
Iron deficient female adolescents in Gaza were discovered to have insufficient nutrition knowledge, attitude, and practice which could contribute to their haemoglobin and ferritin levels. Normal ferritin and hemoglobin levels, on the other hand, necessitate good knowledge, a positive attitude, and good practice. A nutrition education intervention was found to significantly improve knowledge, attitude, and practice [34].
Amani and Soflaei study aimed to improve knowledge of adolescent through the nutrition campaign. The intervention resulted in a significant change in nutritional knowledge and food-group scores consumption of adolescent girls taking part in the public education campaign [35].
Abu-Baker et al. found that more than half of the participants had adequate overall knowledge, attitude, and practice of IDA, many had insufficient knowledge of related issues, such as prior knowledge of anemia, its consequences, or foods that increase iron absorption. Implementing a nutrition education program would effectively improve female adolescents' knowledge, attitude, and practice regarding IDA. The intervention group significantly improved in these aspects after the intervention compared to the control group. Prior research has shown that implementing a structured and comprehensive educational program, even if it is a short-term program, is an effective strategy for improving knowledge, attitude, and practice among adolescents [38].
Prevention, Behavioral changes
Kotecha et al. In their study conducted IFA supplementation intervention once a week. It has proved its potential of not only improving haemoglobin but also improvement of iron stores. The serum ferritin data of over 800 girls confirmed the validity and consistency of the finding. Thus, this strategy of once a week IFA supplementation when given under supervision was effective [28].
The PRECEDE educational model was used in the Sharifirad et al. study. The PRECEDE educational model emphasizes self-care, incentives, and self-reliance through training. This method was the most effective in increasing participant knowledge and changing their attitudes toward behavior change. The PRECEDE framework is a systematic health education process that has been used in numerous studies to help organize a procedure for systematically developing programs. The main advantage of using this framework is that it delineates the factors associated with healthy behavior. It was discovered that educational programs based on the PRECEDE model were effective in controlling IDA and achieving success in other fields of study [36].
DISCUSSION
This review summarizes findings from a total of 12 studies and including 5,355 participants. Most of the studies included in this review were Quasi experimental and assessed the impact of educational intervention on the knowledge and health status among adolescents regarding iron deficiency anemia (IDA). The interventions included Nutrition education, health information, dietary advice, and supplementary micronutrient (Iron).
Given the WHO building block framework, the service delivery platform in all included studies was schools. The nutrition intervention was delivered through school teachers, student classroom monitors, and the research team. None of the included studies detailed details relating to health information systems. In all included studies, researchers provided nutritional supplements, and various non-profit organizations provided some funding. In all included studies, the investigator directly led the intervention. High school girls are one of the most important high-risk groups regarding IDA. That is why this age group was considered as a study subject.
Among the main results, we can confirm that educational intervention can positively impact knowledge, attitudes, practices, behaviour, awareness, and improvement of anaemia conditions in participants with anaemia. Giving daily or weekly iron supplements reduced the severity of anaemia experienced by participants. Only a small number of studies have provided participants with iron supplementation in addition to providing education or health information, so we cannot fully believe in the effectiveness of micronutrient supplementation. These findings require caution in interpretation since there have been very few studies, and because the quality of the results is low or very low, so they can only be seen as preliminary findings.
Booklets are the most widely used media in the studies included in this review [29,34,36,37,39]. These media used by combining several other media such as videos, power points, pamphlets, in channelling or transferring knowledge about anaemia, the results obtained show a positive effect where KAP has increased [29,34].
The overall quality of evidence-based was moderate. It indicates the reliability of the overall intervention approach and determination. The results propose the need to (i) improve the standards and procedures in intervention strategy and outcome apprising in randomized controlled trials to pinpoint actual outcomes relevant to the study population. (ii) Identify the outcomes that tend to improve the significance of health/nutrition education interventions. (iii) To enable the comparison of the methodology of the study in order to determine the factors that promote the effectiveness of health/nutrition education interventions among adolescents. Improving the methodological quality, such as random sequence generators, allocation concealment, blinding of participants, managing the dropout, including matter-of-fact reporting, and follow-up after the intervention will increase the study's quality and the overall quality outcome. More detailed and appropriate studies should focus on middle and low-income countries as they bear more global malnutrition and early marriage burden, especially adolescent females. In low- and middle-income countries, most adolescent girls have become mothers with inadequate knowledge concerning malnutrition and its consequences. Focusing on young women is crucial for themselves and their children in a short time in preventing the intergenerational cycle of IDA transmission.
The limitations of the review include limited access to the several databases which make we were unable to gain possible relevant studies. We are unable to continue with meta analysis because we only collect very few studies with moderate quality. Randomized controlled trials should be followed up to ensure continuity of the intervention. Future studies are expected to include follow-up in their research protocol. Furthermore, future studies should focus on underprivileged low- and middle-income populations through either school-based or community-based interventions.
CONCLUSIONS
Based on the studies in the review, it showed that Educational intervention for the treatment of iron deficiency anemia among adolescent female give positive impact on knowledge, attitude, practice, behavior, and awareness
Acknowledgments
We would like to thank the director of the Jambi Health Polytechnic for supporting this research.
Funding Source
This research did not receive any outside funding or support.
Authors contribution
All authors equally contributed to preparing this article
Conflict of interests
The authors declared no conflict of interest.
REFERENCES
- World Health organization. Regional office for South. East Asia. 2011;65.
- World Health Organization. Global targets 2025 to improve maternal, infant and young children nutrition. World Health Organization; 2017.
- Benedict RK, Schmale A, Namaste S. Adolescent nutrition 2000-2017: DHS data on adolescents age 15-19. In ICF; 2018.
- De Benoist B, Cogswell M, Egli I, McLean E. Worldwide prevalence of anaemia 1993-2005; WHO global database of anaemia. 2008;
- WHO. Anaemia Policy Brief. 2012;(6):1–7.
- McDaniel Jenny K. and Caryn E. Sorge. 2019. Diagnostic Approach to Anemia in Childhood and Adolescents. Springer link. DOI: 10.1007/978-3-319-96487-4_2
- Martini. Faktor - Faktor yang Berhubungan dengan Kejadian Anemia pada Remaja Putri di Man 1 Metro. Jurnal Kesehatan Metro Sai Wawai. 2015;VIII(1):1–7.
- Gunatmaningsih D. Faktor-faktor yang berhubungan dengan kejadian anemia pada remaja putri di SMA Negeri 1 Kecamatan Jatibarang Kabupaten Brebes tahun 2007. Universitas Negeri Semarang; 2007.
- Mengistu G, Azage M, Gutema H. Iron Deficiency Anemia among In-School Adolescent Girls in Rural Area of Bahir Dar City Administration, North West Ethiopia. Anemia. 2019;2019:1–9.
- Wijiastuti H. Faktor-faktor yang Berhubungan dengan Anemia pada Remaja Putri di Tsanawiyah Negeri Cipondok Tangerangtle. 2006;
- Chan, Symphorosa S C Pm Yuen, Ka Wah Yiu DSS. Menstrual Problems and health -seeking behavior in Hong Kong Chinese girls. Hong Kong Med J. 2009;15:18–23.
- Gunaratna Nilupa S, Honorati Masanja SM at all. No Title. PLoS ONE. 2015;
- Kurniawan YAI, Muslimatun S. Iron-Zinc Supplementation Among Adolescent Girls At Elementary School. 2005;(1):1–9.
- Kemenkes RI. Pedoman Penaggulangan Anemia pada Remaja Putri dan Wanita Usia Subur (WUS). Jakarta; 2016.
- Cappellini MD, Musallam KM, Taher AT. Iron deficiency anaemia revisited. Journal of Internal Medicine. 2020;287(2):153–70.
- Awisaba RE. Hubungan Antara Status Gizi dengan Tingkat Kebugaran Jasmani Tim Futsal Putra O2SN SMK Daerah Istimewa Yogyakarta. 2014.
- WHO. Guideline: Intermittent iron and folic acid supplementation in menstruating women. World Health Organization. 2011;1–30.
- Sayogo S, Sudardjat SS, Sudarsono S, Wirawan R, Margono S, Cobiac L. A study on the intervention scheme to reduce anemia in female adolescences, in Curug, Tangerang. Medical Journal of Indonesia. 2000;9(3):175–80.
- Joshi M, Gumashta R. Weekly iron folate supplementation in adolescent girls--an effective nutritional measure for the management of iron deficiency anaemia. Global journal of health science. 2013;5(3):188–94.
- Singh M, Honnakamble RA, Rajoura OP. Knowledge, Attitude and Practice Change about Anemia after Intensive Health Education among Adolescent School Girls of Delhi: An Intervention Study. International Journal of Medicine and Public Health. 2019;9(3):71–3.
- Shet Arun S; Merrick Zwarenstein; Abha Rao; Paul Jebaraj; Karthika Arumugam; Salla Atkins; Maya Mascarenhas; Neil Klar; Maria Rosaria Galanti.Shet Arun S; Merrick Zwarenstein; Abha Rao; Paul Jebaraj; Karthika Arumugam; Salla Atkins; Maya Mascarenhas; Neil. No Title. 2019;
- Bakrania S, Ghimire A, Balvin N. Bridging the gap to understand effective interventions for adolescent well-being: An evidence gap map on protection, participation, and financial and material well-being in low-and middle-income countries. UNICEF Office of Research-Innocenti New York, NY, USA; 2018.
- Rah JH, Melse-Boonstra A, Agustina R, van Zutphen KG, Kraemer K. The Triple Burden of Malnutrition Among Adolescents in Indonesia. Vol. 42, Food and Nutrition Bulletin. SAGE Publications Sage CA: Los Angeles, CA; 2021. p. S4–8.
- Singh M, Rajoura OP, Honnakamble RA. Anemia-related knowledge, attitude, and practices in adolescent schoolgirls of Delhi: A cross-sectional study. International Journal of Health & Allied Sciences. 2019;8(2):144–8.
- Shahzad S, Islam K, Azhar S, Fiza S, Ahmed W, Murtaza Z. Impact of knowledge, attitude and practice on iron deficiency anaemia status among females of reproductive age group (20-21-year-old) studying in Government Home Economics College Lahore, Pakistan. International Archives of BioMedical and Clinical Research. 2017;3(4):31–6.
- Sharmila P, Kumar MA, Rajagopala S. Knowledge, attitude and practices (KAP) related to Pandu Roga (Iron deficiency Anaemia) among adolescent girls attending Ayurveda tertiary care hospital and nearby schools-a survey. Journal of Ayurveda and Integrated Medical Sciences. 2019;4(04):154–9.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. International Journal of Surgery. 2021;88:105906.
- Kotecha P V, Nirupam S, Karkar PD. Adolescent girls’ anaemia control programme, Gujarat, India. Indian J Med Res. 2009;130(5):584–9.
- Chaluvaraj TS, Satyanarayana PT. Change in knowledge, attitude and practice regarding anaemia among high school girls in rural Bangalore: An health educational interventional study. Natl J Community Med. 2018;9:358–62.
- Kamalaja T, Prashanthi M, Rajeswari K. Effectiveness of health and nutritional education intervention to Combat anemia problem among adolescent girls. Int J Curr Microbiol Appl Sci. 2018;7(9):3152–62.
- Gandhi S. Effectiveness of Video Teaching Programme on Knowledge about Anaemia among Countryside Children with Anaemia. International Journal of Nursing Education. 2019;11(4).
- Lanerolle P, Atukorala S, De Silva G, Samarasinghe S, Dharmawardena L. Evaluation of nutrition education for improving iron status in combination with daily iron supplementation. Food and Nutrition Bulletin. 2000;21(3):259–69.
- Bhalsod AS, Dave NN, Thakor N. Impact of educational intervention regarding anaemia and its preventive measures among adolescent girls of Government Arts College of Vadodara, Gujarat, India. 2019;
- Jalambo MO, Naser IA, Sharif R, Karim NA. Knowledge, attitude and practice of iron deficient and iron deficient anemic adolescents in the Gaza Strip, Palestine. Asian Journal of Clinical Nutrition. 2017;9(1):51–6.
- Amani R, Soflaei M. Nutrition education alone improves dietary practices but not hematologic indices of adolescent girls in Iran. Food and nutrition bulletin. 2006;27(3):260–4.
- Sharifirad G, Golshiri P, Shahnazi H, Shakouri S, Hassanzadeh A. PRECEDE educational model for controlling iron-deficiency anaemia in Talesh, Iran. JPMA-Journal of the Pakistan Medical Association. 2011;61(9):862.
- Khani Jeihooni A, Hoshyar S, Afzali Harsini P, Rakhshani T. The effect of nutrition education based on PRECEDE model on iron deficiency anemia among female students. BMC Women’s Health. 2021;21(1):1–9.
- Abu-Baker NN, Eyadat AM, Khamaiseh AM. The impact of nutrition education on knowledge, attitude, and practice regarding iron deficiency anemia among female adolescent students in Jordan. Heliyon. 2021;7(2):e06348.
- Peyman N, Abdollahi M. Using of information–motivation–behavioral skills model on nutritional behaviors in controlling anemia among girl students. Journal of Research and Health. 2017;7(2):736–44.
![]() This work is licensed under a Creative Commons
This work is licensed under a Creative Commons
Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Influence of Consuming Sauropus Androgynus L. Merr, Moringa Oleifera Lam, and Vigna Cylindrica (L) Skeels on Breastfeeding Mothers: Randomized Controlled Trial
Ajeng Galuh Wuryandari1*, Indarmien Netty Ariasih1, Julaecha2
1Department of Midwifery, Health Polytechnic Jambi, Jambi, Indonesia
2Baiturrahim of College of Health Sciences, Jambi, Indonesia
Corresponding author: Ajeng Galuh Wuryandari, dr. Tazar Street, Buluran Kenali, Kec. Telanaipura, Kota Jambi, Jambi 36361, Indonesia, Orcid :https://orcid.org/ 0000-0002-7513-4666, Phone: +62 812-7978-0909, Email: wuryandariajenggaluh@gmail.com
Cita questo articolo
Background: Much scientific evidence shows the benefits of L. Merr, Moringa Oleifera Lam, and Vigna Cylindrica (L) Skeels. The leaves of these plants can be easily found in almost all of Indonesia and are a local food ingredient for Indonesian people. This study analyses the effect of the consumption of Sauropus Androgynus L. Merr, Moringa Oleifera Lam, and Vigna Cylindrica (L) Skeels on increasing the production of breastmilk while breastfeeding.
Methods: The research design used in this study was one group pretest-posttest design. The sample was taken by purposive sampling with 37 breastfeeding mothers with children aged <40 days who met the inclusion criteria. The intervention was to provide products processed as daily dishes, namely " sayur bening "with a composition of 150 grams of each plants (L. Merr, Moringa Oleifera Lam, and Vigna Cylindrica (L) Skeels), then measure the milk production by looking at how much the amount of breast milk increases after consuming the product for five days in a row, with the same seasonings. Data analysis using Wilcoxon test.
Results: The number of respondents in the study was 37 people with an age range between 19-39 years, with a child age range of 4-40 days, and the number of children owned by the respondents between 1-5 people. Analysis using the Wilcoxon test, it was found that all respondents (100%) experienced an increase in breastfeeding with p-value < 0.05, the same result was also shown in the comparison of birth weight with children's body weight after being given the intervention.
Conclusion: Consumption of Sauropus Androgynus L. Merr, Moringa Oleifera Lam, and Vigna Cylindrica (L) Skeels was statistically proven to differ in the amount of breast milk expenditure significantly. Kathree processing is adapted to everyday cooking so that postpartum nursing mothers can easily accept the taste and appearance.
Keywords: Sauropus Androgynus L. Merr, Moringa Oleifera Lam, Vigna Cylindrica (L) Skeels, Breastfeeding, Mothers
Introduction
Breast milk makes the world healthier, smarter, and more equal [1–3]. The benefits of breastfeeding can reduce the incidence of infection, increase intelligence, possibly protect against overweight and diabetes, and prevent cancer for mothers [4,5]. The Lancet report on maternal and child nutrition states that 800,000 child deaths can be prevented through breastfeeding and calls for breastfeeding support, but says that almost worldwide report a decrease in the rate of exclusive breastfeeding, including Indonesia. The reasons why women avoid or stop breastfeeding range from medical, cultural, and psychological reasons to physical discomfort and discomfort [6,7]. These things are not trivial, and many mothers without support turn to bottle feeding of formula. Multiplying across populations and involving multinational commercial interests, this situation has catastrophic consequences at the level of breastfeeding and the next generation's health [8–10].
The mother's nutritional status during breastfeeding is an effect of the nutritional status of the mother before pregnancy and during pregnancy (weight gain during pregnancy). Maternal weight gain during pregnancy depends on the nutritional status of the mother before pregnancy [11,12]. One of the most common factors associated with the failure of exclusive breastfeeding is the factor of breastfeeding that has not come out in the first week after delivery and the mother's view that her milk production is not enough. Exclusive breastfeeding for six months is one of the global strategies to improve infants' growth, development, health, and survival. Although there are many benefits of exclusive breastfeeding for babies, mothers, families and communities, its coverage is still low in various countries, including Indonesia [13,14]. The Basic of Health Research 2010 data shows that the coverage of exclusive breastfeeding for infants up to six months is only 15.3% [10].
Hereditary habits that have become local cultural wisdom in the Danau Sipin District area are various vegetables that are believed to increase breast milk, including banana hearts, long bean leaves, katu leaves, moringa leaves and many more. While in 2019, Lake Sipin was chosen to be the winner of the National Clean and Healthy Behavior Competition, the vegetables above have become regional local wisdom, with a variety of dishes derived from moringa, katu, long beans, kates. Danau Sipin District consists of 5 Kelurahan. There is 1 community health centre, namely the Putri Ayu Community Health Center. For January - September 2019, the target number of exclusive breastfeeding was 458 mothers, who gave exclusive breastfeeding 256 mothers, who did not give exclusive breastfeeding 49 for various reasons, while those who did not visit 153.
Various studies have been conducted to increase breast milk, including by giving oxytocin massage and the results are also significant. The culture of eating various vegetables such as katu leaves, Lembayung leaves (long beans) and banana flower, moringa and green beans related to their function as lactagogues is still focused on extracting and scientifically proving the function of long bean leaves and katu, moringa and kates leaves as lactagogue Traditionally processed form, namely as clear or boiled vegetables, stir-fry [5,15].
Danau Sipin sub-district in the work area of Putri Ayu Community Health Center which has a work area of 5 sub-districts. There is one coordinating midwife who is ready to participate in this research. Likewise, the head of the Driving the Empowerment of Family Welfare and his team and cadres. The leaves of long beans, katuk, and moringa are very potential to be developed both in terms of their benefits as lactagogues and the nature of these plants, which are very easy to grow with a short harvest life. Its use is still limited among Javanese and Malay tribesmen, with the processed form only as clear vegetables or boiled alone or mixed. However, not all villages have Moringa leaves, or Long bean leaves, all the time.
So far, breastfeeding mothers only consume L.Merr leaves which are used as laktagogums, whereas L.Merr leaves or also known as lavender leaves have greater benefits. Likewise, Moringa Oleifera Lam, and Vigna Cylindrica (L) Skeels leaves both contain laktagogums and saponins as well as polyphenols that can increase prolactin levels. Prolactin is a hormone that plays a major role in breast milk production [16-20]. Therefore, the development of functional supplementary food products for nursing mothers containing kathree leaves, namely Lembayung, katu, and moringa in the form of ready-to-eat products.
This study aims to analyze the effect of consumption of Kathree (Sauropus Androgynus L. Merr, Moringa Oleifera Lam, and Vigna Cylindrica (L) Skeels) on increasing the production of breast milk in postpartum mothers.
Materials and Methods
Trial design
The Randomized Controlled Trial with design of this study was one group's pretest-posttest design, namely a research design that contained a pretest before being given treatment and a posttest after being given treatment.
Participants
The sample is mothers who have babies aged < 40 days in the working area of Putri Ayu Health Center. Sampling was done by purposive sampling with 37 mothers who breastfed children aged <40 days who met the inclusion criteria. The inclusion criteria for the sample were healthy mothers and babies, primigravida mothers, while the exclusion criteria were mothers suffering from depression. The sample of this study was randomly selected from 105 postpartum mothers who visited the community health center polyclinic.
The data used in this study is secondary data from the documentation of quarterly reports at the Putri Ayu Health Center and the Jambi City Health Service which was carried out in December 2019-September 2020. The dependent variable of the study was the production of breast milk, measured by criteria 1) Frequency of urination, newborns who get enough Breast milk then urinate for 24 hours at least 6-8 time. 2) Characteristics of urination, clear yellow urine color. 3) Frequency of bowel movements, bowel patterns 2-5 times per day. 4) Color and characteristics of bowel movements, in the first 24 hours the baby excretes bowel movements which is dark green, thick and sticky, which is called meconium and beyond is golden yellow, not too runny and not too thick 5) The number of hours of sleep for babies who have enough breast milk for 2-4 hours. 6) Baby's weight. Signs of adequacy of breast milk in infants are: weight gain of more than 10% in the first week. As explained earlier that the questionnaire on breast milk production uses 6 question items, if the respondent answers yes, he will be given a score of 1 and if he answers no, he will be given a score of zero. Breast milk production questionnaire using the Guttman scale with a score range of 0-1. Breast milk production is said to be smooth if at least 4 of the 6 indicators observed in infants. If the value is less than 4 it is said no smoothly.
Intervention
Participants were given an intervention in the form of food consisting of 150 grams of each plant (L. Merr, Moringa Oleifera Lam, and Vigna Cylindrica (L) Skeels (Herbarium Medanense (Meda). The dose of food (vegetables) was determined based on the daily requirement of vitamins and minerals for postpartum mothers, namely 150 grams of vegetables consumed. 3 times a day for 7 days, if toxic effects occur during consumption of vegetables, the mother and baby will be referred to the clinic. Input (Q1) is the production of breast milk, then the mother is given Kathree vegetables (X) as an intervention, after that comes the output (Q2) in this case changes in breast milk production.
Randomisation
Sample selection using a simple random method
Blinding
In this study, 3 enumerators were used to collect research data. The previous enumerators did not know the participants because they were students who had been trained by the researcher before collecting data.
Statistical methods
Data were presented as numbers or percentages for categorical variables. Continuous data are expressed as the mean ± standard deviation (SD), or median with Interquartile Range (IQR). The data obtained were analyzed by univariate and bivariate, from the normality test (Kolmogorov Smirnov) obtained abnormal data so that the analysis used the Wilcoxon test.
All tests with p-value (p)<0.05 were considered significant. Statistical analysis was performed using the SPSS version 16.0 application.
Ethical Consideration
Registered prospective respondents have signed an informed consent and there is no incentive to participate in the study and the anonymity of participants is guaranteed. Before carrying out data collection, the researcher first took care of ethical permission. The authors state that this study followed all ethical clearance processes and was approved by the health research ethics committee of Ministry of Health Polytechnic of Jambi, Indonesia, and registration number: LB.02.06/2/18/2019.
Results
The results of the univariate analysis, which aims to determine the frequency of each variable studied, can be seen in the table 1.
Table 1 shows that most respondents in group aged 20-30 years amounted to 14 people (37.8%).
Majority of respondents’education level is low education as much as 70.3%, the dominant occupation of respondents is housewives as much as 51.4%.

Table 1. Frequency Distribution of Respondents' Characteristics
The normality test results showed that the data on the measurement of the amount of breast milk expenditure before and after the intervention was abnormal data. The results showed that all respondents (100%) experienced an increase in breastfeeding with p-value < 0.05. Statistically, there is a significant difference between before giving Kathree and after. The results can be clearer as in the table below.

Table 2. Wilcoxon Test Analysis Results about Breast Milk Production
According to the Wilcoxon test, 37 respondents experienced an increase in the amount of milk expulsion. The results of this study prove that dietary factors such as L. Merr, Moringa Oleifera Lam, and Vigna Cylindrica (L) Skeels, with a p-value < 0.05. Based on the results of this study, out of the five respondents, the baby's body weight increased by around 300 - 400 grams for 7 days of administration of purple leaf. Thus it can be stated that the provision of processed mauve leaves affects the increase in breast milk production for postpartum mothers.

Figure 1. Description of milk production
Figure 1 shows the fluctuation of post partum breast milk production before giving Kathree and an increase in milk production after the intervention.
Discussion
This study proves that food factors have a significant effect on breast milk production in addition to psychological factors and baby's suction power. Kathree gift which consists of Moringa leaves, katuk leaves, and long bean leaves, also known as mauve leaves.
Moringa oleifera Lam (synonym: Moringa pterygosperma Gaertner), commonly known as Moringa, is the most popular Moringacae clan species. Moringa oleifera grows in the form of three and is long-lived (perennial) with a height of 7-12 meters. It also has sympodial branches that point upward or oblique and tend to grow in line and lengthwise. Can grow both in the lowlands and highlands to an altitude of ± 1000 m above sea level, often planted as a barrier or fence in the yard or field.
Moringa oleifera is a local food ingredient that can be developed in the culinary of breastfeeding mothers because it contains phytosterol compounds that function to increase and accelerate milk production (lactagogum effect). Increased breast milk production, increased nutritional intake of infants, which is expected to impact the nutritional status of infants [21-22].
Moringa leaves contain high amounts of vitamin A, vitamin C, B vitamins, calcium, potassium, iron and protein which are easily consumed and assimilated by the human body. In addition, Moringa is also known to contain more than 40 anti-oxidants [23]. This content is needed by postpartum mothers who breastfeed. Breastfeeding mothers need more nutrients than during pregnancy. During breastfeeding, she needs extra energy to restore her health condition after giving birth, daily activities such as breast milk formation. In the first month after giving birth, milk production is generally abundant so that it comes out a lot and is sucked by the baby, so the mother is hungry and thirsty faster. In order for the number of calories to be balanced with the needs, adequate nutrition is needed because the energy will be reprocessed to form breast milk. During breastfeeding, the mother produces about 800-1000cc of breast milk [9,24,25].
Breast milk also contains protective compounds that can prevent babies from infectious diseases. Breastfeeding also has a tremendous emotional effect that can affect the inner relationship between mother and baby and affect the psychological development of the baby. Exclusive breastfeeding can optimize the baby's growth. Factors that influence breastfeeding are mothers who are well supported by their families and lactation education which can increase their knowledge, attitudes and behavior to provide exclusive breastfeeding for up to 6 months [24,26-28].
Previous research conducted by Zakaria [21] in Maros District on 70 breastfeeding mothers 6 weeks after giving birth showed that giving Moringa leaf extract and powder could increase breast milk volume, but the increase in the group that received the extract was higher than the group, get powder, but does not affect the quality of breast milk (iron, vitamin C and vitamin E).
Moringa oleifera is one of the alternative plants that are believed to have the potential to reduce malnutrition, hunger, prevent low birth weight, increase maternal hb levels, prevent DNA damage due to stress and prevent anemia in pregnant women [25].
Research by Situmorang [29] by giving katuk leaf stew to nursing mothers as much as 3x1 with 150 cc of katuk leaf stew. Katuk leaves are useful for increasing breast milk, for fever, and many other things. Based on research, katuk leaf infusion can increase milk production in mice. Katuk leaf root infusion has a diuretic effect at a dose of 72 mg / 100 g BW. Katuk vegetable consumption for nursing mothers can prolong the time to breastfeed the baby. The process of boiling katuk leaves can eliminate anti-protozoa properties. Katuk leaf infusion levels of 20%, 40%, and 80% in mice did not cause congenital defects and did not cause reabsorption. Raw katuk leaf juice is used for natural body slimming in Taiwan. The protein content in katuk leaves is nutritious to stimulate the release of breast milk. While the steroid and polyphenol content in it can function to increase prolactin levels. Thus the production of breast milk can increase. The steroids together with vitamin A also promote the proliferation of new alveolar-alveolar epithelium. Thus, there will be an increase in the number of elveoli in the gland which will automatically increase milk production. One of the reasons women do not give breast milk to their babies is that there is not enough milk to not be satisfied with breastfeeding. This is one of the factors that exclusive breastfeeding fails so that the mother gives formula milk to her child [12].
From the research results of Rahmawati [24] conducted a study on giving katuk leaves on increasing the production of sheep's milk. From the results of these studies, it turns out that the 20% katuk leaf extract solution given in vitro can increase milk production> 20%. The milk composition did not change, there was an increase in glucose metabolism activity by> 50%.
Suyanti & Anggraeni, [30] also states that giving katuk leaf decoction which is drunk 3 times a day (150cc in 1x drink) for 7 days can increase milk production by 50-120 ml. The Man Whitney statistical test p value <0.05 showed a significant effect of katuk leaf decoction on breast milk production based on the baby's weight gain. Mothers with sufficient breast milk can be seen from the frequency of weight gain for babies on day 10 [27].
Long bean plant (Vigna cylindrica (L) Skeels) is one plant that people believe can enlarge breasts and increase milk production. This plant has a proliferative effect on breast cells because it contains phytoestrogens, which are natural estrogens found in plants. This compound can stimulate proliferation if it binds to estrogen receptors. Long bean leaves contain 34 kilocalories of energy, 4.1 grams of protein, 5.8 grams of carbohydrates, 0.4 grams of fat, 134 milligrams of calcium, 145 milligrams of phosphorus, and 6 milligrams of iron. In addition, the Long Bean Leaves also contain as much vitamin A as 5240 IU, vitamin B1 0.28 milligrams and vitamin C 29 milligrams [5,31].
In the future, the plants from this research can be used as an alternative therapy for pregnant women who lack milk production. In addition to the effects or side effects that have not been widely reported, these three plants are very easy to find and inexpensive.
Conclusion
Moringa leaves, katuk leaves and long bean leaves were statistically proven to have significant differences in the amount of breastfeeding. Kathree processing is adapted to the form of everyday cooking so that postpartum nursing mothers can easily accept the taste and appearance. Kathree can easily be found in almost all over Indonesia, and is the local wisdom of the Indonesian people.
Study limitations
In our research, it has limitations such as the number of participants being fewer, and in this study there were 3 types of plants used for the intervention and no data analysis was carried out on each type of plant so that the efficacy of each plant could not be known, so in the future it is necessary further research
Author contributions
AGW and J contributed on concepting and designing the research. AGW and INA searched literature, analyze and interpret the data. AGW and J contributed to the paper's conceptualization, critical revision, and edited the overall improvement. All authors drafting manuscript, read and approved the final submitted paper.
Funding
This research did not receive any grant from funding agencies in the public, commercial, or non-profit sectors.
Conflict of interest
There is no conflict of interest to declare.
References
- Piro SS, Ahmed HM. Impacts of antenatal nursing interventions on mothers’ breastfeeding self-efficacy: an experimental study. BMC pregnancy and childbirth. 2020;20(1):1–12.
- Dewey KG. Nutrition, growth, and complementary feeding of the brestfed infant. Pediatric Clinics of North America. 2001;48(1):87–104.
- Butte NF, Lopez-Alarcon MG, Garza C. Nutrient adequacy of exclusive breastfeeding for the term infant during the first six months of life. World Health Organization; 2002.
- Burns E, Triandafilidis Z. Taking the path of least resistance: a qualitative analysis of return to work or study while breastfeeding. International breastfeeding journal. 2019;14(1):1–13.
- Ignjatović S, Buturović Ž. Breastfeeding divisions in ethics and politics of feminism. Sociologija. 2018;60(1):84–95.
- Brown A. Breastfeeding as a public health responsibility: A review of the evidence. Journal of Human Nutrition and Dietetics. 2017;30(6):759–70.
- Hadju Veni. Infant Nutritional Status Of 0-6 Months Of Exclusive Breastfeed Due To The Application Of Moringa Leaf Extract In Breastfeeding Mothers. Health Notions. 2018;2(6):669–74.
- Lancet T. Breastfeeding: achieving the new normal. The Lancet. 2016 Jan;387(10017):404.
- Infodatin Kemenkes RI. Situasi Dan Analisis ASI Eksklusif 2014. Pusat Data dan Informasi Kementerian Kesehatan RI; 2014.
- Kemenkes RI. Hasil utama RISKESDAS 2018 [Internet]. Kementerian Kesehatan Badan Penelitian dan Pengembangan Kesehatan. Jakarta; 2018. Available from: https://kesmas.kemkes.go.id/assets/upload/dir_519d41d8cd98f00/files/Hasil-riskesdas-2018_1274.pdf
- Langer-Gould A, Smith JB, Albers KB, Xiang AH, Wu J, Kerezsi EH, et al. Pregnancy-related relapses and breastfeeding in a contemporary multiple sclerosis cohort. Neurology. 2020;94(18):e1939–49.
- Sandhi A, Lee GT, Chipojola R, Huda MH, Kuo S-Y. The relationship between perceived milk supply and exclusive breastfeeding during the first six months postpartum: a cross-sectional study. International Breastfeeding Journal. 2020;15(1):1–11.
- Rezal F. Hubungan Pengetahuan, Sikap dan Status Ekonomi dengan Pemberian ASI Esklusif Pada Bayi Usia 0-6 Bulan di Wilayah Kerja Puskesmas Lampeapi Kabupaten Konawe Kepulauan. Nursing Care and Health Technology Journal (NCHAT). 2021;1(2):94–101.
- La Adili DRS, Salma WO, Tosepu R. Factors related to the exclusive breastfeeding in the working area of PHC Poasia, Kendari City. Iberoamerican Journal of Medicine. 2021;3(4):300–6.
- Mensah KA, Acheampong E, Anokye FO, Okyere P, Appiah-Brempong E, Adjei RO. Factors influencing the practice of exclusive breastfeeding among nursing mothers in a peri-urban district of Ghana. BMC research notes. 2017;10(1):1–7.
- Purnanto NT, Himawati L, Ajizah N. Pengaruh Konsumsi Teh Daun Kelor Terhadap Peningkatan Produksi ASI di Grobogan. Jurnal Keperawatan dan Kesehatan Masyarakat Cendekia Utama. 2020;9(3):268–71.
- Johan H, Anggraini RD, Noorbaya S. Potensi Minuman Daun Kelor Terhadap Peningkatan Produksi Air Susu Ibu (ASI) PAda Ibu Postpartum. Sebatik. 2019;23(1):192–4.
- Firdausi A, Qomar UL. Penerapan Pemberian Olahan Daun Lembayung dalam Produksi ASI. Proceeding of The URECOL. 2019;33–9.
- Widyawaty ED, Fajrin DH. Pengaruh Daun Lembayung (Vigna sinensis L.) Terhadap Peningkatan Produksi Asi Pada Ibu Menyusui Bayi 0-6 Bulan. NERSMID: Jurnal Keperawatan dan Kebidanan. 2020;3(2):93–100.
- Suwanti E, Kuswati K. Pengaruh Konsumsi Ekstrak Daun Katuk Terhadap Kecukupan Asi Pada Ibu Menyusui Di Klaten. Interest: Jurnal Ilmu Kesehatan. 2016;5(2):132–5.
- Zakaria Z, Hadju V, As’ ad S, Bahar B. Pengaruh Pemberian Ekstrak Daun Kelor Terhadap Kuantitas Dan Kualitas Air Susu Ibu (Asi) Padaibu Menyusui Bayi 0-6 Bulan. Media Kesehatan Masyarakat Indonesia. 2016;12(3):161–9.
- Heryati, Paath EF, Rumdasih Y. Nutrition in Reproductive Health. Jakarta: EGC; 2005.
- Mutiara T, Titi ES, Estiasih W. Effect lactagogue moringa leaves (Moringa oleifera Lam) powder in rats. Journal of basic and applied scientific Research. 2013;3(4):430–4.
- Gunanegara RF, Suryawan A, Sastrawinata US, Surachman T. Efektivitas Ekstrak Daun Katuk dalam Produksi Air Susu Ibu untuk Keberhasilan Menyusui. Maranatha Journal of Medicine and Health. 2010;9(2):151203.
- Hackman, N. M., Schaefer, E. W., Beiler, J. S., Rose, C. M., & Paul IM. Breastfeeding Outcome Comparison By Parity. Breastfeeding Medicine. 2015;10(3):156–62.
- Djama N. Effect of Long Bean Leaves Consumption on Increased Breast Milk Production in Breastfeeding Mothers. Jurnal Riset Kesehatan. 2018;7(1):5.
- Emmanuel A. A Literature Review Of The Factors That Influence Breastfeeding. International Of Nursing And Health Science. 2015;2(3):28–36.
- Estiyani A, Suwondo A, Rahayu S, Suharyo Hadisaputro MNW, Susiloretni KA. The Effect Of Moringa Oleifera Leaves On Change In Blood Profile In Postpartum Mothers. Belitung Nursing Journal. 2017;3(3):191–7.
- Situmorang TS. The Effect of Consumption of Water Decoction of Katuk Leaves on the Expenditure of Breast Milk Production in Postpartum Mothers in the Independent Practice Midwife Manurung Medan in 2018. Stikes Murni Teguh. 2019;1(2).
- Suyanti S, Anggraeni K. Efektivitas Daun Katuk Terhadap Kecukupan Air Susu Ibu (Asi) Pada Ibu Menyusui Di Bidan Praktek Mandiri (Bpm) Bd. Hj. Iin Solihah, S. St., Kabupaten Majalengka. Journal of Midwifery Care. 2020;1(1):1–10.
- Fachruddin F, Suprayogi A, Hanif N. Addition of Katuk Leaf Hexane Fraction of Zanzibar Varieties in Feed Increased Milk Production, Display of Mother and Young Rats. Jurnal Veteriner. 2017;18(2289–296).
![]() This work is licensed under a Creative Commons
This work is licensed under a Creative Commons
Attribution-NonCommercial-NoDerivatives 4.0 International License.
Technological innovations in cardiac electrostimulation: Professional updating and cultural evolution of nurses
Carlo Uran1, Pasquale Piscitelli2, Mariuccia falco3, Giovanna Bombace3, Palma Eterno3
1 Interventional cardiologist. Cardiology and Intensive Care Unit, “San Giuseppe e Melorio” Hospital, Santa Maria Capua Vetere, Italy
2 Registered nurse. Cardiology and Intensive Care Unit, “San Giuseppe e Melorio” Hospital, Santa Maria Capua Vetere, Italy
3 Graduate nurse. Cardiology and Intensive Care Unit, “San Giuseppe e Melorio” Hospital, Santa Maria Capua Vetere, Italy
Corresponding author: Dr. Carlo. Uran, Cardiology and Intensive Care Unit, “San Giuseppe e Melorio” Hospital, Santa Maria Capua Vetere, Italy. Email: carlura@libero.it
Cita questo articolo
Abstract
Cardiology made enormous advances in the treatment of extremely severe diseases such as heart failure. Specifically, interventional cardiology has been enriched, over the years, with increasingly complex aids that have contributed in improving the quality of life and survival of patients suffering from this disease. These advances in technique compel the interventional cardiologist being constantly updated on new procedures and therapy. As a result, both the ward nurses and those supporting the cardiologist in the surgery room, must acquire the knowledge that allows them to be always in step with the fast-changing times.
The aim of this commentary is to underlining the importance of a continuous updating of nurses by emphasizing that their role has been changing over the years and that these professionals, along with the physicians, must stay up-to-date regarding technological innovations, within the limits of their specific skills.
Keywords: Heart failure; Cardiac Contractility Modulation; Nurse updating
Introduction
Nurses of interventional Cardiology unit must acquire more and more skills because of the evolution of technology and subsequently of the complexity of implantable devices. The acquisition of skills is a continuous process and requires constant effort. Therefore, not only the physician, who remains the main operator, must constantly update himself on new techniques and procedures, but also nurses who assist him in and out the operating room, must acquire the scientific mentality that allows them to get highly specialized technical knowledges. In the field of interventional cardiology, advances in technology made care approach increasingly complex, before, during and after an interventional procedure. In such a large and constantly evolving field, nurses should necessarily acquire all the skills for the assistance process and should consequently have the ability to analyze, decide and execute the most appropriate and safe care services, supported by solid evidence of effectiveness. Cardiac Contractility Modulation (CCM) therapy, delivered by OPTIMIZER SMART®, is part of the non-pharmacological therapy for treatment of heart failure with reduced or moderately reduced ejection fraction, in symptomatic patients (NYHA class II-IV) despite optimized medical therapy [1]. It is an important technological innovation for the treatment of this severe disease. The CCM acts by delivering a high-energy non-excitatory bipolar signal, synchronized with local electrical activity, in the ventricular absolute refractory period, by means of two active-fixation leads, placed on the IVS and spaced from each other by no more than 1 cm. Both leads can have a sensing and therapy delivery function. In the implantation phase, is very important to be meticulous in positioning the leads so that they have a sensing greater than 4 mV at the PSA. In the short and long term, this treatment increases left ventricular contractility. As result, the CCM therapy improves clinical status, functional capacity, quality of life and prevents hospital admissions of carefully selected patients [2]. The selection of the patient to whom implant this device, takes place by evaluating his quality of life and the frequency of hospitalizations for heart failure. Quality of life is assessed by the MLWHFQ questionnaire. A score over 30 in a patient in NYHA II class is indicative of severe lack of autonomy and is a significant element in the decision to implant such device (Fig. 1). The interventional procedure does not differ from those implemented for the implantation of other cardiac devices. The difference is about the periodic checking of the implanted device, performed by the cardiologist with the help of a biomedical engineer, who analyze the data by a portable computer loaded with a specific software, by which, electrical parameters and therapy delivery time are tested. The therapy delivery time must be at least 7 hours per day and a parameter to pay attention to is the percentage of therapy delivery, which must be as high as possible and not fall below 80%. [3].
Discussion
Many papers describe implantation procedure and the role of nurses [4-5-6]. After the surgery, nurse takes the patient back to the ward and performs an ECG. Nurses who record the ECG should be able to understand whether the device is properly working or not. The typical ECG of a patient implanted with a CCM device shows a ‘spike’ in the absolute refractory period of cardiac cycle: the ‘R wave’ of QRS complex. (Fig. 2). Nurses should know that the presence of a ‘spike’ on the ‘R wave’ of the QRS complex is not a non-capturing sign or a sensing defect: it is the proper operating of the device itself. This knowledge is important in order not to alarm the patient and inappropriately alert the cardiologist. The day after implantation, nurses should check the surgical wound, evaluate whether there is a hematoma or not and if medical attention is required. Then the patient can undergo to a chest x-ray to evaluate the position of the leads and to exclude a PNx, if the subclavian vein puncture has been performed without echo guide [7]. OPTIMIZER SMART® is powered by a weekly-rechargeable battery through an induction mini-charger, rechargeable itself, delivered to the patient. At bedside, physician and nurses instruct the patient, with the assistance of biomedical engineer, regarding its use. It is important, in this phase, that nurses as well assist the patient and reassure him about the easiness of device recharging procedure. Patient should charge the device battery weekly and it is advisable to suggest him to always recharging the device on the same day and at the same time, specifying however that it is not a life-saving device, but an electrical therapy provider. This avoids the worry of postponing or anticipating the charging process. Nurses get involved in many ways in interventional procedures: they manage the pre-operation care and technical setup; help the physician in the surgical room; check the correct functioning of the device and, if complications are detected, alert the physician and look for a quick solution to them. In order to perform these tasks, nurses should know how the device acts and which complications might occur after intervention, so they can be able to deal with them without any anxiety. In 2014 in order to assess critical care nurses' knowledge and practice regarding implantable cardiac devices in Egypt, was published a paper by which authors showed that Critical care nurses have inadequate knowledge and practice regarding implantable cardiac devices [8]. Unfortunately, things have not changed over the years. In 2017, in order to assess cardiology nurses' knowledge and confidence in providing education and support to ICD recipients, Steffes et al. published a paper. The result was surprising: authors proved that the ICD knowledge of US nurses in 2015 was similar to that reported in the United Kingdom in 2004 [9-10], with limited knowledge about the complexities of modern ICD devices. Such deficits in knowledge may affect the quality of education provided to ICD recipients in preparing them to live safely with an ICD. A survey published in 2021 by Fitzimons et al, showed that many nurses felt not being living up to their job and emphasize the importance of in continuing cardiovascular nursing education and of their professional updating[11]. Nowadays, the nurses should be a complete professional and should have the technical and care skills required to obtain the best result in interventional procedures, as regard the new generation devices as well. Consequently, the interventional cardiology/electrostimulation nurses are required to have not only care skills, but also the knowledge of devices. In CCM therapy, electrical stimulation is delivered to the cardiac muscle during the absolute refractory period. In this phase, the electrical signals activate the mobilization of calcium ions in the cardiomyocytes. The mechanism of action of the CCM can be summarizing as follows: CCM signals applied during the absolute refractory period cause an increase of cytosolic calcium during the systole, resulting in improving the cardiac contraction [12]. The mechanism of action explains the typical ECG of a patient with CCM and the nurses must be able to recognize it in order not urgently alert the doctor. This is the reason why nurses as well should know it. Furthermore, nurses have to be aware about the effects of such therapy. A few seconds after the delivery of the therapy, normalization of the activity of the proteins that are involved in regulation of intracellular calcium, occurs. After a few hours, there is a progressive normalization of the abnormal expression of fetal gene program, which is a characteristic of heart failure. Reverse remodeling has been demonstrated within 3 months, with reduction of mechanical and neuro-hormonal stress and increase of left ventricular ejection fraction. CCM restores the structure and function of damaged cells to their normal state [13]. Due to this action, CCM improves clinical outcomes in terms of exercise tolerance and QOL at 6 months [14], and this is the reason why guidelines published in 2016 and the Consensus HFA ESC 2019, state that CCM can be considering in selected patients with HF [15]. In 2020, Giallauria et al. evaluated the three currently available randomized controlled trials of CCM therapy for treatment for patients with heart failure. This comprehensive meta-analysis made the authors conclude that CCM provides statistically significant and clinically meaningful benefits in measures of functional capacity and HF-related quality of life [16]. The latest ESC guidelines on heart failure (2021) suspend the judgment on CCM ('under evaluation'), since its effect on the long-term mortality rates of patients with heart failure has not evaluated yet in a randomized controlled multicenter trial [17]. However, it is noteworthy that some preliminary studies showed that CCM improves clinical outcome in terms of exercise tolerance and QOL. Besides, it improves long-term survival, compared with the mortality predicted by the Sattle Heart Failure Model Score and reduces hospitalizations by 75%. [18]. Due to these considerations, we highlighted that the cardiology nurses have not an adequate preparation. Because of this, patient care inevitably suffers. This is the reason why we believe that it is mandatory for the nurse to be updated both about procedures and about devices. They should have adequate knowledge about the indications and the mechanism of action of devices. Furthermore, as regard the CCM, it is mandatory for the cardiology nurses, the knowledge of the typical ECG of a patient implanted with such device.
Acknowledgement
The authors warmly thank Serena Costanza Uran for her collaboration in the translation
Funding statement
This paper did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Competing interest statement
There are no competing interests for this study.
Authors’ contribution
Dr. C. Uran: Investigation, conceptualization, resources, preparation and translation of the paper. Dr. M Falco; P. Piscitelli; Dr. G. Bombace; Dr. P. Eterno: Preparation
References
- https://www.fda.gov/media/123038/download;
- Abraham WT, Smith SA. Devices in the management of advanced, chronic heart failure. Nat Rev Cardiol. 2013;10(2):98-110.
- Abraham W.T et al. A Randomized Controlled Trial to Evaluate the Safety and Efficacy of Cardiac Contractility Modulation. J Am Coll Cardiol HF 2018;
- Kim Rajappan, Cardiac Department, John Radcliffe Hospital, Headley Way, Headington, Oxford OX3 9DU, UK; Education in Heart Arrhythmias. Permanent pacemaker implantation technique: part I; http://dx.doi.org/10.1136/hrt.2007.132753
- Rajappan K. Permanent pacemaker implantation technique: part II. Heart. 2009;95(4):334-342. doi:10.1136/hrt.2008.156372
- Porfili A. Protocollo infermieristico per procedure di elettrostimolazione: impianto o sostituzione di Pacemker, Defibrillatori, Dispositivi per la terapia di re sincronizzazione cardiaca (CTR) Linee guida AIAC 10.2018
- Glikson M, Nielsen JC, Kronborg MB, et al. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J. 2021;42(35):3427-3520. doi:10.1093/eurheartj/ehab364
- Nahla Shaaban Ali; Warda Youssef; Abdo Mohamed; Ali Hussein Nurses' knowledge and practice regarding implantable cardiac devices in Egypt. British Journal of Cardiac Nursing 10, No. 1. Published Online:26 Dec 2014https://doi.org/10.12968/bjca.2015.10.1.34
- Steffes SS, Thompson EA, Bridges EM, Dougherty CM. Knowledge of Implantable Cardioverter Defibrillator Purpose and Function Among Nurses in the United States. J Cardiovasc Nurs. 2017;32(3):304-310. doi:10.1097/JCN.0000000000000339
- Tagney J. Can nurses in cardiology areas prepare patients for implantable cardioverter defibrillator implant and life at home? Nurs Crit Care. 2004;9(3):104Y114
- Donna Fitzsimons, Matthew A Carson, Tina B Hansen, Lis Neubeck, Mu’ath I Tanash, Loreena Hill, The varied role, scope of practice, and education of cardiovascular nurses in ESC-affiliated countries: an ACNAP survey, European Journal of Cardiovascular Nursing, Volume 20, Issue 6, August 2021, Pages 572–579, https://doi.org/10.1093/eurjcn/zvab027
- Borggrefe, M.; D. Burkhoff (Jul 2012). “Clinical effects of cardiac contractility modulation (CCM) as a treatment for chronic heart failure”. Eur J Heart Fail. 14 (7): 703–712.
- Butter, C.; et al. (May 2008). “Cardiac Contractility Modulation Electrical Signals Improve Myocardial Gene Expression in Patients With Heart Failure” (PDF). J Am Coll Cardiol. 51 (18):1784–1789.
- Kuschyk et al. Cardiac Contractility Modulation treatment in patients with symptomatic heart failure despite optimal medical therapy and cardiac resynchronization therapy (CRT) International Journal of Cardiology 277 (2019) 173-177 .
- Petar M. Seferovic et al ”Clinical practice update on heart failure 2019: pharmacotherapy, procedures, devices and patient management. An expert consensus meeting report of The Heart Failure Association of the European Society of Cardiology.
- Giallauria F, Cuomo G, Parlato A, Raval NY, Kuschyk J, Stewart Coats AJ. A comprehensive individual patient data meta-analysis of the effects of cardiac contractility modulation on functional capacity and heart failure-related quality of life. ESC Heart Fail. 2020;7(5):2922-2932.
- McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure [published correction appears in Eur Heart J. 2021 Oct 14;:]. Eur Heart J. 2021;42(36):3599-3726.
- “MAGGIC” Heart Failure Risc Calculator according to Pocock et al. Predicting survival in heart failure: a risk score based on 39372 patients from 30 studies, Eur Heart J (2013) 34(19) 1404-1413.

Figure 1. The Minnesota questionnarie 21 items

Figure 2. ECG of a patient with a CRT-D system, implanted with the CCM device

Table of abbreviations
Sleep Quality Related to Vigilance Among Nurses in Hospital: A Cross Sectional Study
Debbie Nomiko1*, Ernawati1, Bettywaty Eliezer1
1Nursing Department, Health Polytechnic Ministry of Health Jambi, Indonesia
Corresponding author: Debbie Nomiko, dr. Tazar Street, BuluranKenali, Kec. Telanaipura, Kota Jambi, Jambi 36361, Indonesia, Orcid :https://orcid.org/0000-0002-3623-7937, Phone: +62 812-7897-981, Email: debbiedebbienomiko@gmail.com
Cita questo articolo
ABSTRACT
Introduction: Sleep quality disorders may cause a decrease in concentration and work performance of individual. It is also believed that nurses with work shifts as health workers may run into sleep quality disorders. Several researches have shown the relationship between sleep quality and the work performance of nurses in shifts duty. This study aimed to determine the relationship of sleep quality and vigilance of nurses in shifts duty in Raden Mattaher hospital Jambi.
Methods: A cross sectional study was performed recruiting 97 nurses working shifts in 3 inpatients wards of the Raden Mattaher Hospital Jambi. Socio-demographic details and data nurses alertness were collected using ad hoc questionnaires, data sleep quality were collected using the Pittsburgh Sleep Quality Index. Relationships among sleep patterns and alertness variables were investigated. Data were analyzed by univariate and chi-square test (CI 95%). Statistical analysis was performed using the SPSS version 16.0.
Results: Results showed an average of 29.4 years of age. Respondents were mostly female, married with working time <5 years. The results of the bivariate analysis show there was not relationship between sleep quality and vigilance of nurses who undergoing shifts in Raden Mattaher hospital Jambi with p-value 0.35.
Conclusion: There was not a relationship between sleep quality and vigilance among nurses undergoing a shift in patients' rooms
Keywords: Nurses, Sleep Quality, Wakefulness, Shift Work Schedule
INTRODUCTION
The prevalence of sleep quality disorders every year tends to increase, one of the causes is fatigue due to excessive work volume [1–4]. Poor sleep quality may cause adverse effects workers physical and psychological health leading to negative consequence workplace such as mistakes and reduced performances [5–8]. Health professionals have been known to experience fatigue at times. The condition has also long been associated with reduced patient safety [9,10]; decreased satisfaction, health and well-being [11–13]; more conflict among team members [14]; risk of needle stick injuries [14,15] and increased staff turnover [10]. Nurses, the largest group of healthcare providers, are prone to relatively high acute burnout, chronic fatigue, and recovery from fatigue after shift changes [16]. It is closely related to the demands they face throughout the working day, such as physical, mental, emotional demands and pressures associated with shift and non-standard work schedules. These factors place hospital nurses very vulnerable to burnout and its accompanying effects [17].
Nurses are professional workers who use a shift work system, so it can be ascertained that sleep quality disorders can also occur in nurses who undergo shifts [18–20]. Shift work has an impact on disturbances in circadian rhythms [21], and the main one being sleep pattern disturbances that cause sleep deprivation and fatigue [22,23].
Vigilance is degree of readiness of a person in responding to something [24] A person's level of vigilance is needed at work. Accidents occur as a result of decreased levels of alertness [25]. Variables that affect the level of alertness are monotonous state, level of sleepiness, psychophysiology, distraction, and work fatigue. In the variable of sleepiness level, there are 3 indicator variables, namely, circadian rhythm, sleep quality, and sleep time [26,27]. Research results show that 78% of nurses who work shifts experience changes in sleep quality. Furthermore, poor sleep quality is one of the contributing factors to medical errors that occur in health services [28–30]. The impact of poor sleep quality has been widely studied. Sleep absence is an important predictive factor influencing the occurrence of various chronic diseases such as hypertension [31] and cardiovascular disease [32], and diabetes [33]. Nurses' inconsistent sleep habits can have a severe impact on their health as well as their ability to do their jobs [34,35].
METHODS
Trial design
A cross-sectional study was made at the Raden Mattaher Hospital Jambi.
Participants
The population in this study was all shift nurses in 3 inpatient installations at Raden Mattaher Hospital Jambi with a total sample of 97 people with the criteria of nurses in the inpatient installation, not leave, having at least a minimum nursing diploma.
Intervention
A study questionnaire was made to collect socio-demographic details and a 24 items questionnaire was implemented to collect nurses’ alertness data. to four point scored Likert scales (always, often, sometimes and never) were used for the self-assessment of nurses’ alertness before, during and after care activities, with particular attention to missed cares, mistakes and documentation management. Nurses’ sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI) tool [36]. Authors declare that the PSQI (Indonesian version) permission to use was obtained by the copyright property.
The PSQI is widely considered the gold standard tool for sleep patterns evaluation and quality of sleep assessment. It provides a global score ranged from 0 to 21 where scores higher than 5 means poor sleep quality. Furthermore, it provides 7 sub-scores assessing sleep patterns: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medications, and daytime dysfunctions. The PSQI questionnaire was translated into Indonesian and
tested for reliability with Cronbachs alpha result of 0.753. Data were collected by three interviewers who were unknown to the participants before the study.
Blinding
In this study, 3 enumerators were used to collect research data. The previous enumerators did not know the participants because they were students who had been trained by the researcher before collecting data.
Ethical Consideration
Before carrying out data collection, the researcher first took care of ethical permission. The authors state that this study followed all ethical clearance processes and was approved by the health research ethics committee of Jambi Universitys Faculty of Medicine and Health Sciences.
Statistical methods
Data were presented as numbers or percentages for categorical variables. Continuous data are expressed as the mean ± standard deviation (SD), or median with Interquartile Range (IQR). The chi square test and Fisher's exact test were performed to evaluate significant differences of proportions or percentages between two groups. Particularly Fisher's exact test was used where the chi square test was not appropriate. All tests with p-value (p)<0.05 were considered significant. Statistical analysis was performed using the SPSS version 16.0 application.
RESULTS
Ninety-seven out of one hundred twenty-two nurses working shifts in 3 wards) qualified nurses
completed their studies. The results of this study presented in the table 1.
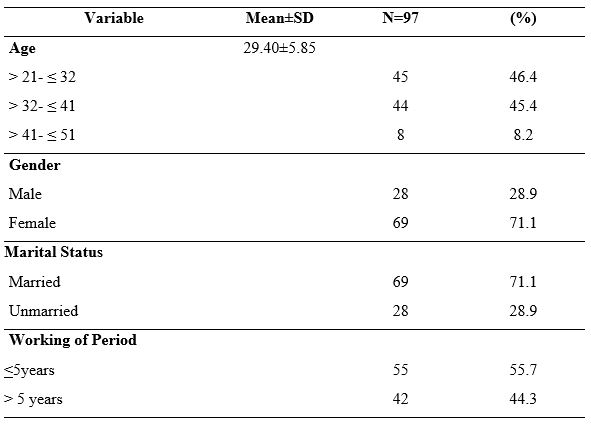
Table 1. Demographic Data of Nurses Undergoing Shift
Most of respondents were female (71.1%), married (71.1%) and have working of period < 5 years (55.7%). These results showed the average age of the respondents was 29.40 years, and the age range was between 21-51 years (SD 5.85).
Table 2 shows the results of the assessment of the seven components of the respondent's sleep quality, it was found that the component of the use of sleeping pills (using pills) had the highest score in terms of not using, namely 97.93%, the second highest score was the component of the subject's sleep quality, namely the subjective average of respondents stated 86.6% had good sleep quality. The results also showed that most of the respondents had sleep disturbances as much as 65%, and as many as 40% had sleep efficiency in the range of 75-84%.
That most nurses (86.6%) have good sleep quality based on subjective sleep quality. In the second component (sleep latency), most of the respondents (51.5%) had a sleep latency of 1-2 hours, and merely a small portion (7.2%) had a sleep latency of 5-6 hours.

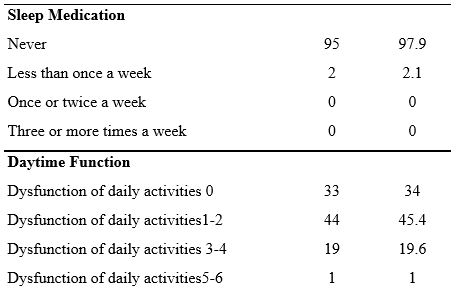
Table 2. Sleep Quality Components: Subjective and Objective Sleep Quality measures
In the third component (sleep duration), most of the respondents, as many as 32% of respondents, had sleep duration < 5 hours and only five respondents (5.2%) had sleep duration > 7 hours. Furthermore, 26.8% of the fourth component had a daily sleep efficiency > 85%, and only 14 respondents (14.4%) had a daily sleep efficiency of 14.4%. This result is slightly different from the previous study [49], which showed that 73.5% of nurses have sleep efficiency >85%.
Sleep quality in terms of sleep disturbance components shows that most of the respondents (67%) have sleep disorders with a score of 1-9, then for the use of sleeping pills, most of the respondents (97.93%) have never used sleeping pills at all.
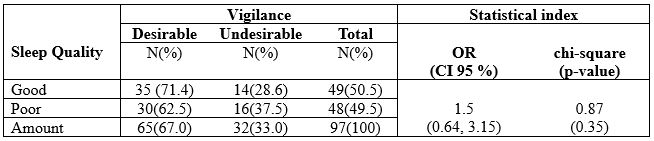
Table 3. The Correlation Between Sleep Quality and Vigilance Among Nurses undergoing Shift
The results of statistical tests obtained a p-value = 0.35, so it can be concluded that there was not a
significant relationship between sleep quality and vigilance among nurses who undergoing a shift in
the hospital.
DISCUSSION
Statistically it was found that in this study, there was no relationship between sleep quality and nurses' work alertness, although descriptively it can be reported that Nurses with good sleep quality tend to have good vigilance, and contrarily, nurses who have poor sleep quality tend to have less vigilance (see table 3). It significantly affects the productivity of nurses at work, where nurses in carrying out their work with good vigilance will work with good performance compared to nurses who are less alert.
Nurses who work night and rotating hours have been proven to have more trouble staying awake on duty and make twice as many mistakes as those who work day and evening shifts. More than 20% of workers in industrialized countries work shifts, and about 10% of them are diagnosed with sleep disorders [37]. Many factors affect sleep quality, one of which is shift work. Individuals who work shifts or shifts have difficulty adjusting to changing sleep schedules [6].
Poor sleep quality mainly occurs in nurses who use shift work systems. A study by Murphy et al., [38] found that shift work was significantly associated with poor sleep quality after controlling for variables of age, gender, and length of work.
This study also found almost the same proportion of respondents between respondents who had good and bad sleep quality, while most of the respondents had the desired of vigilance, which was around 67%. A systematic review study conducted by Dall’Ora et al. [39] found that shift characteristics are related to employee performance, and having sufficient rest time positively affects employee vigilance. Furthermore, Wahyuni [40] found a decrease in vigilance in night shift nurses with a proportion of decreased vigilance of 71.1%. However, statistically, it was not proven
to have a significant effect. The factor that influences the level of alertness before office hours is the
sleep quality. Lack of sleep results in a person's condition is less energetic and not enthusiastic [41].
We report that research data show that nurses predominately have a sleep latency of 1-2 hours, and only a small proportion (7.2%) have a sleep latency of 5-6 hours. Sleep latency is the length of sleep from start to fall asleep [42,43]. One of the factors that can affect sleep latency is bedtime habits that can disrupt a person's sleep and have an impact on increasing sleep latency [44].
This result is in line with the results of a previous study [45] that most respondents (60.3%) shift nurses experienced sleep disturbances less than once a week. Of all the sleep quality components, the sleep disturbance component had the highest mean of 1.44 with a standard deviation of 0.90 in a study of nurses undergoing shifts in Jordan [46].
Nurses’ poor sleep quality leads to a number of negative health outcomes. Nurses suffering from
poor sleep quality were more prone to develop burnout [47], depression and anxiety [48]. In addition, poor sleep could impair cognitive performance, such as concentration and memory, which may lead to poor work performance and even affect patients’ safety [49-51].
Effective measures, such as education on sleep hygiene [48], yoga [52] and cognitive-behavioral therapy for insomnia [53], should be considered to improve nurses’ sleep quality, quality of life, and patients’ safety.
CONCLUSION
The current study found that sleep quality was not a significant factor contributing to nurses' vigilance and medical error. Nevertheless, we still suggest that hospital managers should apply a 15-30 minute rest period during work shifts for nurses and pay attention to work rotation times, especially night shifts as a strategy to increase vigilance to prevent fatigue, sleepiness, and work errors.
LIMITATION OF STUDY
This study was only conducted in 3 hospital wards, so it cannot be compared with the same conditions in different hospitals. No intervention was carried out in this study to improve nurses' sleep quality and increase alertness while working. Other factors that influence Precautions, such as lighting conditions, environment, pills, caffeine, and other ingredients, were not studied.
Authors’ contribution
All authors equally contributed to preparing this article.
Acknowledgement
We express our gratitude to the director Director of Health Polytechnic, Ministry of Health Jambi, Indonesia for its support for the implementation of this research
Funding
This research received funding from the Development and Empowerment of Human Resources in Public Health (BPPSDMK) Indonesia
Conflict Of Interest
The authors declare that there was no conflict of interest in this research.
REFERENCES
- Deng X, Liu X, Fang R. Evaluation of the correlation between job stress and sleep quality in community nurses. Medicine. 2020;99(4).
- Boll J. Development of a Measure of Nurse Vigilance from the Patient’s Perspective: A Content Validity Study. 2014;
- Surani S, Hesselbacher S, Guntupalli B, Surani S, Subramanian S. Sleep quality and vigilance differ among inpatient nurses based on the unit setting and shift worked. Journal of patient safety. 2015;11(4):215–20.
- Kaliyaperumal D, Elango Y, Alagesan M, Santhanakrishanan I. Effects of sleep deprivation on the cognitive performance of nurses working in shift. Journal of clinical and diagnostic research: JCDR. 2017;11(8):CC01.
- Sayilan AA, Kulakaç N, Uzun S. Burnout levels and sleep quality of COVID-19 heroes. Perspect Psychiatr Care. 2020;57(3):1231–6.
- PA Potter AP. Fundamental Keperawatan. Jakarta: EGC; 2006.
- Tsai J-C, Chou K-R, Tsai H-T, Yen Y-C, Niu S-F. Effects of nocturnal sleep quality on diurnal cortisol profiles and attention in nurses: A cross-sectional study. Biological Research for Nursing. 2019;21(5):510–8.
- Di Muzio M, Diella G, Di Simone E, Pazzaglia M, Alfonsi V, Novelli L, et al. Comparison of Sleep and Attention Metrics Among Nurses Working Shifts on a Forward-vs Backward-Rotating Schedule. JAMA network open. 2021;4(10):e2129906–e2129906.
- Rainbow JG, Drake DA, Steege LM. Nurse health, work environment, presenteeism and patient safety. Western journal of nursing research. 2020;42(5):332–9.
- Smith-Miller CA, Shaw-Kokot J, Curro B, Jones CB. An integrative review. The journal of nursing administration. 2014;44(9):487–94.
- Asakura K, Asakura T, Satoh M, Watanabe I, Hara Y. Health indicators as moderators of occupational commitment and nurses’ intention to leave. Japan Journal of Nursing Science. 2020;17(1):e12277.
- Austin S, Fernet C, Trépanier S, Lavoie‐Tremblay M. Fatigue in new registered nurses: A 12‐month cross‐lagged analysis of its association with work motivation, engagement, sickness absence and turnover intention. Journal of nursing management. 2020;28(3):606–14.
- Bazazan A, Dianat I, Rastgoo L, Zandi H. Relationships between dimensions of fatigue and psychological distress among public hospital nurses. Health promotion perspectives. 2018;8(3):195.
- Han K, Trinkoff AM, Geiger-Brown J. Factors associated with work-related fatigue and recovery in hospital nurses working 12-hour shifts. Workplace health & safety. 2014;62(10):409–14.
- Fisman DN, Harris AD, Rubin M, Sorock GS, Mittleman MA. Fatigue increases the risk of injury from sharp devices in medical trainees results from a case-crossover study. Infection Control & Hospital Epidemiology. 2007;28(1):10–7.
- Barker LM, Nussbaum MA. Fatigue, performance and the work environment: a survey of registered nurses. Journal of advanced nursing. 2011;67(6):1370–82.
- Steege LM, Drake DA, Olivas M, Mazza G. Evaluation of physically and mentally fatiguing tasks and sources of fatigue as reported by registered nurses. Journal of Nursing Management. 2015;23(2):179–89.
- Reinke L, Özbay Y, Dieperink W, Tulleken JE. The effect of chronotype on sleepiness, fatigue, and psychomotor vigilance of ICU nurses during the night shift. Intensive care medicine. 2015;41(4):657–66.
- Geiger-Brown J, Rogers VE, Trinkoff AM, Kane RL, Bausell RB, Scharf SM. Sleep, sleepiness, fatigue, and performance of 12-hour-shift nurses. Chronobiology international. 2012;29(2):211–9.
- Ruggiero JS, Redeker NS, Fiedler N, Avi-Itzhak T, Fischetti N. Sleep and psychomotor vigilance in female shiftworkers. Biological research for nursing. 2012;14(3):225–35.
- Sun Q, Ji X, Zhou W, Liu J. Sleep problems in shift nurses: A brief review and recommendations at both individual and institutional levels. Journal of Nursing Management. 2019;27(1):10–8.
- Maurits LS, Widodo ID. Faktor dan Penjadualan Shift Kerja. Teknoin. 2008;13(2):18–22.
- Dong H, Zhang Q, Sun Z, Sang F, Xu Y. Sleep disturbances among Chinese clinical nurses in general hospitals and its influencing factors. BMC Psychiatry. 2017;17(1):1–9.
- Dorrian, J., Roach, Gregory.D., Fletcher, A., Dawson D. Simulated train driving: Fatigue, self awareness and cognitive disengagement. Applied Ergonomics. 2007;
- Desai A V., Haque MA. Vigilance monitoring for operator safety: A simulation study on highway driving. Journal of Safety Research. 2006;37(2):139–47.
- Zeng L-N, Yang Y, Wang C, Li X-H, Xiang Y-F, Hall BJ, et al. Prevalence of poor sleep quality in nursing staff: a meta-analysis of observational studies. Behavioral sleep medicine. 2020;18(6):746–59.
- Tu Z, He J, Zhou N. Sleep quality and mood symptoms in conscripted frontline nurse in Wuhan, China during COVID-19 outbreak: A cross-sectional study. Medicine. 2020;99(26).
- Arimura M, Imai M, Okawa M. Sleep, Mental Health and Errors in Nurses. Industrial health. 2010;48(6):811–7.
- Balas MC, Casey CM, Scott LD, Rogers AE. Maintain vigilance in the ICU. Nursing2020 Critical Care. 2007;2(4):38–44.
- Boughattas W, El Maalel O, Chikh R Ben, Maoua M, Houda K, Braham A, et al. Hospital night shift and its effects on the quality of sleep, the quality of life, and vigilance troubles among nurses. International Journal of Clinical Medicine. 2014;2014.
- Wang Y, Mei H, Jiang Y-R, Sun W-Q, Song Y-J, Liu S-J, et al. Relationship between duration of sleep and hypertension in adults: a meta-analysis. Journal of Clinical Sleep Medicine. 2015;11(9):1047–56.
- Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. European heart journal. 2011;32(12):1484–92.
- Alimoradi Z, Lin C-Y, Broström A, Bülow PH, Bajalan Z, Griffiths MD, et al. Internet addiction and sleep problems: A systematic review and meta-analysis. Sleep medicine reviews. 2019;47:51–61.
- Gómez-García T, Ruzafa-Martínez M, Fuentelsaz-Gallego C, Madrid JA, Rol MA, Martínez-Madrid MJ, et al. Nurses’ sleep quality, work environment and quality of care in the Spanish National Health System: observational study among different shifts. BMJ open. 2016;6(8):e012073.
- Kang J, Noh W, Lee Y. Sleep quality among shift-work nurses: A systematic review and meta-analysis. Applied nursing research. 2020;52:151227.
- Buysse DJ, Reynolds III CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry research. 1989;28(2):193–213.
- Basent B. Shift-work sleep disorder. New England Journal of Medicine. 2005;353(5):519–21.
- Murphy R, Osterweil D, MscED CMD, Spivack BS, Zee PC. Improving Sleep Management in the Elderly. Citeseer; 2010.
- Dall’Ora C, Ball J, Recio-Saucedo A, Griffiths P. Characteristics of shift work and their impact on employee performance and wellbeing: A literature review. International journal of nursing studies. 2016;57:12–27.
- Wahyuni I, Dirdjo MM. Hubungan Kelebihan Waktu Kerja dengan Kelelahan Kerja dan Kinerja pada Perawat di Ruang Perawatan Intensif RSUD Abdul Wahab Sjahranie Samarinda. Borneo Student Research (BSR). 2020;1(3):1715–24.
- Budiawan W, Prastawa H, Kusumaningsari A, Sari DN. Pengaruh Monoton, Kualitas Tidur, Psikofisiologi, Distraksi, Dan Kelelahan Kerja Terhadap Tingkat Kewaspadaan. J@Ti Undip : Jurnal Teknik Industri. 2016;11(1).
- Rocha MCP da, Martino MMF De. Stress and sleep quality of nurses working different hospital shifts. Revista da Escola de Enfermagem da USP. 2010;44:280–6.
- Fietze I, Knoop K, Glos M, Holzhausen M, Peter JG, Penzel T. Effect of the first night shift period on sleep in young nurse students. European journal of applied physiology. 2009;107(6):707–14.
- Mubarok. Buku Ajar Kebutuhan Dasar Manusia : Teori & Aplikasi dalam Praktik. Jakarta: EGC; 2007.
- Safitrie A, Ardani MH. Studi Komparatif Kualitas Tidur Perawat Shift dan Non Shift di Unit Rawat Inap dan Unit Rawat Jalan. Prosiding Konferensi Nasional PPNI Jawa Tengah. 2013;17–23.
- Suleiman K, Al-Khaleeb T, Al-Kaladeh M, Sharour LA. The Effect of Shift Fluctuations on Sleep Quality among Nurses Working in the Emergency Room in Amman, Jordan. International Journal of Occupational Safety and Health. 2020;10(1):11–7.
- Giorgi, F., Mattei, A., Notarnicola, I., Petrucci, C., & Lancia, L. Can sleep quality and burnout affect the job performance of shift-work nurses? A hospital cross-sectional study. Journal of Advanced Nursing, 2018; 74, 698–708. doi:10.1111/jan.13484
- Baroni, A., Bruzzese, J. M., Di Bartolo, C. A., Ciarleglio, A., & Shatkin, J. P. Impact of a sleep course on sleep, mood and anxiety symptoms in college students: A pilot study. Journal of American College Health, 2018; 66, 41–50. doi:10.1080/07448481.2017.1369091
- Barbe, T., Kimble, L. P., & Rubenstein, C. Subjective cognitive complaints, psychosocial factors and nursing work function in nurses providing direct patient care. Journal of Advanced Nursing, 2018; 74, 914–925. doi:10.1111/ jan.13505
- Caruso, C. C. Negative impacts of shiftwork and long work hours. Rehabilitation Nursing, 2014; 39, 16–25. doi:10.1002/rnj.107
- Park, E., Lee, H. Y., & Park, C. S. Association between sleep quality and nurse productivity among Korean clinical nurses. Journal of Nursing Management. 2018; doi:10.1111/jonm.12634
- Fang, R., & Li, X. A regular yoga intervention for staff nurse sleep quality and work stress: A randomised controlled trial. Journal of Clinical Nursing, 2015; 24, 3374–3379. doi:10.1111/jocn.12983
- Kalmbach, D. A., Cheng, P., Arnedt, J. T., Anderson, J. R., Roth, T., Fellman-Couture, C., … Drake, C. L. Treating insomnia improves depression, maladaptive thinking, and hyperarousal in postmenopausal women: Comparing cognitive-behavioral therapy for insomnia (CBTI), sleep restriction therapy, and sleep hygiene education. Sleep Medicine, 2019; 55, 124–134. doi:10.1016/j.sleep.2018.11.019
![]() This work is licensed under a Creative Commons
This work is licensed under a Creative Commons
Attribution-NonCommercial-NoDerivatives 4.0 International License.
DEVELOPMENT AND EFFECTIVENESS OF AUGMENTED REALITY-BASED LEARNING FOR HEALTH SCIENCE STUDENTS: A SYSTEMATIC REVIEW
Lia Artika Sari1, Muhammad Rusdi2, Asrial2, Herlambang2
1 Doctorate student in Education MIPA Jambi University, Indonesia
2 Jambi University, Indonesia
Corresponding author: Lia Artika Sari Jl. Prof DR GA Siwabessy No.42, Buluran Kenali, Kec. Telanaipura, Kota Jambi, Jambi 36122, Indonesia, Tel: +6282196687959, Email: liaartikasari57@gmail.com, Orcid : https://orcid.org/0000-0002-5285-5356
Cita questo articolo
ABSTRACT
Background and Objective. The rapid development of technology makes it easier for teachers to continue to be interactively connected with students, for example, by using Augmented Reality technology. We conducted this review intending to investigate the diffusion and the effectiveness of AR technology as a learning media for students from various health fields.
Materials and Method. This systematic review was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols) Checklist. We used some databases including PubMed, Google Scholar, Wiley Online Library, and Sciencedirect to search relevant literature with eligibility criteria, namely articles published in the period 201-2021, and discuss the development of Augmented Reality -based applications for learning students in the field of health
Results. The studies included are on the development of AR-based learning applications carried out to improve the clinical skills of health students (Medicine, Nursing, and Midwifery). Various types of application development are carried out including anatomy, Endotracheal Intubation, AR Prototype for Medical Surgery, Intravascular Neurosurgery, injection skills, and Laparoscopic.
Conclusion. The use of Augmented Reality as a learning medium really helps improve the understanding and skills of students majoring in health sciences.
Keywords: Development, Augmented Reality, Health-Science, Students
INTRODUCTION
The use of technology in the education of health science students has evolved over the years. These trends are mainly evolving in response to the challenges facing health education [1]. The use of simulation in health education has been applied in the last 50 years [2]. Augmented reality technology is an example of virtual reality technology developing rapidly in nursing education [3].
Augmented Reality (AR) technology refers to virtual elements to display the actual physical environment to create mixed-reality files in real-time. It complements and enhances the perceptions that humans acquire through their senses in the real world [4]. AR provides various levels of understanding and interaction, which can help students in e-learning activities [5]. For example, in an AR learning environment, motivational factors related to attention and learning satisfaction are rated higher than slide-based learning [6]. Today's development of smartphone technology makes AR technology more accessible to students and lecturers; for example, mobile learning (m-learning) using AR has become a trend [7].
Simulations using AR technology can replicate real-world aspects so that a safe learning environment is available for students where they can practice until the expected skill competencies are achieved [8]. Simulation has become an integral part of nursing curricula [9], which involves using patient simulators, trained people, real-life virtual environments, and role play [10].
Technological advances over time have increased the realism and authenticity of the simulated environment, leading to increased reactions, satisfaction, learning attitudes, cognitive and affective outcomes among health students in general [11].
Clinical health services have also used AR because it provides an internal picture of the patient, without the need for invasive procedures [12–15]. Medical students and professionals need more situational experience in clinical care, especially for patient safety, so this shows that there is a real need to continue developing the use of AR in health education.
The focus of studies on AR in recent years [16,17] has highlighted the belief that AR provides medical students with rich contextual learning to help achieve core competencies, such as decision making, work for effective teams, and creative adaptation of global resources to address local priorities [18], AR provides more authentic and engaging learning opportunities for various learning styles, providing students with a more personalized and exploratory learning experience [19]. The security of the patient will also be awake if an error occurs during skills training with AR [20].
Objective
This review was conducted to describe the development of AR technology as a learning medium for students from various health fields. This study is expected to be a reference material for teachers in learning strategies.
METHOD
Review Protocol
The research design is a Systematic Review, using the PRISMA-P 2009 (Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols) Checklist.
Searching strategy
To search for literature using the PubMed database, Google Scholar, Wiley Online Library, and Sciencedirect using the keywords "Developing" AND "Augmented Reality" AND "Clinical practice" AND (Medical OR Nurse OR Midewifery) "College student".
We categorize the search into five categories that are considered to represent the topic of Augmented Reality development, namely AR typology, AR features and advantages, AR user perceptions, AR effectiveness in supporting learning, and AR design. Each category was analyzed to identify the best lessons, experiences, and evidence related to the design and development of AR.
Eligibility Criteria
The articles included in this review use the development method, with the subject of the trial being health students. In addition, the articles used are in English and full text, published in the period 2010–2020. Furthermore, the data obtained are then analyzed using quantitative descriptive methods and a narrative is produced that explains the study results.
The study results were documented to identify the effectiveness of using augmented reality in student health learning.
Study Type
The studies included in the criteria for this review are only limited to studies on the development
of Augmented Reality technology for student learning in the health sector. Articles entered are in English, full text, and is not a thesis or dissertation.
Type of Participant/Population Target
The participants used were health students (Medicine, Nursing, Midwifery) who did clinical practicum (Clinical Skill). There are no restrictions on age, gender, level/semester, as long as participants do clinical practicum learning (clinical skills).
Article Quality
Quality assessment was carried out on six journals that met the inclusion and exclusion criteria using the JBI Critical Appraisal Checklist criteria. Journals are good if they meet at least 80%, moderate if they meet 50–80% and weak if they meet less than 50% of the criteria. Articles are used in good to moderate categories for further data synthesis, namely, grouping similar extracted data according to the results to be measured to conclude.
RESULTS
Literature Identification and Selection
There were 319 articles identified from four databases (Pubmed, Google Scholar, ScienceDirect, and Wiley Online Library) relevant to the review topic, where the assessment or screening was based on the title and abstract of the articles obtained. 66 studies were removed because they were duplicate. After screening the title and abstract, 219 studies were removed due to irrelevant theme, not AR topic, and proceeding types. At the eligibility stage, 28 studies were not fit the inclusion criterias.
Critical Appraisal
Based on the JBI Critical Appraisal Checklist, six pieces of literature are in the excellent category, and two pieces of literature are in the weak category.
To maintain the quality of the literature studies made, this review only uses six good-quality journals, and then data extraction will be carried out (Figure 1).

Figure 1. PRISMA Flowchart: Strategy for Searching for Development of Augmented Reality in Educational Situations for Health-Science Students
After bearing the assessment, screening, and feasibility, the authors agreed to include six studies in this systematic review of the literature. Furthermore, the extraction of data from each of the included literature we describe in the following table displays the critical information needed with the theme of the study.
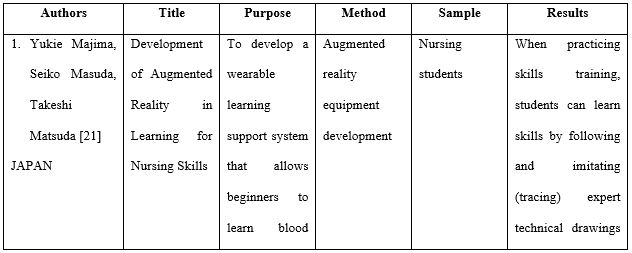
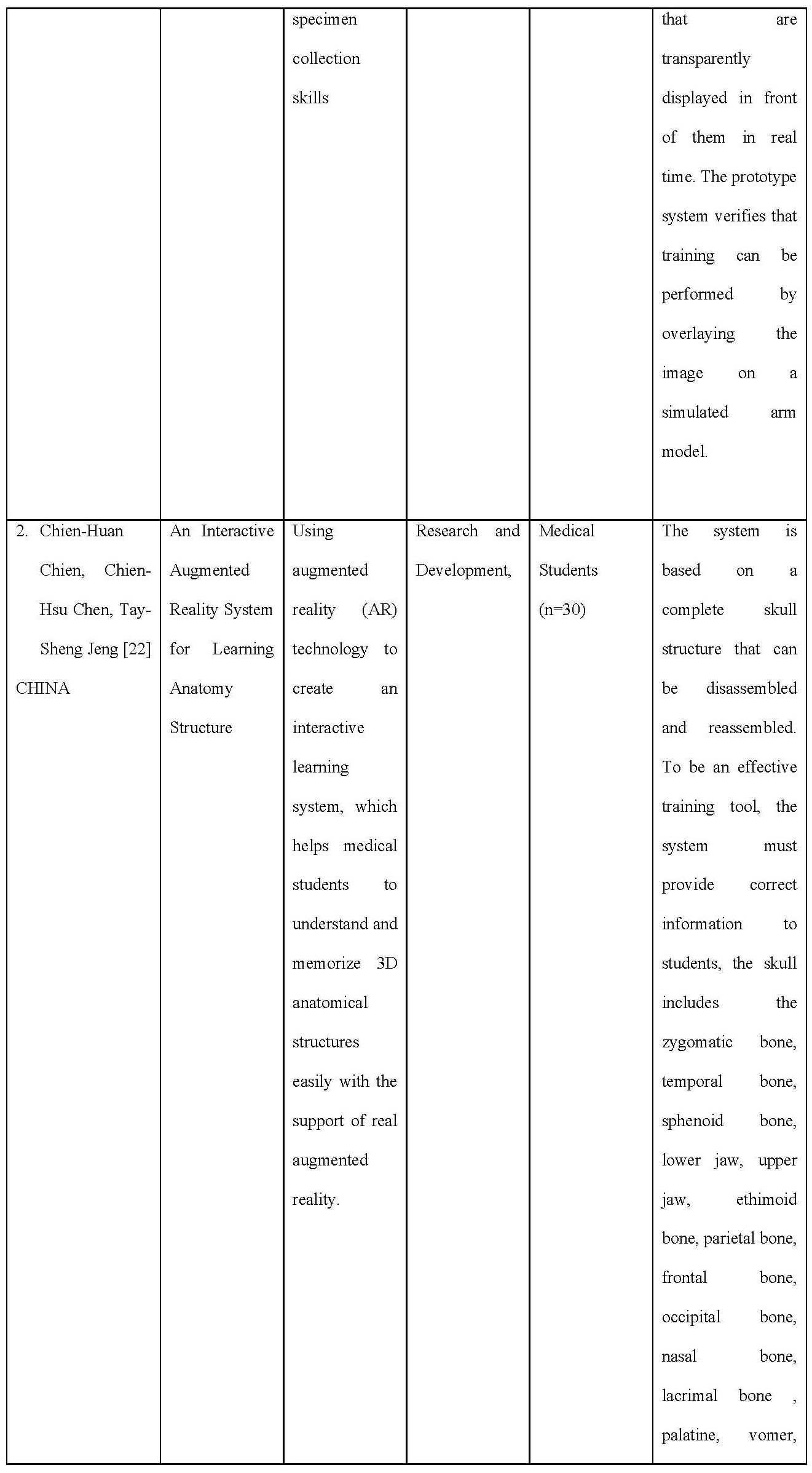


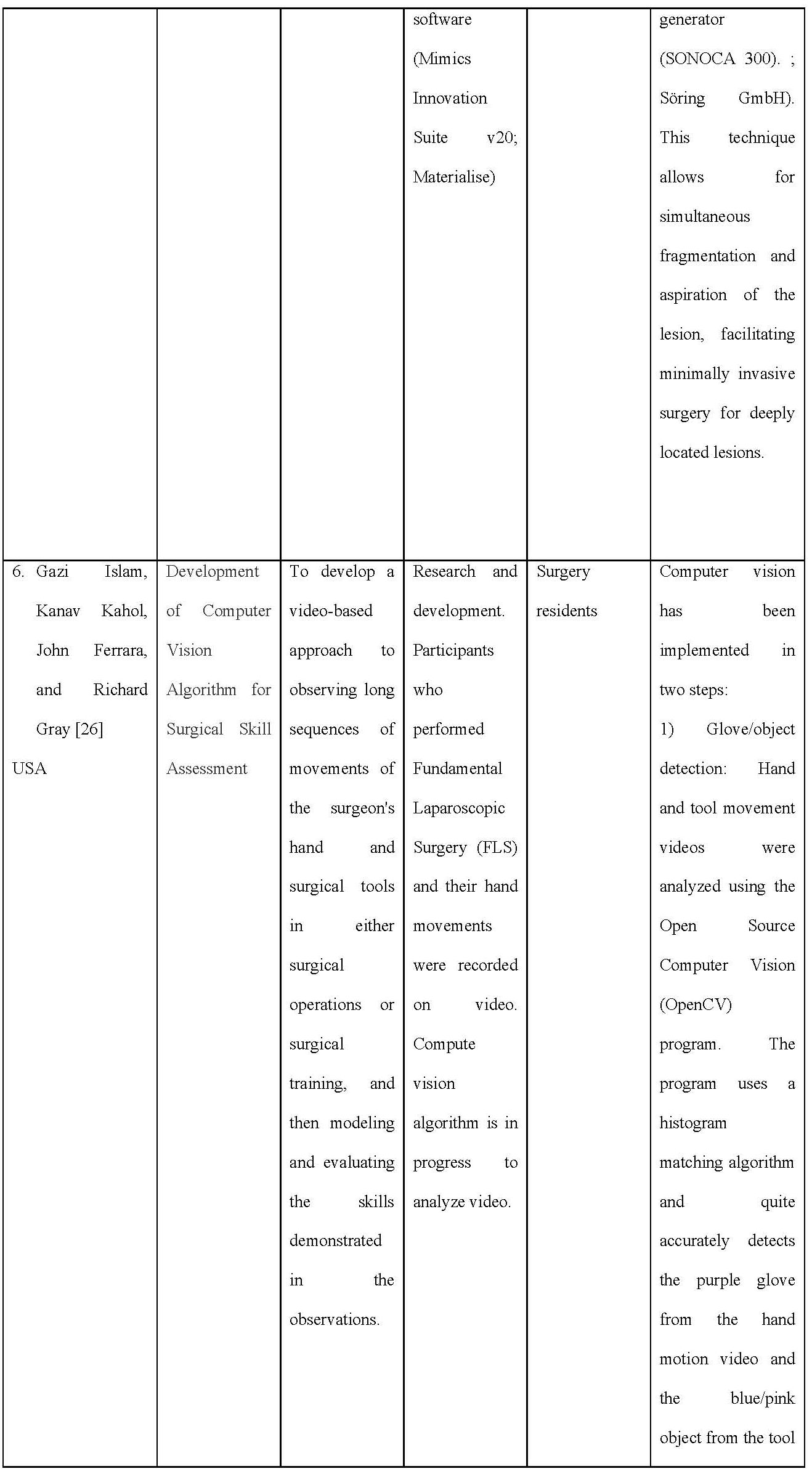

Table 1. Data Extraction on Included Articles
Characteristics of the studies included
The articles included in the inclusion criteria were six from several countries, including the USA as many as two articles, Canada 1 article, Sweden 1 article, Ireland 1 article, and Japan 1 article. Overall, the article taken is a study on the development of AR-based learning applications carried out to improve the clinical skills of health students (Medicine, Nursing, and Midwifery). Various types of application development are carried out including anatomy, Endotracheal Intubation, AR Prototype for Medical Surgery, Intravascular Neurosurgery, injection skills, and Laparoscopic.
Critical Appraisal
Based on the JBI Critical Appraisal Checklist, six pieces of literature are in the excellent category, and two pieces of literature are in the weak category. To maintain the quality of the literature studies made, this review only uses six good-quality journals, and then data extraction will be carried out.

Table 2. Summary of Critical appraisal based on JBI checklist
AR system design
In Majimas’ work, the learners can learn experts’ nursing skills without moving their lines of sight. When practicing skills training, learners can learn skills by following and imitating (tracing) the images of experts’ techniques that are dis-played transparently in front of them in real time. The prototype system verified that training is possible by overlaying images on a simulation arm model.
Chien and colleague The system is based on a complete structure of the skull which can be decomposed and reassembled. To be an effective training tool, the system has to provide correct information to the students, the skull includes zygomatic bone, temporal bone, sphenoid bone, mandible, maxilla, ethimoid bone, parietal bone, frontal bone, occipital bone, nasal bone, lacrimal bone, palatine, vomer, and inferior nasal concha.
Torregrosa and team developed an ARBOOK which includes a standard part of descriptive anatomy of the lower limb including osteology, arthrology, myology, nerve and vascular supply. Each part of the book includes bi-dimensional images and text about the muscles: origin insertion, vascular and nerve supply or action. It also includes a card for each anatomical figure that can be recognized by a digital webcam connected to a computer. The users can modify the actual position of the virtual structure by moving the card. To develop the ARBOOK, more than 100 TC images were needed and the images were processed by OsiriX software and 3D constructed. LabHuman and VMV3D companies performed the animation.
Drapkin study, an open-source T1 and T2 weighted simulated MRI dataset of a normal human brain constructed from a composite of 27 volumetric datasets of the same living subject was obtained from the BrainWeb simulated brain database. This dataset was viewed using GEHC MicroView software, version 2.1.2 (General Electric Healthcare, Little Chalfont, Buckinghamshire, UK). 3D models were constructed using MicroView to create isosurfaces based on gray scale values within a given region of interest to create a 3D mesh approximating the shape of a given internal brain structure. These computer graphic object composites were exported as a VTK PolyData file and edited using Maya software, version 2010 (Autodesk, San Rafael, CA) and were examined by two neuroanatomists and one neurologist for accuracy and compared to the Netter’s Atlas of Human Neuroscience. The final edited versions were imported back into MicroView 2.1.2 as Wavefront OBJ files and overlaid on top of the original MRI dataset. The final product was a set of digital 3D models of internal brain structures that can be freely rotated and zoomed by the user. To fabricate the 3D-printed models in Licci study, anonymized CT data set of a patient with enlarged CSF spaces was first downloaded from the picture archiving and communication system (PACS) and further processed with the medical segmentation software Materialise Mimics (Mimics Innovation Suite v20; Materialise). The DICOM CT data set consisted of native cross-sectional slices of bone and soft-tissue windows to display the relevant anatomical features. Further processing and segmentation of several anatomical structures according to tissue density (Hounsfield units) was worked out. The virtual cranial vault was designed with the help of the modeling software Materialise 3-Matics to be removable and equipped with realistic, neurosurgical burr holes for endoscopic access. The osseous skull was printed completely (2 parts) with a consumer Replicator+ 3D printer (MakerBot Industries) from polylactic acid (PLA; light gray), and the corresponding ventricle spaces were divided into 2 parts with a wall thickness of 3 mm in transparent PLA material. After printing a total of 5 skull models, the support structures were manually removed, and the two halves of the ventricular system were glued together. These were inserted into the skull model, and the cavity between the ventricular system and the bony skull was filled with 2-component silicone for stabilization.
In the Islam study, they proposed a novel video-based approach for observing continuous, long sequence of surgeon’s hand and surgical tool movements in both surgical operation or surgical training, and then modeling and evaluating the skill demonstrated in the observation. Hand movement of entire surgical procedure is captured using inexpensive video camera. Video data of the tool movement can also be obtained for minimal invasive surgery (MIS). Both of the video data are analyzed using computer vision algorithm and then integrated to correlate with user’s skill level.
For modeling the surgical skill, a stochastic approach is proposed that uses simple arithmetic mean and standard deviation of the processed data. Using this technique, observer-independent models can be developed through objective and quantitative measurement of surgical skills. Because of the non-contact nature of the tracking technique, the system is free from sterile issue and there is minimal interference with the skill execution, unlike other methods that employ instrumented gloves or sensor-based surgical tools.
AR for Nursing skills
There is one study that developed the teaching skills of nurses using AR technology. The skill learned in the study was performing intravenous injections [21].
AR for Anatomy learning
Three studies [22] developed learning methods based on AR technology. AR technology was used to create an interactive learning environment, which allows students to understand the 3D skull structure with visual support [14]. One of the studies gave their app the name ARBOOK, which can be presented in both, printed or electronic version. ARBOOK includes a standard part of descriptive anatomy of the lower limb including osteology, arthrology, myology, nerve and vascular supply [15]. Another study developed 3D Neuroanatomy Teaching Tool. The models were created of the ventricular system, thalamus, hypothalamus, pituitary gland, hippocam-pus, amygdala, fornix, caudate, putamen, globus pallidus, brainstem, cerebral peduncles, and cerebellar peduncles [16].
AR for Surgical training
There are two studies that develop training based on AR technology. The first study involved a neuroendoscopic ventricular lesion removal training [17], and the second study provided two laparoscopic graspers and performed the pegboard transfer exercise on the FLS [18].
DISCUSSION
It is undeniable that the advancement of Augmented Reality technology has had a significant impact on the health sciences. Professions requiring high precision and good psychomotor abilities certainly require more time to practice carrying out their actions. The presence of Augmented Reality technology in its various forms is proven to increase students' abilities and interests in dealing with the learning process.
Under certain conditions, especially during pandemic times where large-scale restrictions are imposed, direct meetings to carry out laboratory practicums are deemed possible, so there must be changes in strategies or effective learning methods for students in dealing with curriculum demands related to learning outcomes. A total of 6 eligible articles have been extracted to provide an overview of the development of Augmented Reality technology-based tools/tools in many health science fields, including Medicine, Nursing,/Midwifery. From the article, the discussion will be described based on the field of development, software and hardware used,
Development area
Anatomy Learning
Two articles develop applications for learning body anatomy based on Augmented Reality [18]. Tried to develop a 3D interactive learning environment of bone structure with visual support. This application is equipped with pop up labels and interactive displays in 3D to make it easier for users to see the position of each bone at various angles. In addition, users are also facilitated with the help of each label with information about the bone so that students no longer need to open books to look for information about the designated bone. To use this 3D application, students/users need hardware devices such as laptops/PCs equipped with cameras and pointers. For testing this device, Chien and colleagues used 30 medical students who had never taken anatomy courses to hope that the participants' responses to this application would be of better quality. At the evaluation stage, participants revealed that the developed application was fascinating because it could provide a complete picture of the displayed bone structure and explain each pop-up label, making it easier to understand and memorize. In addition, another exciting thing is that the reassembled function in the application allows students to see the inner structure of the bone.
Another application developed by Torregrosa and colleagues in 2014 called ARBOOK (Augmented Reality Book) focuses on the anatomical structure of the lower extremities. For its development, 100 TC photos/images are needed, then the images are processed using OsiriX software and 3D object creation. For validation, the questionnaire compiled for the ARBOOK evaluation consists of the categories of task motivation and attention, autonomous work, comprehensive spatial orientation, and 3D interpretation. . Next, an expert assessment will be carried out. Application testing involves first-year health students who have never taken an anatomy course. The test results show a significant difference between learning using ARBOOK and conventional learning. As has been stated in previous studies that the use of virtual materials in anatomy learning can provide good benefits for student learning achievement, especially regarding motivation and independence [27,28].
Augmented Reality technology was also developed in Neuroanatomy learning for MRI exercises developed by Drapkin and colleagues in 2015. The developed application makes the brain image display into a 3D shape. This 3D model begins by using MicroView to form a primary image in the form of isosurfaces and then form a 3D model similar to the shape of the actual brain. The graph is then exported in VTK PolyData file format and edited using Maya software. The editing results are then given to neuroanatomists and neuroscientists to assess the accuracy of the image shape and compared with images on the ATLAS neuroscience Netter. The final image is then placed on top of the actual brain image from the MRI. Next, we entered the pilot phase, which was conducted on participants who were medical students at level 1. The trials showed that this 3D neuroanatomy teaching tool effectively trains medical students to read brain MRI and effectively teach students to identify internal brain structures.
Surgery training
In contrast to learning the body's anatomical structure, surgical skills in surgery require hand-eye coordination, which can be achieved with continuous practice [29]. In surgery, one is not enough to see what other people are doing when performing surgery; that is, to become skilled, it is necessary to "watch and do" [30].
One of the six articles included in this review is an Augmented Reality-based simulation development study for Neuroendoscopic Ventricular Removal exercises [25]. In this development study, a 3D-printed model of synthetic body tissue was created. The idea is based on the limited material for practical surgery such as tumour removal. By using this 3D-printed model, it is hoped that it can accommodate all residents to do exercises repeatedly because this model is reusable.
Overall, the surveyed participants agreed or strongly agreed (Likert scores of 4 and 5) on the realistic nature of the anatomical model of the skull and ventricular system, the technical suitability of the model, the camera view, which was similar to the actual surgical view. Participants also agreed or strongly agreed that the content validity of the simulator is a valuable tool for enhancing surgical competence for neuro-endoscopic procedures that helps develop coordinating skills and represent an excellent practical exercise tool for ventricular tumour removal.
Other Augmented Reality-based surgical simulations are also included in this study. The development study conducted by Islam et al. [26] aims to create a video-based approach to observing surgeon hands and surgical instrument movements in surgery and surgical training. The data is captured with a video camera and then explored using a computer vision algorithm. Furthermore, by analyzing the basic statistical parameters, observer-independent performs objective and quantitative measurements of the surgical skills of the trainees. Computer vision is done through two steps, namely Glove/object detection and motion capture. This application is very suitable for remote assessment of student skills. Between the rater and the assessed, it is possible not to be in the room together; this allows the assessed participants to be calmer in the face of the assessment. Students can also receive virtual and interactive demonstrations of surgical procedures with surgeons carrying out the surgery so that students can experience real situations in the operating room.
Nursing skills
Majima, et all [21] developed a practicum learning system for nursing students based on Augmented Reality, especially in the act of taking blood specimens. In certain types of blood vessels, beginners find it difficult to insert the needle. It is the basis for this research. Through this development, beginners can learn the "art" in the veins and imitate the images displayed in front of them. In injection skills education, both instructors and students are usually very interested in holding a syringe. However, in reality, the teaching given is limited to fixation, and the left finger technique is taught, which is tailored to the characteristics of each patient's blood vessels that are difficult to insert a needle. How to repair and lengthen unstable blood vessels has not been entirely taught.
When practising skills training, students can learn skills by following and imitating (tracing) expert technical drawings transparently displayed in front of them in real-time. The prototype system verifies that training can be performed by overlaying the image on a simulated arm model.
CONCLUSION
The use of Augmented Reality as a learning medium really helps improve the understanding and skills of students majoring in health sciences. The many choices of models in application development provide opportunities for researchers to continue to innovate. Augmented Reality-based learning applications in the future become an absolute thing along with the increasing development of technology.
Limitation
Many databases not used in this review, such as Scopus, Ebsco, IEEE, and others, are very
credible for searching literature/articles. It is due to limited access to these databases. The use of gray literature such as google scholar conducted carefully with agreement of all authors.
The author also has limitations in understanding the software and programming languages used in the articles reviewed, so the authors cannot further discuss the application development process in the six articles reviewed.
Recommendation
This study provides a broad overview of the Augmented Reality-based application development process so that it can be a reference material for future teachers or researchers to be able to innovate in the development of Augmented Reality-based learning applications, for example, in the process of guiding final project students, or multiplying nursing action tutorials that are currently available. Not yet fully available in the form of an Augmented Reality application.
Funding
This systematic review does not get funding.
Conflict of Interest
The author declares there is no conflict of interest in this study.
REFERENCES
- Birt J, Stromberga Z, Cowling M, Moro C. Mobile mixed reality for experiential learning and simulation in medical and health sciences education. Information. 2018;9(2):31.
- Jones F, Passos-Neto CE, Braghiroli OFM. Simulation in medical education: brief history and methodology. Principles and practice of clinical research. 2015;1(2).
- Foronda CL, Alfes CM, Dev P, Kleinheksel AJ, Nelson Jr DA, O’Donnell JM, et al. Virtually nursing: Emerging technologies in nursing education. Nurse educator. 2017;42(1):14–7.
- Arena F, Collotta M, Pau G, Termine F. An Overview of Augmented Reality. Computers. 2022;11(2):28.
- Chiang THC, Yang SJH, Hwang G-J. Students’ online interactive patterns in augmented reality-based inquiry activities. Computers & Education. 2014;78:97–108.
- Di Serio Á, Ibáñez MB, Kloos CD. Impact of an augmented reality system on students’ motivation for a visual art course. Computers & Education. 2013;68:586–96.
- Khan T, Johnston K, Ophoff J. The impact of an augmented reality application on learning motivation of students. Advances in Human-Computer Interaction. 2019;2019.
- Jeffries PR. A framework for designing, implementing, and evaluating: Simulations used as teaching strategies in nursing. Nursing education perspectives. 2005;26(2):96–103.
- Aebersold M, Voepel-Lewis T, Cherara L, Weber M, Khouri C, Levine R, et al. Interactive anatomy-augmented virtual simulation training. Clinical simulation in nursing. 2018;15:34–41.
- Scalese RJ, Issenberg SB. Effective use of simulations for the teaching and acquisition of veterinary professional and clinical skills. Journal of veterinary medical education. 2005;32(4):461–7.
- Hamacher A, Kim SJ, Cho ST, Pardeshi S, Lee SH, Eun S-J, et al. Application of virtual, augmented, and mixed reality to urology. International neurourology journal. 2016;20(3):172.
- Bajura M, Fuchs H, Ohbuchi R. Merging virtual objects with the real world: Seeing ultrasound imagery within the patient. ACM SIGGRAPH Computer Graphics. 1992;26(2):203–10.
- Cameron C. How augmented reality helps doctors save lives. Read Write Web. 2010.
- De Paolis LT, Ricciardi F, Dragoni AF, Aloisio G. An augmented reality application for the radio frequency ablation of the liver tumors. In: International Conference on Computational Science and Its Applications. Springer; 2011. p. 572–81.
- Pandya A, Siadat M-R, Auner G. Design, implementation and accuracy of a prototype for medical augmented reality. Computer Aided Surgery. 2005;10(1):23–35.
- Rolland JP, Biocca F, Hamza-Lup F, Ha Y, Martins R. Development of head-mounted projection displays for distributed, collaborative, augmented reality applications. Presence: Teleoperators & Virtual Environments. 2005;14(5):528–49.
- Sielhorst T, Obst T, Burgkart R, Riener R, Navab N. An augmented reality delivery simulator for medical training. In: International workshop on augmented environments for medical imaging-MICCAI Satellite Workshop. 2004. p. 11–20.
- Frenk J, Chen L, Bhutta ZA, Cohen J, Crisp N, Evans T, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. The lancet. 2010;376(9756):1923–58.
- Parmaxi A, Demetriou AA. Augmented reality in language learning: A state‐of‐the‐art review of 2014–2019. Journal of Computer Assisted Learning. 2020;36(6):861–75.
- Kobayashi L, Zhang XC, Collins SA, Karim N, Merck DL. Exploratory application of augmented reality/mixed reality devices for acute care procedure training. Western Journal of Emergency Medicine. 2018;19(1):158.
- Majima Y, Masuda S, Matsuda T. Development of Augmented Reality in Learning for Nursing Skills. In: MEDINFO 2019: Health and Wellbeing e-Networks for All. IOS Press; 2019. p. 1720–1.
- Chien C-H, Chen C-H, Jeng T-S. An interactive augmented reality system for learning anatomy structure. In: proceedings of the international multiconference of engineers and computer scientists. International Association of Engineers Hong Kong, China; 2010. p. 17–9.
- Ferrer-Torregrosa J, Torralba J, Jimenez MA, García S, Barcia JM. ARBOOK: Development and assessment of a tool based on augmented reality for anatomy. Journal of Science Education and Technology. 2015;24(1):119–24.
- Drapkin ZA, Lindgren KA, Lopez MJ, Stabio ME. Development and assessment of a new 3D neuroanatomy teaching tool for MRI training. Anatomical sciences education. 2015;8(6):502–9.
- Licci M, Thieringer FM, Guzman R, Soleman J. Development and validation of a synthetic 3D-printed simulator for training in neuroendoscopic ventricular lesion removal. Neurosurgical focus. 2020;48(3):E18.
- Islam G, Kahol K, Ferrara J, Gray R. Development of computer vision algorithm for surgical skill assessment. In: International Conference on Ambient Media and Systems. Springer; 2011. p. 44–51.
- Fairén M, Moyés J, Insa E. VR4Health: Personalized teaching and learning anatomy using VR. Journal of medical systems. 2020;44(5):1–11.
- Pringle RM, Dawson K, Ritzhaupt AD. Integrating science and technology: Using technological pedagogical content knowledge as a framework to study the practices of science teachers. Journal of Science Education and Technology. 2015;24(5):648–62.
- Rao A, Tait I, Alijani A. Systematic review and meta-analysis of the role of mental training in the acquisition of technical skills in surgery. The American Journal of Surgery. 2015;210(3):545–53.
- Herrlin S V, Wange PO, Lapidus G, Hållander M, Werner S, Weidenhielm L. Is arthroscopic surgery beneficial in treating non-traumatic, degenerative medial meniscal tears? A five year follow-up. Knee Surgery, Sports Traumatology, Arthroscopy. 2013;21(2):358–64.
![]() This work is licensed under a Creative Commons
This work is licensed under a Creative Commons
Attribution-NonCommercial-NoDerivatives 4.0 International License.
KNOWLEDGE AND ATTITUDES BETWEEN NURSES, MIDWIVES AND STUDENTS ABOUT VOLUNTARY TERMINATION OF PREGNANCY: A SCOPING REVIEW OF THE LITERATURE
Sofia Di Mario1, Andrea Minciullo2 & Lucia Filomeno3*
- RN, MSN, PhD Student; Department of Public Health and Infectious Diseases, Sapienza University of Rome, Piazzale Aldo Moro 5, 00185, Rome, Italy.
- RN, MSN, Gastroenterology and Digestive Endoscopy Unit, Campus Bio-Medico, 00128, Rome, Italy,
- RN, MSN, PhD Student; AOU Policlinico Umberto I – Department of Neurosciences and Mental Health, Viale dell’Università, 30, 00185, Rome, Italy.
* Corresponding author: Lucia Filomeno, Department of Neurosciences and Mental Health, AOU Policlinico Umberto I, Rome. E-mail: lucia.filomeno@uniroma1.it
Cita questo articolo
ABSTRACT
Background: Voluntary termination of pregnancy (VTP) is influenced by ethical convictions, religious orientations and knowledge of the law. The latter is essential for students to be improved in University curricula, in order to develop attitudes among future nurses and midwives with the objective to reduce stigma and reluctance in providing VTP. Previous research has shown that nursing and midwifery students' attitudes and knowledge can be improved.
Aim: The aim of this study is to describe literature regarding knowledge and perception about abortion and voluntary termination of pregnancy in several countries of the world among nurses, midwives and university students.
Methods: This is a scoping review of the literature conducted by following the recommendations of the PRISMA-ScR Statement. The authors selected studies in MEDLINE, Scopus, CINAHL, PsycINFO, Academic Search Index, Science Citation Index and ERIC, published in English and Italian in the last decade. Quality assessment was performed using the Jadad scale.
Results: Initially, 434 studies were selected. A total of 11 articles met the inclusion criteria. The articles included in the scoping review deal with the issue of abortion from different perspectives. From the analysis it emerged that the barriers for VTP are the lack or inadequate knowledge of the legislation and of the practical / technical phases of the procedure.
Conclusions: Health professionals and students have different perspectives and attitudes toward VTP. Nurses and midwives have inadequate knowledge of procedures and legislation. Therefore, it is recommended to implement university curricula on the topic.
Keywords: knowledge, attitudes, voluntary termination of pregnancy, nurses, midwives, students.
INTRODUCTION
Abortion, originated as birth control, is the termination of pregnancy before 20 weeks of gestation or with the foetus weight less than 500 gr at birth [1,2]. It can happen when at least three events occur: spontaneous or habitual abortion (also called Voluntary Termination of Pregnancy - VTP), criminal or illegal abortion, and therapeutic or legal abortion [3]. In the last decades of the 20th century, many countries all over the world legalised this practice. The World Health Organization (WHO) states that 3 out of 10 (29%) of all pregnancies, and 6 out of 10 (61%) of all unintended pregnancies, ended in an induced abortion [4]. In many societies, a deep conflict about the legality and morality of abortions manifests itself in restrictive laws and strong antiabortion attitudes. Women, including adolescents, with unwanted pregnancies often resort to unsafe abortion when they cannot access a safe one. Barriers to accessing safe VTP include: restrictive laws, poor availability of services, high cost, stigma, conscientious objection of health-care providers and unnecessary requirements, such as mandatory waiting periods, mandatory counselling, provision of misleading information, third-party authorization, and medically unnecessary tests that delay care [5,6]. Kumar et al. [7], defined abortion stigma as “a negative attribute ascribed to women who seek to terminate a pregnancy that marks them, internally or externally, as inferior to the ideals of womanhood”. According to this definition, women who experience VTP challenge social norms regarding female sexuality and maternity, and their doing so elicits stigmatising responses from the community. Where opposition to abortion is widespread, abortion-related stigma is likely to negatively influence women’s abortion experience.
Increased knowledge and improved attitudes among health care providers and university students have the potential to reduce stigma and reluctance to provide abortion [6]. In a recent study conducted by O'Shaughnessy et al. [8], it was reported that “low levels of knowledge among staff suggests that training is required to ensure the provision of a safe and effective VTP service”. Midwifery and Nursing schools do not provide termination of pregnancy education or, if they do, it is inadequate and so, most staff were left to navigate this procedure without support or prior practice.
Termination is only possible in the rarest of cases: when the pregnancy poses a serious risk to the woman’s life or in the event of foetal malformations [7]. In Italy, as in many countries, it is set at 12 weeks’ gestation according to the law No. 194 enacted on May 22nd, 1978. Before that date, VTP was considered illegal by the criminal code [9]. The law regulates VTP with the aim of guaranteeing the bio-psycho-social integrity and well-being of women. A woman can have an abortion within the first 90 days, or within the fourth and fifth months only for therapeutic reasons [9]. Conscientious objection status does not exempt the professional from assisting the woman before and after the procedure, but from carrying out only those procedures directed towards and aimed at the termination [10-13]. The nurse can raise a conscientious objection to assisting the VTP with a declaration that can be withdrawn at any time [9]. Termination is a woman’s right, and the staff involved must act in accordance with the law and the woman’s right to free choice. A better understanding of factors influencing perceptions may be useful in determining the curricula of university programs and in giving nurses and midwives the tools to cope with their own beliefs towards late abortions [14-16]. Thus, this review seeks to contribute to research on abortion stigma by exploring literature regarding attitude, knowledge and perception differences toward abortion among nursing, midwifery and students, assessing the scientific evidence available to date and thereby delineating directions for future research.
METHODS
Identification of Relevant Studies
A scoping review was chosen as the research methodology [17]. This supports what is referred to as a systematic approach to the synthesis of evidence, helping to identify gaps for future studies. In this case, the goal is to determine the strength of the evidence using a consistent best practice approach. The search of the international literature was conducted in accordance with the PRISMA-ScR Statement (PRISMA extension for Scoping Reviews)[18] and was conducted within some main databases of biomedical interest: MEDLINE, Scopus, CINAHL, PsycINFO, Academic Search Index, Science Citation Index and ERIC. The review was carried out from October 2021 to February 2022. The keywords used were “knowledge; attitude; perception; nurse; student; abortion; midwife and questionnaire”. The latter were useful in formulating the research question according to the PCC (Population, Concept and Context) methodology (Table 1).

Table 1. Clinical research question identified through the PCC methodology
Study Selection and Eligibility Criteria
Research question: “What are the differences in knowledge and attitudes between nursing and midwifery staff and the corresponding university students?”. The search string was created using the Boolean operators (AND and OR), the terms MeshTerms and the truncation function, to ensure maximum search sensitivity and specificity:
(Knowledge OR Attitude OR Perception) AND (Abortion) AND (Nurse OR Midwife OR Student) AND (Questionnaire OR Assessment)
The study population were nurses, midwives and nursing and midwifery students. The primary studies concerning the assessment of attitudes, perceptions and knowledge about abortion between the two groups and the efficacy and validity of these arguments within the degree programs were considered eligible. The studies included experimental or quasi-experimental studies and observational studies. Since grey literature (i.e., unpublished conference proceedings or theses or dissertations) was not considered, other potentially relevant studies were not included in this review.
The selection criteria listed below were met to identify suitable studies for the purpose of this review.
Inclusion criteria
- Literature from the last 10 years.
- Italian or English language.
- Experimental and observational studies: RCT (Randomised Controlled Trial), quasi-experimental research designs, pretest-posttest, cross-sectional.
- Nurses, midwives and corresponding university students.
Exclusion criteria
- Other healthcare professionals, physicians, medical students or students of other healthcare professionals.
- Grey
- Qualitative and mixed-methods studies.
Data Extraction
In the first phase, the results obtained from the research were imported into a software for the management of bibliographic references and duplicates were eliminated. In the second phase, each article uploaded to the database was carefully and independently examined. Initially, they were analysed by reading their title and abstract and, according to the previously established eligibility criteria, the irrelevant ones were excluded, while those relevant for full-text reading were selected. Thanks to the in-depth reading, it was possible to exclude the articles that did not answer the research questions. Two reviewers worked independently. The following data was collected for each article: study title, first author, year of publication, study sample and study design, objective, assessment and a summary of the results. The approach used to group the articles was thematic: the main objective of the thematic analysis is to identify similar concepts in the collected dataset, exploring their relationships of meaning. These reports can be used to further develop and corroborate the interpretation of theories that seek to investigate the phenomena studied [19].
Quality Assessment
The quality of the studies was assessed usingthe Jadad Scale [20], focusing on methods for random allocation, double blinding, and withdrawals and dropouts. Total scores ranged from 0 to 5 points, where studies with 0-2 points were considered poor quality and those with 3-5 points represented high-quality evidence [20].
RESULTS
Initially, 434 articles were selected with duplicates removed (Figure1). Of these, 11 met the inclusion criteria and underwent the review process. The main information of the relevant articles was organised in a data extraction table (Table 2). Studies were conducted in 11 different countries: Belgium, Ghana, Iran, Brazil, Israel, Spain, Ethiopia, Finland, Canada, Pakistan and South Korea. This demonstrates a notable absence of literature in Italy. The studies included a sample ranging from a minimum of 74 to a maximum of 647 participants. The most recent one dates to 2020, while the oldest one dates to 2010. From the analysis it emerged that the barriers for abortion treatment are the lack or inadequate knowledge of the legislation and of the practical / technical phases of the intervention [21-24]. The possession of skills is often not enough as in the study by Romina et al. [22] where it emerged that there was no significant relationship between the knowledge of the law and the care performance of health professionals while a statistically significant relationship was observed between their opinion of abortion and their active collaboration[22].

Figure 1. - PRISMA 2020 flow diagram for new systematic reviews which included searches of databases and registers only.
Personal and religious beliefs have been considered to have a profound influence on opinion and behaviour, in some cases resulting in the inability to take care of the patient for fear of remorse [21; 25-27]. The presence of moral and / or religious values in health workers was significantly correlated with the occurrence of the request for conscientious objection (CO) [21-26].



Table 2. Data Extraction Table.
In South Korea, where about half of the population declared themselves irreligious, Chung Mee Ko et al. [26] assessed the opinions of 167 nurses regarding CO; the majority replied that patients’ rights to health care should take priority over nurses’ right to refuse health care, concluding that the nursing profession should seriously consider whether it is necessary to insist on nurses’ right to CO and should be actively involved in the determination process of new abortion laws and related policies [26]. Nieminen et al. [6] studied CO among Finnish nursing students and practitioners. Most of them seemed to consider the continuation of adequate services to patients in the event of the introduction of CO as crucial, while emphasising the surgical act over patient support. Despite their views and beliefs, health workers sometimes faced a conflict with their commitment to care; in the work of Ben Natan et al. [15], they stated that bioethical dilemmas, as well as the reasons for abortion, influenced their ability to actively collaborate during the termination of pregnancy [15]. Nurses attitude and ability to actively participate in late abortions were found to be strongly conditioned by the level of religious observance [21-22]. The study by Roets et al. [28] found that in several neonatal intensive care units in Belgium, healthcare workers practicing late abortion had a high degree of tolerance towards late termination of pregnancy, regardless of the patient’s socio-demographic factors, so much so that they asked the institutions to provide for a change in legislation [28].
Ben Natan et al. [15], however, found that nursing students had more prejudices towards late abortions than experienced nurses, evidence in line with the study conducted by Assefa et al. [24] where it turned out that a predictor of a positive attitude towards VTP was seniority [24]. The role of health workers is very important, especially on a psychological level, even more so when they must help women to deal with a negative event such as a miscarriage. To this end, Engel et al. [27] suggested that health workers should receive specific training to be able to support women and their families [27]. Previous research has shown that university education programs do not provide the tools necessary to achieve the objectivity required in preparation for abortion and that this may have contributed to anti-abortion attitudes and misconceptions about legal regulations that are common among students10. Same results emerged from the work of Baig et al. [29] who studied the knowledge, attitudes and practices of midwives in post-abortion care services [29]. The work highlighted the need to provide comprehensive training and mentoring to midwives and students, building strong networks to enable the development of broader initiatives to reduce the stigma of abortion.
DISCUSSION
Although the total number of studies investigating abortion stigma among undergraduate students and nurses and midwives such as nurses and midwives is low, results indicate that knowledge, personal and religious beliefs significantly affect attitudes about VTP. This is in line with the findings by Madziyire et al. [10] where incomplete comprehension of abortion laws highlights the urgent need for providers education as a key step in reducing stigma and mortality associated with unsafe abortion [10]. Additionally, the lack of expertise evidenced by most of the studies, suggest that even nurses and midwives who have good intentions may unwittingly disseminate misinformation. One study underlined the fact that type of profession and seniority were important in providers’ knowledge about abortion. Also, being male and having high knowledge significantly influenced providers’ attitude. The same findings were highlighted by Hammarstedt et al. [30] who stated that gynaecologists and midwives were less restrictive towards legal abortion the more experience they had, being especially influenced by recently obtained experience within the last year [30]. Claims of conscientious objection must be ethically justified, and not become a strategy to hide prejudices or fear of lawsuits and moral accusations. Such an instrument cannot be an obstacle for women to have access to abortion [31]. Humanized care in the abortion process is part of the reproductive and sexual rights of women, and ensuring it is a duty of all health professionals.
Abortion laws and practice differ between cultures, religions and countries. The Finnish healthcare system is relatively liberal regarding the right for induced abortion until the 12° gestational week. Despite lively discussion, there is no legislation in this country on the possibility of CO [32]. Post-abortion care is important especially in countries like Pakistan, where half of pregnancies are unintended. Demand for abortions is high in Jamaica, but many doctors refer clients to another provider. Patient assessment is good, but support services need improvement [33]. This has been reported in other surveys in other countries. In Ghana, for example, only 45% of surveyed physicians said that they would perform abortions, whereas another 36% said that they would provide counselling prior to abortion but not the procedure itself [33]. Women deserve a well-prepared, informed personnel and similarly, students deserve a thoughtfully inclusive curriculum that accurately addresses ethical topics, as most programs do not require sexual health courses as a part of their curriculum [34-35].
CONCLUSION
The role of the health professional assisting the woman who decides to undergo a voluntary termination of pregnancy is very important, especially in the phases before and after the intervention. Assistance must always be provided with respect for the woman’s dignity, confidentiality and freedom of choice. Nurses need to provide a source of support for the woman by establishing a relationship based on trust. Health professionals and students have different perspectives and attitudes toward VTP. Nurses and midwives have inadequate knowledge of procedures and legislation. It is important that the health professional realises the crucial importance of their role in the woman’s grieving process to ensure good care.
Limitations of the study
Our study has some limitations that should be mentioned. In our analysis, only research articles published in English and Italian were included, which may have produced a language bias regarding the conclusion, as some scientific papers were published in other languages. Additionally, only studies published in peer-reviewed journals were included; this criterion was meant to ensure reporting quality but may mean that relevant grey literature was missed.
Practical implication
Nurse sneed to have adequate training in the bereavement context: they should know what interventions implement and what to avoid. The aim of the scoping review was to analyze the international panorama regarding abortion as a point of departure on which to develop an Italian study to compare legislation knowledge, attitudes and perspective differences among students and nurses and midwives. Therefore, it is recommended to implement university curricula on the topic.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
The authors declared no conflict of interest.
REFERENCES
- Lobo RA, Gershenson DM, Lentz GM, Valea FA. Comprehensive gynecology E-book. Elsevier Health Sciences, 2016.
- Echeverría BC, Serani MA, Arriagada U AM, Goic G A, Herrera CC, Quintana VC, et al. An ethical and medical perspective on the voluntary termination of pregnancy. 2015;143(11):1478–83. https://doi.org/10.4067/S0034-98872015001100014
- Narayan KS, Reddy M. Essentials of Forensic Medicine and Toxicology. JAYPEE Brothers MEDICAL P, 2017.
- World Health Organization. (2021). Access to medical abortion medicines in the South-East Asia Region-a status report.
- Bearak J, Popinchalk A, Ganatra B, Moller A-B, Tunçalp Ö, Beavin C, Kwok L, Alkema L. Unintended pregnancy and abortion by income, region, and the legal status of abortion: estimates from a comprehensive model for 1990–2019. Lancet Glob Health. 2020 Sep; 8(9):e1152-e1161. https://doi.org/10.1016/S2214-109X(20)30315-6
- Nieminen P, Lappalainen S, Ristimäki P, Myllykangas M, Mustonen A-M. Opinions on conscientious objection to induced abortion among Finnish medical and nursing students and professionals. BMC Medical Ethics. 2015 Mar 25;16(1):17. https://doi.org/10.1186/s12910-015-0012-1
- Kumar A, Hessini L, Mitchell EMH. Conceptualising abortion stigma. Culture, Health & Sexuality. 2009;11(6):625–39. https://doi.org/10.1080/13691050902842741
- O’Shaughnessy E, O’Donoghue K, Leitao S. Termination of pregnancy: Staff knowledge and training. Sexual&Reproductive Healthcare. 2021 Jun1;28:100613. https://doi.org/10.1016/j.srhc.2021.100613
- Italiana R. Legge 22 maggio 1978, n. 194. Norme per la tutela sociale della maternità e sull’interruzione volontaria della gravidanza. Gazzetta Ufficiale, 22. https://www.gazzettaufficiale.it/eli/id/1978/05/22/078U0194/sg
- Madziyire MG, Moore A, Riley T, Sully E, Chipato T. Knowledge and attitudes towards abortion from health care providers and abortion experts in Zimbabwe: a cross sectional study. Pan AfrMed J. 2019 Oct16;34:94. https://doi.org/10.11604/pamj.2019.34.94.18107
- Aragaw Y, Sinishaw W, Daba W, Mekie M. Attitude of Nursing and Midwifery students towards clinical practice and its associated factors in Northwest Ethiopia: a cross-sectional study. BMC Research Notes. 2019 Apr 3;12(1):205. https://doi.org/10.1186/s13104-019-4230-3
- Jafari H, Khatony A, Abdi A, Jafari F. Nursing and midwifery students’ attitudes towards principles of medical ethics in Kermanshah, Iran. BMC Medical Ethics. 2019 Apr 25;20(1):26. https://doi.org/10.1186/s12910-019-0364-z
- Biggs MA, Casas L, Ramm A, Baba CF, Correa SP. Medical and midwifery students’ views on the use of conscientious objection in abortion care, following legal reform in Chile: a cross-sectional study. BMC Medical Ethics. 2020 May 24;21(1):42. https://doi.org/10.1186/s12910-020-00484-4
- Glenton C, Sorhaindo AM, Ganatra B, Lewin S. Implementation considerations when expanding health worker roles to include safe abortion care: a five-country case study synthesis. BMC Public Health. 2017 Sep 21;17(1):730. https://doi.org/10.1186/s12889-017-4764-z
- Ben Natan M, Melitz O. Nurses’ and nursing students’ attitudes towards late abortions. Int Nurs Rev. 2011 Mar;58(1):68–73. https://doi.org/10.1111/j.1466-7657.2010.00840.x
- Harries J, Stinson K, Orner P. Health care providers’ attitudes towards termination of pregnancy: A qualitative study in South Africa. BMC Public Health. 2009 Aug 18;9(1):296. https://doi.org/10.1186/1471-2458-9-296
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology. 2005 Feb 1;8(1):19–32. https://doi.org/10.1080/1364557032000119616
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Annals of Internal Medicine. 2018 Sep 4;169(7):467–73. https://doi.org/10.7326/m18-0850
- Allodola V.F. Metodi di ricerca qualitativa in MedicalEducation: Approcci, strumenti e considerazioni di rigore scientifico. Educ. Sci. Soc. 2014, 5, 121–144.
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996 Feb;17(1):1–12.https://doi.org/10.1016/0197-2456(95)00134-4
- De Roose M, Tency I, Beeckman D, Van Hecke A, Verhaeghe S, Clays E. Knowledge, attitude, and practices regarding miscarriage: A cross-sectional study among Flemish midwives. 2018 Jan;56:44–52. https://doi.org/10.1016/j.midw.2017.09.017
- Romina S, Alamshahi M, Moafi F, Mafi M, Hajnasiri H. Relationship of Knowledge and Attitude Towards Legal Abortion Laws with the Performance of Midwives in Qazvin, Iran. Health, Spirituality and Medical Ethics. 2019 Jun 10;6(2):17–23. http://dx.doi.org/10.29252/jhsme.6.2.17
- Cacique DB, Passini Junior R, Duarte Osis MJM, Oliveira HC, Padilha KM, Tedesco RP, et al. Perspectives of healthcare workers on the morality of abortion: a multicenter study in seven Brazilian public hospitals. Health Care Women Int. 2020 Jul;41(7):761–76. https://doi.org/10.1080/07399332.2019.1672169
- Assefa EM. Knowledge, attitude and practice (KAP) of health providers towards safe abortion provision in Addis Ababa health centers. BMC Women’s Health. 2019 Nov 14;19(1):138. https://doi.org/10.1186/s12905-019-0835-x
- Voetagbe G, Yellu N, Mills J, Mitchell E, Adu-Amankwah A, Jehu-Appiah K, et al. Midwifery tutors’ capacity and willingness to teach contraception, post-abortion care, and legal pregnancy termination in Ghana. HumResour Health. 2010 Feb23;8:2. https://doi.org/10.1186/1478-4491-8-2
- Ko CM, Koh CK, Lee YS. An ethical issue: nurses’ conscientious objection regarding induced abortion in South Korea. BMC Med Ethics. 2020 Oct 27;21(1):106. https://doi.org/10.1186/s12910-020-00552-9
- Engel J, Rempel L. Health Professionals’ Practices and Attitudes About Miscarriage. MCN Am J Matern Child Nurs. 2016 Feb;41(1):51–7. https://doi.org/10.1097/nmc.0000000000000207
- Roets E, Dierickx S, Deliens L, Chambaere K, Dombrecht L, Roelens K, et al. Healthcare professionals’ attitudes towards termination of pregnancy at viable stage. Acta ObstetGynecolScand. 2021 Jan;100(1):74–83. https://doi.org/10.1111/aogs.13967
- Baig M, Jan R, Lakhani A, Ali S, Mubeen K, Ali S, et al. Knowledge, Attitude, and Practices of Mid-Level Providers regarding Post Abortion Care in Sindh, Pakistan. Journal of Asian Midwives (JAM). 2017 Jun 1;4(1):21–34.
- Hammarstedt M, Jacobsson L, Wulff M, Lalos A. Views of midwives and gynecologists on legal abortion--a population-based study. Acta ObstetGynecolScand. 2005 Jan;84(1):58–64. https://doi.org/10.1111/j.0001-6349.2005.00695.x
- Madeiro A, Rufino A, Santos P, Bandeira G, Freitas I. Conscientious Objection and Legal Abortion: Medical Students’ Attitudes. Rev bras educ med. 2016 Mar;40:86–92. http://dx.doi.org/10.1136/medethics-2013-101482
- Gissler M, Ulander VM, Hemminki E, Rasimus A. Declining induced abortion rate in Finland: data quality of the Finnish abortion register. Int J Epidemiol. 1996 Apr;25(2):376–80. https://doi.org/10.1093/ije/25.2.376
- Fletcher H, Gordon-Strachan G, McFarlane S, Hamilton P, Frederick J. A survey of providers’ knowledge, opinions, and practices regarding induced abortion in Jamaica. Int J Gynaecol Obstet. 2011 Jun;113(3):183–6. https://doi.org/10.1016/j.ijgo.2010.12.022
- Baba CF, Casas L, Ramm A, Correa S, Biggs MA. Medical and midwifery student attitudes toward moral acceptability and legality of abortion, following decriminalization of abortion in Chile. Sexual&Reproductive Healthcare. 2020 Jun1;24:100502. https://doi.org/10.1016/j.srhc.2020.100502
- Burnes TR, Singh AA, Witherspoon RG. Sex Positivity and Counseling Psychology: An Introduction to the Major Contribution. The Counseling Psychologist. 2017 May 1;45(4):470–86. https://doi.org/10.1177%2F0011000017710216
![]() This work is licensed under a Creative Commons
This work is licensed under a Creative Commons
Attribution-NonCommercial-NoDerivatives 4.0 International License.
NUTRITION EDUCATION MODELS IN PREGNANCY TO INCREASE KNOWLEDGE AND DIETARY PATTERNS: A SYSTEMATIC REVIEW
Suryani*1, Muhammad Rusdi1, Asni Johari1, Solha Elrifda1
- Post-Graduate Program of Mathematic and Natural Science Education College, Jambi University, Indonesia
Correspondence: Suryani, Address : Dr. Tazar Street, Buluran Kenali, Kec. Telanaipura, Kota Jambi, Jambi 36361, Indonesia, Email : suryanipoltekkes3@gmail.com, Orcid : 0000-0001-6540-2607
Cita questo articolo
ABSTRACT
Background. The misconception of nutritional principles causes dietary oversight, resulting in an excess or deficit of energy and specific nutrients essential for the proper course of pregnancy and a child's healthy growth. This review aims to evaluate the effectiveness of nutrition education in improving knowledge and dietary change conducted in pregnant women.
Methods. This review study complies with the 2009 PRISMA guidelines. The studies included in this review are mainly studies with experimental designs. Databases used in searching relevant literatures such as PubMed, ScienceDirect, Willey online Library, Web of Science, Cochrane, and Proquest that were published from 2010 to 2021, full text, English version, experimental studies. Two review authors conducted studies screening based on the eligibility criteria, and extracted important points in the studies included. Quality of the studies included were assessed using EPHPP.
Results. A total of 10 studies were identified in this review. Six studies in the high quality, and four studies in moderate quality. Overall outcomes of the studies included are Knowledge, Attitude, practice, dietary practice, awareness, hemoglobin blood level, and Gestational Weight Gain (GWG).
Conclusion. Nutrition education in many methods has a power to improve knowledge, and dietary change of pregnant women. It implies the need for future large high quality trials using a standardized approach to measuring and reporting similar findings across studies.
Keywords : Pregnancy, Pregnant women, Education, Nutrition
INTRODUCTION
Pregnancy is one of the most notable moments in a person's life, and at that time, diet is essential [1]. So far, maternal malnutrition or failure to meet nutritional needs has caused specific health problems for both mothers and newborns [2]. Due to insufficient and unbalanced nutrition, problems such as anemia, osteomalacia, and pregnancy toxemia often arise, and the chances of stillbirth in newborns, premature delivery, congenital abnormalities, and mental retardation increase [3,4]. Furthermore, poor maternal nutritional quality causes developmental maladaptation in the fetus [5]. This results in long-term structural, physiological and metabolic changes and an increased risk of cardiovascular, metabolic, and endocrine diseases in adults [6].
Poor eating habits are a leading contributor to the development of overweight and obesity across the world [7,8]. The frequency of home-cooked meals has decreased over the last five decades, while consumption of foods produced outside the house (i.e., fast food and restaurant food), often higher in calories, fat, and salt, has grown [9,10]. Consumption of home-cooked meals regularly is linked to better diet quality over the lifespan [11,12]. As a result, increasing the frequency of home-prepared meal intake is a significant health habit to target for preventing overweight and obesity in adults and children, and it has been the topic of extensive research over the last two decades [13,14].
International authorities define pregnancy as a moment of highly nutritional needs to promote mother and fetal growth [15]. Nutritional support needed in pregnancy includes carbohydrates, fiber, protein, and micronutrients, such as vitamin A, vitamin B complex folate, and iron [16]. However, a study in Canada found that people have insufficient micronutrients through food, such as high levels of iron (97 percent), vitamin D (96 percent), and folate (70 percent) intake [17]. Therefore, stakeholders intended to present food and nutrition education to encourage a balanced diet based on food culture's valorization [18]. Food and nutrition education is an essential strategy for upgrading health because it encourages people to identify and tolerate their cultural discrepancies and empowers them to complete decisions concerning their health care [19]. Antenatal nutrition education is related to better eating patterns and a healthier pregnancy [20]. Healthy fetal growth and development, cognitive capacity, and immunological function are promoted by optimal nutrition throughout pregnancy [21]. Pregnant women's adherence to dietary guidelines decreases due to a lack of nutrition expertise and insufficient information from health providers [22]. Before and during pregnancy, the mother's behavior becomes a determining factor for both the mother and her child [23,24]. Many dietary mistakes can be caused by a lack of understanding of nutritional principles, resulting in an excess or deficit of energy and specific nutrients essential for the proper course of pregnancy and a child's healthy growth [25,26]. Adequate diet, in combination with sufficient physical activity and the avoidance of harmful habits, enhances the chances of a healthy pregnancy [27,28]. One of the previous systematic reviews on pregnant women's compliance in following dietary guidelines during pregnancy stated that knowledge was an essential predictor concerning adherence to the given nutritional guidelines [29].
It is essential to assess how successful nutrition educations are in improving the nutritional status of pregnant women especially their knowledge and dietary.
This systematic review aimed to assess the efficacy of nutrition education in knowledge and dietary change during pregnancy and their implications for future research. Therefore, the question for this review is, "what kind of nutritional education model is good for increasing knowledge and changes in the diet of pregnant women?".
METHODS
Design
When reporting this systematic review, the standards outlined in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement were followed [30].
Eligibility Criteria
The participants, intervention, comparator, outcome, and study design (PICOS) criteria outlined in Table 1 were used to select studies for inclusion in this review.

Table 1. Studies Criteria based on PICOS
Type of Studies
The studies included in this review use experimental designs such as Randomized Controlled trials (RCT) and Quasi-experimental. Participants in the study should be pregnant women in any trimester of pregnancy.
Search Strategy
The following databases (platforms) were searched: PubMed, ScienceDirect, Willey online Library, Web of Science, Cochrane, and Proquest in the time frame between 2010 to 2021. We also searched the gray literature database for additional information such as Google Scholar, conference proceedings, and BASE. The keywords used are based on the Medical Subject Headings (MeSH) standard. Using Boolean operators and a combination of keywords used, namely: ((("pregnancy nutrition"[Title/Abstract]) OR ("pregnancy nutrition knowledge"[Title/Abstract])) AND ((("health education"[Title/Abstract]) OR ("nutritional education"[Title/Abstract])) OR ("health promotion"[Title/Abstract]))) AND (((("knowledge"[Title/Abstract]) OR ("attitude"[Title/Abstract])) OR ("practice"[Title/Abstract])) OR ("awareness"[Title/Abstract])).
Study selection
Two review authors independently assessed the titles and abstracts of the retrieved studies to see if they met the eligibility criteria (RUS and ASJ). The full-text publications for the remaining studies were obtained and evaluated for eligibility which obtained and read full texts of the studies that potentially met the inclusion criteria. The first ineligibility criterion from the following list determines why a publication was excluded: study design, population, intervention, and results. The first authors decided disagreements from review authors regarding the feasibility of the study (SUR and SOE), and this procedure was followed throughout the review.
Data Extraction and Quality Assessment
Two authors (SUR and SOE) independently extracted data in duplicate from studies that met the
inclusion criteria to avoid any chance of misinterpretation of conceptualizations in each study.
Data were synthesized in two ways: (1) research design and intervention strategies were presented. (2) the findings of each study were analyzed qualitatively by collecting the main findings with the design and intervention applied. Furthermore, data extraction was carried out to provide a brief description of the articles' substance, such as the characteristics of the respondents and the characteristics of the study. Data extracted included author, year, country, participant, study design, Intervention, outcome, and main findings. The researchers then examined each extraction and any discrepancies were discussed until consensus was reached.
The quality of the articles included was measured using an assessment tool for the Effective Public Healthcare Panacea Project (EPHPP) [31] which allows experts to apply this tool to articles on any public health topics. This tool uses STRONG, MODERATE, and WEAK categorizations based on the assessment results on eight components, namely Selection Bias, Study Design, Confounders, Blinding, Data Collection Methods, Withdrawals, and Drop-outs, Intervention Integrity, and Analyzes. Articles in the STRONG category are the article reached four strong from the EPHPP component without any of the components being considered weak, the MODERATE category if four components reach strong. One component is rated "weak," and for the WEAK category, it is given if two or more components reach a "weak" value.
Data synthesis
Data from the included studies could not be pooled for meta-analysis because to the substantial diversity in the methodological design of the investigations. Consequently, the narrative synthesis of the included study findings was provided using the Synthesis without Meta-analysis in Systematic Reviews: Reporting Guideline [32].
RESULTS
Search Results
The process of searching for articles up to the determination of articles that meet the inclusion requirements can be illustrated in Figure 1.

Figure 1. PRISMA Flowchart for Literature Search
Search results from five databases yielded 486 articles according to the keywords applied, and then 159 articles were eliminated because they were duplicates, leaving 327 articles. Furthermore, the screening stage was carried out on the remaining articles; as many as 295 articles were excluded because they did not discuss the nutrition status in pregnancy. At the end of the screening, ten articles met the inclusion criteria (Table 2). Those were included in the moderate and robust categories based on the EPHPP assessment tool for article quality assessment.



Table 2. Extraction of Literature Included
Description of studies included
The articles reviewed in this study are located in several countries such as Iran [37], Ethiopia [34], USA [41], Brazil [33], Palestine [36], and Somalia [39]. Study design including Randomized Controlled Trial (RCT) [33–35,38,39,42], and Quasy experimental [36],[37,40,41].
Characteristics of participants
All reviewed studies included pregnant women with variations in gestational age including below 36 weeks (Oliveira et al., 2018), below 16 weeks [34,35] below 20 weeks [41,42], 14-16 weeks [36], 6-10 weeks [38], 18 – 24 weeks [40], 14-20 [41]. Two studies were not applied the gestational age [37,39].
Description of interventions
Some studies provided booklet regarding Healthy Diet during Pregnancy [33], Counseling regarding dietary practice [34], Nutrition education (theoretical session, poster, brochures, flipchart, and whiteboard) [35,37,40], theoretical and practical [36], the nutrition‑education intervention based on Pender’s HPM [38], video health information [39], exercise, self-monitoring, facebook private group [41], web-based health information [42].
A booklet entitled “Healthy Diet during Pregnancy with Regional Foods (Alimentação Saudável na Gravidez com os Alimentos Regionais)” was used as the main intervention which contains the concept of healthy nutrition, allowed and avoided foods during pregnancy, the benefits of healthy dietary habits for mothers and babies, food hygiene, and recipes with regional foods. The intervention group participated in the individual intervention in a private room, in a single session, with an average duration of 20 minutes. During the meeting, the booklet was introduced, read, and the patients kept a copy to take home [33].
The counseling model has also been used in a study in Ethiopia. The intervention package was community-based guided counseling using the HBM and the TPB. The core content of counseling guide including meal frequency, portion size with increasing gestational age and taking diversified meals, consumption of iron/folic acid supplementation, iodized salt use, reducing of a heavy workload, taking day rest, use of impregnated bed nets, and health services. Counseling was given monthly using a counseling guide and leaflets with core contents. Individual Nutrition counseling was given through a home visit on non-working days. Each counseling session lasted for 40 to 60 minutes. Participants attended four counseling sessions during pregnancy. The first counseling was given before 16 weeks of gestation, the second and third counseling sessions were given during the second trimester of pregnancy, the fourth counseling was given during the early third trimester of pregnancy. The control group received nutrition education given by the health system [34].
Nutrition education intervention recorded in three studies was given to pregnant women between 1 and 4 months at baseline. The education was given every 15 days for 5 consecutive months. For intervention group, education intervention was given based on Health Belief Model theory: (1) susceptibility of the pregnant women and fetus to malnutrition due to inappropriate dietary practices nutrient deficiency or over nutrient intake; (2) severity of malnutrition such as wasting/thinness and overweight/obesity and high risk of fetus to intrauterine growth retardation, brain development, and cognitive function due to macro- and micronutrient deficiency; (3) benefits of right eating or dietary practices on women nutritional status and fetus health, (4) barriers to practice appropriate good dietary practices; and (5) self-confidence/efficacy to follow right dietary practices. The education was provided using theoretical session, poster, brochures, flipchart, and whiteboard. For the control group, nutrition education was given by trained community health volunteers based on the general usual nutrition education which is currently provided by health extension workers [35]. Fallah et al [37] conducted face-to-face nutritional education which contains two to four lessons based on a nutrition package by Iranian ministry of health. Another study by Shakeri [40] nutrition education conducted in groups of 12 people, held in 8 sessions each planned for three sections taking 90 minutes. An educational CD, educational booklet, tract, and pamphlet about the advantages of good nutrition for mothers and embryo, appropriate ways of doing activities during pregnancy, and false beliefs were given to the participants. Furthermore, lecture, question and answer, group discussion, and film screening methods were used to educate the patients. Paticipants in control group received the routine prenatal instructions [40].
The complementary nutritional intervention (CNI) program proposed by Al-Tell and colleague, it was developed based on the educational principles using the principles of health belief model that aimed to behavior change. The program composed of two parts that were presented within 16 hours and through 8 grouped sessions, in addition to another 2 individualized/ follow-up session for each woman. The content of the theoretical part consisted of 60% of program hours, and the practical part consisted of 40% of program hours. The study also used educational booklet for additional materials. It included information regard iron deficiency anemia in term of causes, complication, treatment inhibitors and promoters of iron absorption and examples of prepared meals rich of iron [36].
Khoigani and colleague conducted nutritional education based on the Pender’s HPM for intervention group, included three 45 – 60 minutes training sessions in 6 – 10, 18, and 26 weeks of pregnancy. Each participant had a meeting with the study nutritionist at the time of enrollment for nutritional assessment. In the first session, the dietary pattern, including the average daily servings of five food groups, was explained to the participants. In the second session, practical steps (goal‑setting techniques) to increase self‑efficacy [38].
Destephano et al evaluated the use of DVD to spread information about caesarean birth, episiotomy, nutrition and exercise, the father’s role, preparation and prevention, and pregnancy myths and facts. Each video topic ranged from 3 to 4 min in length, incorporated
traditional songs and poetry, and had English subtitles [39].
Baruth et al used the social cognitive theory to develop SELF intervention (Supporting hEaLthy Futures: Creating a Healthy Family by Investing in YourSELF). The intervention included four key components: Exercise is Medicine™, self-monitoring, opportunities for support, and walking groups (optional). In self monitoring, Participants were given a FitBit Charge to monitor their physical activity (daily) and an Eat Smart Precision digital scale (model ESBS-01) to monitor their weight. Participants were instructed to weigh themselves once a week using the scale provided, and enter their weight into their FitBit account [41].
Participants (control and intervention groups) in Olson et al [42] trials given access to the intervention website and to the placebo control website. The self-directed, integrated online and mobile phone behavioral intervention was designed using the Integrative Model of Behavior Prediction and the Behavior Model for Persuasive Design based on a non-electronic pregnancy lifestyle intervention. Participants in intervention group received access to three behavior change tools including a weight gain tracker, a diet and a physical activity goal-setting and self-monitoring tool, as well as, health information including tips, articles, frequently asked questions; a description of pregnancy and parenting-related resources available in the local community; a blogging tool; and an event and appointment reminder [42].
Quality Assessment
Assessment of the methodological quality of studies resulted in 6 studies with a high quality score [33–35,38,41,42] and 4 studies with a moderate quality score [36,37,39,40].
Description of Outcomes
Outcome measures reported in the included studies were Knowledge, attitude, practice [33–35,37,39,40], Dietary practices [34,35,38], Gestational Weight Gain (GWG) [41,43], behavior change [42], Hemoglobin blood level [36]. One study collected the result of outcomes measurement immediately after the intervention [39], Three studies conducted the evaluation in two times for 6 weeks [40], 5 months [36], and 8 months [42]. The rest of the studies evaluated the outcomes in the range of one to five months [33–35,37,38,41].
As mentioned in Oliveira et al study, the knowledge was considered adequate when used to prepare varied meals and/or juices, knew three or more types of regional foods, and mentioned at least two types of meals prepared with regional foods. The attitude was considered adequate when pregnant women prefer to use regional foods and know the advantages. The practice was considered adequate when pregnant women referred to use regional foods at least twice a day [33]. In Diddana study, knowledge measurement is based on the Health Belief Model consists of 15 nutrition question [35]. In Fallah study, Knowledge as a primary outcome was measured before the intervention and two posttests within three weeks interval [37]. Another study in Iran with knowledge and attitude as primary outcome completed the evaluation immediately and 6 weeks after the educational intervention for the samples of experimental and control groups [40].
For dietary practice outcome, assessment used a food frequency questionnaire (FFQ) collected between 36 to 37 weeks of gestation. Women who didn’t attend all counseling sessions were considered non-adherent to the guideline. But, women who withdraw from participating in the study were labeled as lost to follow up [34]. In Diddana study, dietary practice variable was collected by using 17 dietary habit questions [35].
DISCUSSION
Overview study included
This review provides evidence that interventions with a health education on pregnancy issue can improve pregnant women knowledge, attitude, practice, dietary pattern, awareness, hemoglobin level, and weight gain outcomes. There is somewhat more persuasive evidence that health education interventions are favorably linked with healthy living change during pregnancy of pregnant women as participants due to the number of RCTs that revealed significant findings. Because of the high variability of research designs and methodology utilized in the included papers, meta-analysis cannot be conducted. Furthermore, the goal of this evaluation was to serve as a first step in identifying evidence-based treatments that would help transfer prenatal nutrition research and guidelines into practice. Although the evidence highlighting the importance of nutritional status during pregnancy has been documented, and numerous practice guidelines, including the recently consolidated inter-professional practice guidelines, have existed for some time, there is still a significant gap in translating this evidence to pregnant women through health promotion efforts. Overall, there are few dietary promotion treatments during pregnancy, and only 10 interventions have been assessed on specified health outcomes, according to this analysis.
Overall, the studies comprised a wide range of pregnant women from six different nations, resulting in some findings. Furthermore, all of the research was done in a communal context. A previous evaluation noted that complete prenatal care treatments should be available in remote regions or with less infrastructure and that their duties and those of trained CHWs should be harmonized across nations to assure basic levels of care [44]. Pregnant women who did not take advantage of offered interventions, so missing out on the possibility of a better pregnancy outcome, exemplified the lack of access to services in remote regions [45].
We recommend that maternal and family health service managers at the national, state, and local levels devote resources to adapting and testing existing culinary nutrition programs or, as appropriate, developing new culinary nutrition programs tailored to these life stages, as a result of the potential benefits of culinary nutrition interventions during pregnancy and postpartum identified in this review. Culinary nutrition programs for pregnant or postpartum women might be incorporated into existing health education programs or offered separately. A workforce with culinary nutrition expertise in maternity and family health care would be required to support such initiatives.
Nutrition Education
For this group is included in the demographic group prone to nutrition and health concerns, nutrition education is crucial during pregnancy [46]. According to cross-sectional research, pregnant women's understanding of nutrition during pregnancy went from 53.9 percent to 97 percent after receiving nutrition education, while their pregnancy-specific dietary practices increased from 46.8 percent to 83.7 percent [47].
Besides knowledge, GWG is also an important issue to be discussed In both the short and long term, excessive GWG is linked to unfavorable health outcomes for mother and child health [48]. Excess GWG is linked to an increased risk of hypertensive disorders [49], glucose intolerance [50] and and poor delivery outcomes during pregnancy [51]. It also predicts more significant baby morbidity and fetal development, such as birth weight, big for gestational age, and macrosomia, among other things [52].
Olson et al., [42] In their experiment, a self-directed, integrated online and mobile phone behavior modification intervention failed to show a beneficial effect on the proportion of the sample with excessive total GWG when compared to an information-only placebo control condition (which is included in this review). It was most likely discovered because the intervention was self-directed. That may have been a wrong decision. Structured, personalized treatments were more likely to be successful in promoting dietary change, according to a recent assessment of the research on e-behavioral nutrition interventions [42].
One research included in this review, which focuses on the hemoglobin blood level as an outcome, was done in Palestine. Compared to the control group, the study found a substantial beneficial link between dietary behaviors and improved hemoglobin levels. Compared to the control group, there was also a good connection between maternal hemoglobin levels in the third trimester and tiredness levels in the study group [36]. According to review research, nutrition education such as counseling, web-based, and text messages may enhance pregnant women's adherence to iron supplements. The research also stressed the significance of a more extended trial period to assess the intervention's effectiveness correctly [53].
According to the World Health Organization, pregnant women who reside in areas with high nutritional deficits should get some primary nutritional treatment. Nutrition counseling on a healthy diet, energy and protein dietary supplements, iron and folic acid supplementation (all settings), calcium supplementation to reduce the risk of pre-eclampsia in settings where dietary calcium intake is low. Zinc supplementation is only recommended for pregnant women in the context of rigorous research, and multiple micronutrient supplementation is all recommended in settings where 20% or more of women are underweight. Nonetheless, in areas where nutritional shortages are common, several micronutrient supplements include iron and folic acid, may be recommended for maternal health [54].
CONCLUSION
Nutrition education in many methods has a power to improve knowledge, and dietary change of pregnant women. However, there is a need for future large high quality trials using a standardized approach to measuring and reporting similar findings across studies. A future study might use a double-blind RCT approach with larger sample size and a variety of nutritional outcomes. Longer duration in implementing the trials will improve the outcomes of the study as expected.
Limitation
Our study has several flaws, including a lack of access to the most often recommended databases for searching relevant literature and, ultimately, trial trials. Some research relied on self-reported outcome measures, which might be vulnerable to various biases (e.g., recall bias and response bias). Because some of the studies are of intermediate quality, their conclusions should be read with care. We should also consider that non-English paper were not considered and included in this review, with a potential bias to not identify as many eligible studies as possible.
Conflict of interest statement
The author(s) declares no conflict of interest.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Acknowledgements
We express our gratitude to the director of Jambi University for its support for the implementation of this research and President of Jambi University, Indonesia
REFERENCES
- Ho A, Flynn AC, Pasupathy D. Nutrition in pregnancy. Obstetrics, Gynaecology & Reproductive Medicine. 2016;26(9):259–64.
- Woldeamanuel GG, Geta TG, Mohammed TP, Shuba MB, Bafa TA. Effect of nutritional status of pregnant women on birth weight of newborns at Butajira Referral Hospital, Butajira, Ethiopia. SAGE open medicine. 2019;7:2050312119827096.
- Sokulmez P OA. Effects of General Health and Nutritional Status of Pregnant Adolescents on Newborn Health. Journal of Turkish Society of Obstetrics & Gynecology. 2014;11(1).
- Momin M, Jain V, Momin S, Kulkarni V. Nutritional Management for Pregnant Women-an extended role of Pharmacist. Journal of Pharmacy Research. 2012;5(12).
- Fleming TP, Watkins AJ, Velazquez MA, Mathers JC, Prentice AM, Stephenson J, et al. Origins of lifetime health around the time of conception: causes and consequences. The Lancet. 2018;391(10132):1842–52.
- Sebastiani G, Andreu-Fernández V, Herranz Barbero A, Aldecoa-Bilbao V, Miracle X, Meler Barrabes E, et al. Eating Disorders During Gestation: Implications for Mother’s Health, Fetal Outcomes, and Epigenetic Changes. Frontiers in pediatrics. 2020;8:587.
- Ronto R, Wu JHY, Singh GM. The global nutrition transition: trends, disease burdens and policy interventions. Public health nutrition. 2018;21(12):2267–70.
- Popkin BM. Global changes in diet and activity patterns as drivers of the nutrition transition. In: Emerging societies-coexistence of childhood malnutrition and obesity. Karger Publishers; 2009. p. 1–14.
- Smith LP, Ng SW, Popkin BM. Trends in US home food preparation and consumption: analysis of national nutrition surveys and time use studies from 1965–1966 to 2007–2008. Nutrition journal. 2013;12(1):1–10.
- Juul F, Hemmingsson E. Trends in consumption of ultra-processed foods and obesity in Sweden between 1960 and 2010. Public health nutrition. 2015;18(17):3096–107.
- Sweetman C, McGowan L, Croker H, Cooke L. Characteristics of family mealtimes affecting children’s vegetable consumption and liking. Journal of the American Dietetic Association. 2011;111(2):269–73.
- Wolfson JA, Bleich SN. Is cooking at home associated with better diet quality or weight-loss intention? Public health nutrition. 2015;18(8):1397–406.
- Lavelle F, Hollywood L, Caraher M, McGowan L, Spence M, Surgenor D, et al. Increasing intention to cook from basic ingredients: A randomised controlled study. Appetite. 2017;116:502–10.
- Herbert J, Flego A, Gibbs L, Waters E, Swinburn B, Reynolds J, et al. Wider impacts of a 10-week community cooking skills program-Jamie’s Ministry of Food, Australia. BMC public health. 2014;14(1):1–14.
- Berti C, Decsi T, Dykes F, Hermoso M, Koletzko B, Massari M, et al. Critical issues in setting micronutrient recommendations for pregnant women: an insight. Maternal & child nutrition. 2010;6:5–22.
- Jun S, Gahche JJ, Potischman N, Dwyer JT, Guenther PM, Sauder KA, et al. Dietary supplement use and its micronutrient contribution during pregnancy and lactation in the United States. Obstetrics and gynecology. 2020;135(3):623.
- Dubois L, Diasparra M, Bédard B, Colapinto CK, Fontaine-Bisson B, Morisset A-S, et al. Adequacy of nutritional intake from food and supplements in a cohort of pregnant women in Québec, Canada: the 3D Cohort Study (Design, Develop, Discover). The American journal of clinical nutrition. 2017;106(2):541–8.
- Pava-Cárdenas A, Vincha KRR, Vieira VL, Cervato-Mancuso AM. Promoting healthy eating in primary health care from the perspective of health professionals: a qualitative comparative study in the context of South America. BMC nutrition. 2018;4(1):1–11.
- Sharma P, Rani MU. Effect of digital nutrition education intervention on the nutritional knowledge levels of information technology professionals. Ecology of food and nutrition. 2016;55(5):442–55.
- Ota E, Hori H, Mori R, Tobe‐Gai R, Farrar D. Antenatal dietary education and supplementation to increase energy and protein intake. Cochrane Database of Systematic Reviews. 2015;(6).
- Hanson MA, Bardsley A, De‐Regil LM, Moore SE, Oken E, Poston L, et al. The International Federation of Gynecology and Obstetrics (FIGO) recommendations on adolescent, preconception, and maternal nutrition:“Think Nutrition First”#. International Journal of Gynecology & Obstetrics. 2015;131:S213–53.
- Lee A, Newton M, Radcliffe J, Belski R. Pregnancy nutrition knowledge and experiences of pregnant women and antenatal care clinicians: A mixed methods approach. Women and Birth. 2018;31(4):269–77.
- Marques AH, O’Connor TG, Roth C, Susser E, Bjørke-Monsen A-L. The influence of maternal prenatal and early childhood nutrition and maternal prenatal stress on offspring immune system development and neurodevelopmental disorders. Frontiers in neuroscience. 2013;7:120.
- Gernand AD, Schulze KJ, Stewart CP, West KP, Christian P. Micronutrient deficiencies in pregnancy worldwide: health effects and prevention. Nature Reviews Endocrinology. 2016;12(5):274–89.
- Borge TC, Aase H, Brantsæter AL, Biele G. The importance of maternal diet quality during pregnancy on cognitive and behavioural outcomes in children: a systematic review and meta-analysis. BMJ open. 2017;7(9):e016777.
- Fadare O, Amare M, Mavrotas G, Akerele D, Ogunniyi A. Mother’s nutrition-related knowledge and child nutrition outcomes: Empirical evidence from Nigeria. PloS one. 2019;14(2):e0212775.
- Lindqvist M, Lindkvist M, Eurenius E, Persson M, Ivarsson A, Mogren I. Leisure time physical activity among pregnant women and its associations with maternal characteristics and pregnancy outcomes. Sexual & Reproductive Healthcare. 2016;9:14–20.
- Aşcı Ö, Rathfisch G. Effect of lifestyle interventions of pregnant women on their dietary habits, lifestyle behaviors, and weight gain: a randomized controlled trial. Journal of Health, Population and Nutrition. 2016;35(1):1–9.
- Caut C, Leach M, Steel A. Dietary guideline adherence during preconception and pregnancy: A systematic review. Maternal & child nutrition. 2020;16(2):e12916.
- Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine. 2009;6(7):e1000097.
- Armijo‐Olivo S, Stiles CR, Hagen NA, Biondo PD, Cummings GG. Assessment of study quality for systematic reviews: a comparison of the Cochrane Collaboration Risk of Bias Tool and the Effective Public Health Practice Project Quality Assessment Tool: methodological research. Journal of evaluation in clinical practice. 2012;18(1):12–8.
- Campbell M. E McKenzie J. Sowden A, Katikireddi SV, E Brennan S, Ellis S, Hartmann-Boyce J, Ryan R, Shepperd S, Thomas J, et al Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline BMJ. 2020;368:l6890.
- Oliveira SC de, Fernandes AFC, Vasconcelos EMR de, Ximenes LB, Leal LP, Cavalcanti AMTS, et al. Effect of an educational intervention on pregnancy: a cluster-randomized clinical trial. Acta Paulista de Enfermagem. 2018;31:291–8.
- Demilew YM, Alene GD, Belachew T. Effect of guided counseling on dietary practices of pregnant women in west Gojjam zone, Ethiopia. Plos one. 2020;15(5):e0233429.
- Diddana TZ, Kelkay GN, Dola AN, Sadore AA. Effect of nutrition education based on health belief model on nutritional knowledge and dietary practice of pregnant women in Dessie Town, Northeast Ethiopia: A cluster randomized control trial. Journal of Nutrition and Metabolism. 2018;2018.
- AL-TELL MA, EL-GUINDI FK, SOLIMAN NM, EL-NANA H. Effect of nutritional interventions on anemic pregnant women’s health using health promotion model. The Medical Journal of Cairo University. 2010;78(2).
- Fallah F, Pourabbas A, Delpisheh A, Veisani Y, Shadnoush M. Effects of nutrition education on levels of nutritional awareness of pregnant women in Western Iran. International journal of endocrinology and metabolism. 2013;11(3):175.
- Goodarzi-Khoigani M, Moghadam MHB, Nadjarzadeh A, Mardanian F, Fallahzadeh H, Mazloomy-Mahmoodabad S. Impact of nutrition education in improving dietary pattern during pregnancy based on pender’s health promotion model: A randomized clinical trial. Iranian journal of nursing and midwifery research. 2018;23(1):18.
- DeStephano CC, Flynn PM, Brost BC. Somali prenatal education video use in a United States obstetric clinic: A formative evaluation of acceptability. Patient Education and Counseling. 2010;81(1):137–41.
- Shakeri M. The effect of educational program based on basnef model on the nutritional behavior of pregnant women. Int Res J Applied Basic Sci. 2013;5(12):1606–11.
- Baruth M, Schlaff RA, Deere S, Walker JL, Dressler BL, Wagner SF, et al. The feasibility and efficacy of a behavioral intervention to promote appropriate gestational weight gain. Maternal and child health journal. 2019;23(12):1604–12.
- Olson CM, Groth SW, Graham ML, Reschke JE, Strawderman MS, Fernandez ID. The effectiveness of an online intervention in preventing excessive gestational weight gain: the e-moms roc randomized controlled trial. BMC pregnancy and childbirth. 2018;18(1):1–11.
- Olson CM. Behavioral nutrition interventions using e-and m-health communication technologies: a narrative review. Annual review of nutrition. 2016;36:647–64.
- Nishimwe C, Mchunu GG, Mukamusoni D. Community‐based maternal and newborn interventions in Africa: Systematic review. Journal of Clinical Nursing. 2021;
- Konje ET, Magoma MTN, Hatfield J, Kuhn S, Sauve RS, Dewey DM. Missed opportunities in antenatal care for improving the health of pregnant women and newborns in Geita district, Northwest Tanzania. BMC pregnancy and childbirth. 2018;18(1):1–13.
- Teweldemedhin LG, Amanuel HG, Berhe SA, Gebreyohans G, Tsige Z, Habte E. Effect of nutrition education by health professionals on pregnancy-specific nutrition knowledge and healthy dietary practice among pregnant women in Asmara, Eritrea: a quasi-experimental study. BMJ Nutrition, Prevention & Health. 2021;bmjnph-2020.
- Zelalem A, Endeshaw M, Ayenew M, Shiferaw S, Yirgu R. Effect of nutrition education on pregnancy specific nutrition knowledge and healthy dietary practice among pregnant women in Addis Ababa. Clinics in Mother and Child Health. 2017;14(3):265.
- Goldstein RF, Abell SK, Ranasinha S, Misso M, Boyle JA, Black MH, et al. Association of gestational weight gain with maternal and infant outcomes: a systematic review and meta-analysis. Jama. 2017;317(21):2207–25.
- Boyle A, Timofeev J, Halscott T, Desale S, Driggers RW, Ramsey PS. Is 40 the new 30?: pregnancy outcomes by degree of weight gain among obesity subclasses. Obstetrics & Gynecology. 2014;123:41S.
- Berntorp K, Anderberg E, Claesson R, Ignell C, Källén K. The relative importance of maternal body mass index and glucose levels for prediction of large-for-gestational-age births. BMC pregnancy and childbirth. 2015;15(1):1–8.
- Wu Y, Wan S, Gu S, Mou Z, Dong L, Luo Z, et al. Gestational weight gain and adverse pregnancy outcomes: a prospective cohort study. BMJ open. 2020;10(9):e038187.
- Chen C-N, Chen H-S, Hsu H-C. Maternal prepregnancy body mass index, gestational weight gain, and risk of adverse perinatal outcomes in Taiwan: a population-based birth cohort study. International journal of environmental research and public health. 2020;17(4):1221.
- Gomes F, Bergeron G, Bourassa MW, Dallmann D, Golan J, Hurley KM, et al. Interventions to increase adherence to micronutrient supplementation during pregnancy: a protocol for a systematic review. Annals of the New York Academy of Sciences. 2020;1470(1):25.
- World Health Organization (WHO). Mainstreaming nutrition through the life-course. Essential Nutrition Actions. 2019.
![]() This work is licensed under a Creative Commons
This work is licensed under a Creative Commons
Attribution-NonCommercial-NoDerivatives 4.0 International License.
The influence of mobile app in Glycemic Control and Prevention of Hypoglycemics in Diabetic management: A Systematic Review
Netha Damayantie1* Muhammad Rusdi2, Syamsurizal2, Ummi Kalsum3
1 Student of Doctoral Programme faculty of Mathematic and and science, Jambi University
2 Chemical Education Study Program, Teacher Training and Education Faculty, Jambi University
3Public Health Study Program, Medicine and Health Sciences Faculty, Jambi University
* Corresponding author: Netha Damayantie, Jl. Jambi - Muara Bulian No.KM. 15, Mendalo Darat, Kec. Jambi Luar Kota, Kabupaten Muaro Jambi, 36129, Indonesia, Orcid : https://orcid.org/0000-0002-5628-2700. Email: netha.dam.57@gmail.com
Cita questo articolo
Abstract
Background. The use of technology in the treatment of diabetes can facilitate the medium of communication between nurses and clients in data collection to create a comfortable life for patients. The use of mobile health technology in diabetic education is an innovative learning method that can engage patients and influence positive health behaviors.
Aim. This study aims to find out the influence of mobile-based education applications in the Haemoglobin A1c control and prevention of hypoglycemia in patients with type 2 diabetes mellitus.
Methods. Database search for article are from four databases such as Pubmed, Sciencedirect, Proquest, and Cochrane is limited to the publication of the last ten years from 2010 to 2021 and full text article in English. Authors individually screened the titles and abstracts, then full articles in order to obtain papers that met inclusion criteria
Results. a total of 664 references were found. After duplicates were removed, 391 potentially relevant references remained from the database searches. Eight articles were finally designated as articles to be reviewed and use RCT design. Most studies put a Haemoglobin A1c (HbA1c) as a primary outcomes, and hypoglycemia as a secondary outcomes. Through the use of mobile app, there are reductions in HbA1c which affect the hypoglycemia events in Type 2 DM patients.
Conclusion. Mobile application can enhance HbA1c and hypoglycemia control among T2DM patients. Because providing patient education face to face is time-consuming, the use of mobile application may be an effective complement or alternative for healthcare professionals to manage the rapidly increasing number of diabetes patients.
Keywords: Mobile app, Type 2 DM, Glycemic control, Hypoglicemia prevention
Introduction
Diabetes mellitus, particularly type 2, is a global health issue in the worldwide. The International Diabetes Federation (IDF) estimated an escalation of diabetes prevalence from 424.9 million in 2017 to about 628.6 million by 2045 [1]. More than 10,3 million people had diabetes mellitus in Indonesia [2]. Ninety percent (90%) of diabetes cases is type 2 diabetes mellitus with characteristics of insulin sensitivity disorders and/or impaired insulin secretion [3]. The prevalence of diabetes mellitus in Indonesia based on doctor's diagnosis in the population aged ≥15 years has increased from 1.5% in 2013 to 2.0% in 2018 [4,5]. Administration of insulin therapy causes the main side effect of hypoglycemia. Another side effect is the immune response to insulin which can lead to insulin allergies or insulin resistance [3]. Hypoglycemia is a condition in which glucose levels in the blood decrease below the value of 70 mg / dl or less [6,7].The prevalence of hypoglycemia with type II diabetes mellitus patients can reach 70-80%, which has a serious impact on morbidity, mortality, and quality of life [8]. Severe occurrence of hypoglycemia in type 2 diabetes mellitus patients reaches 3-73 episodes per 100 patients annually [6]. A common phenomenon in the clinical practice is that many patients argue that mild hypoglycemia as a consequence of hypoglycemic control [9]. In addition, many patients misunderstand the symptoms of hypoglycemia as a symptom of ketoacidosis, because they need to reduce or delay insulin administration [10]. Patients attempted to lower blood sugar levels without knowing the effects of using the drug where patients may experience severe hypoglycemia as the result. One of the reasons for the lack of patient knowledge about hypoglycemia is the lack of information provided by healthcare professionals [11]. Shreds of evidence have shown that the potential use of smartphone-based technology has helped people with diabetes in self-care management by staying connected with health care providers. Futuristic features are provided with all the ease to understand and use [12,13]. A well-suited App could transform a mobile phone into a medical device helping ease the burden of diabetes, preventing complications, and improving a patient’s quality of life. However, an overwhelming number of products and services are available to patients with diabetes. Patients and providers must recognize the characteristics of these products and services to capitalize on the advantages while avoiding harmful deficiencies [14]. The use of technology in the treatment of diabetes can facilitate the medium of communication between nurses and clients in data collection to create a comfortable life for patients. An important goal of treatment with electronic media is to enable patients the opportunity to maintain effective they education without interruption [12]. Interest in mobile health apps in supporting self-management of health arises because it is easily accessible, portable, low cost, convenient for users, and has a widespread. Furthermore, 50% of smartphone users will have at least one mobile health app [13]. The use of mobile health technology in diabetic education is an innovative learning method that can engage patients and influence positive health behaviors [14].
This review aims to collate and provide evidence related to mobile application for Glycemic Control, and prevention of hypoglycemia of Diabetes Melitus patients.
Methods
Design
This study is a systematic review based on Preferred Reporting Items for Systematic Reviews and Meta-Analyzes (PRISMA). PRISMA is an evidence-based minimum set of items for reporting in systematic reviews and meta-analyses. PRISMA focuses on the reporting of reviews evaluating randomized trials, but can also be used as a basis for reporting systematic reviews of other types of research, particularly evaluations of interventions. Authors must use PRISMA as a guideline and theory underlying aims to help authors improve the reporting of systematic reviews and meta-analyses (PRISMA Statement, 2015).
Eligibility
Inclusion criteria for this systematic review are (1) adult-elderly patients (18-85 years), (2) uncomplicated or non co morbid diabetes mellitus patients, and (3) patients who are conscious and cooperative (4) study design that include in this review is randomized control trials (RCT). Exclusion criteria in this systematic review are (1) patients experiencing complications (stroke, heart, kidney), and (2) patients who have dementia and aphasia.
Search Methods
Database search for article are from four databases such as Pubmed, Sciencedirect, Proquest, and Cochrane is limited to the publication of the last ten years from 2010 to 2021 and full text article in English. Keywords used in the article search of all databases are combination of "diabetes mellitus" OR “Type 2 DM” AND "glycemic control” OR “Hypoglicemia prevention” OR “HbA1c” AND "health education" AND “m-health" OR “Mobile app”. The next step after the articles that meet the criteria are collected is to analyze and form the articles according to the specified inclusion and exclusion criteria. The article search process was carried out in August 2021. The article search uses keywords that have been determined by the researchers and limits the inclusion and exclusion criteria. The data obtained are then selected one by one by the researchers to determine the suitability of the articles desired by the researchers and delete the same articles or those that do not fit the criteria. After getting the articles according to the researchers, the articles are analyzed one by one and grouped to get the results. The next step is to discuss based on the points obtained from the selection results.
Critical appraisal
The included quantitative studies were appraised using the McMaster Critical Review Form for quantitative studies [18]. The critical appraisal process was undertaken independently by the two authors. Discrepancies in scoring were then resolved through discussions until consensus was achieved.
There are 13 question items that can be answered with yes, no, and not addressed options. Scores are given as a percentage, and one point for each question item if available. 90% were categorized as high quality, 70% medium, and low quality for the rest.
Data Abstraction
Two authors independently reviewed the abstracts of studies retrieved from the database Search and read the full-text of potentially relevant articles. For studies that met the inclusion criteria, data extraction was independently conducted by two investigators using our data extraction tool adapted from existing guidelines and other review articles of mobile application for DM [19,20]. Using this tool we extracted the general and mobile app features of the papers including the outcome, study design, characteristics of the intervention, evaluation method and main findings. Disagreements in data extraction were solved by a third investigator.
Data Analysis/ Synthesis
Data of the studies included were synthesized thematically in order to understand the effectiveness of mobile application. Thematic analysis involves discovering, interpreting and reporting patterns and clusters of meaning within the data. Using this frame-work and by reading the included articles several times, themes were identified. Subsequently, these themes were further examined for their similarities, differences and contradictions. The subject matter of the findings from the quantitative studies was examined, and the resulting information was placed under the qualitative themes. This integration of quantitative findings to the qualitative themes was completed by the first author. The second author reviewed the matched themes and quantitative studies. Any disagreement was resolved through mutual discussion. Due to the heterogeneity and insufficient number of the studies included, we could not conduct meta-analyses.
Results
Search Results
Combining the output of the searches in the various databases, a total of 664 references were found. After duplicates were removed, 391 potentially relevant references remained from the database searches. 283 articles removed by reasons of irrelevant, review/report, not full text, book chapter. Eight articles were finally designated as articles to be reviewed. PRISMA flowchart for Study selection can be presented in Figure 1.

Figure 1. PRISMA flowchart for Study selection
The main focus of this systematic literature review is the effects of mobile app on hypoglycemia prevention. However, to optimize the interpretation of these effects, we will first clarify the methodological quality and characteristics of the studies, as well as the characteristics of the mobile app under review. The authors developed tables for data analysis with the type of diabetes addressed in the review article, the types of technology used for the intervention along with outcomes measured. The most common health outcome measure was hemoglobin A1c (A1c), and hypoglycemia may present in secondary outcome. This shared data element allowed comparison between the varying interventions addressed in these reviews.
In Table 1 we reported the articles included in our study.






Table 1. Data extraction of studies included
The result of Critical review
The results of the critical appraisal of the studies are presented in Table 2, respectively. The data that contributed to the generation of these themes are presented narratively in the following results subsection, with the appropriate source references identified.

Table 2. Critical review for Quantitative studies included
Critical appraisal of quantitative research studies: As outlined in Table 2, all of the studies had a clear purpose and relevant literature reviews. All of the studies reported appropriate conclusions, given their study purpose.
Table 2 shows the value of Cohen's kappa coefficient in each article with a range of 0.41 to 0.806 with a moderate to strong category. This coefficient is the result of two reviewers who evaluate each article separately.
Study Characteristics
Most of the selected reviews used research from locations around the globe. Articles that meet the inclusion criteria come from several countries including China [21–23], USA [24,25], Norway [26], Japan [27], and France [28]. The mean age range reported was from 38 to 68 years old. Duration of the intervention was 3 months [27], 6 months [21,22,26], 9 months [23], and 12 months [24,25,28]. The number of participants involved in the study was in the range of 54 to 665 patients divided into intervention and control groups.
Outcomes Measured, Primary Focus
Primary outcomes
Change in HbA1c level after 1 year was chosen as the primary outcome because it is the main target measure when treating diabetes and is frequently used when evaluating interventions. HbA1c data were collected through the GPs and were assessed primarily with the Siemens DCA Vantage Analyzer a maximum of 2 weeks before or after the follow-up to reduce measurement bias [26].
In the study of Waki and colleague, HbA1c as a primary outcome was measured from baseline to 3-month follow-up for each patient with an intention-to-treat analysis in intervention and control groups [27].
The primary outcome of Quinn [25] study was change in glycated hemoglobin comparing control usual care (UC) and maximal treatment (Coach primary care providers portal with decision support (CPDS) at baseline versus 12 months. Medical chart reviews were used to ascertain patient data. For patients without a glycated hemoglobin within 4 months of the desired measurement, a glycated hemoglobin test was offered at no charge at baseline to determine eligibility and at 12 months. At baseline, glycated hemoglobin was measured using one device, the Bayer DCA 2000, by trained staff blinded to patient group assignment. At follow-up, if glycated hemoglobin was not ascertained within 14 days of the 12-month time point, reminders were provided to patients and physicians to complete the test. Glycated hemoglobin level at intermediate time points (3, 6, and 9 months) was collected from patients’ medical charts [24,25].
Franc et al. determined the primary outcomes of their study was the mean change in HbA1c from baseline to 12 months (primary endpoint), and the occurrence of hypoglycemia. An independent ‘‘Hypoglycemia Adjudication Committee’’ validated the classification of all declared hypoglycaemic episodes. A severe hypoglycemic episode means that the patient required the indispensable assistance of a third person. A symptomatic hypoglycemic episode refers to those symptoms of hypoglycemia associated with rapid recovery after self-administration of sugar [28].
The primary outcome in Xu et al study [22] was diabetic symptom scores. It was assessed by the diabetes symptom grading and quantitative scale according to the Guidelines for the Clinical Research of Chinese Medicine New Drugs. Secondary outcome was blood glucose level including fasting blood glucose, 2-h postprandial blood glucose (2 hPG), and glycated hemoglobin (HbA1c) at baseline and 6 months after intervention. Serum HbA1c level reflects a patient’s blood glucose concentration during the previous 2–3 months, so it was taken into consideration as an essential indicator [22].
The primary outcome in Zhang et al. study [29] was glucose control, including the changes (from baseline to months 3 and 6) in the HbA1c level. The major adverse event was hypoglycemia. Hypoglycemia was defined as BG ≤3.9 mmol/L [21].
In the Sun study, there were intervention and control groups. Primary outcome was self-administered blood glucose level. HbA1c level was measured at 3 and 6 months [23].
The primary outcome of Quinn study [24] was the change in HbA1c (% of total hemoglobin) in the control group versus in the intervention group, at baseline versus at 12 months. HbA1c levels were recorded at baseline and at 3, 6, 9, and 12 months. Patient data were retrieved from medical charts [24].
Intervention Features
We will describe a mobile application intervention based on each of the studies that we included in this review. Holmen et al., [26]: To increase self-management comprised of 3 intervention groups: the Few Touch Application (FTA) intervention group, the FTA with health counseling (FTA-HC) intervention group, and the control group. The FTA-HC group received health counseling for the first 4 months of the project period. The health counseling was based on the transtheoretical model of stages of change and a problem-solving model, and used motivational interviewing as a counseling technique. The health counseling in the present study was part of the mHealth intervention.
Waki et al., [27]. DialBetics is composed of 4 modules. First is the data transmission module: patients’ data—blood glucose, blood pressure, body weight, and pedometer counts. Second is the evaluation module: data are automatically evaluated following the Japan Diabetes Society (JDS) guideline’s targeted values. Third is the communication module: about meals, and advice on lifestyle modification. Fourth is dietary evaluation: patients’ photos of meals are sent to the server.
Quinn et al., [25]. The mobile software allowed patients to enter diabetes self-care data (blood glucose values, carbohydrate intake, medications, other diabetes management information) on a mobile phone and receive automated, real-time educational, behavioral, and motivational messaging specific to the entered data. The patient web portal augmented the mobile software application and consisted of a secure messaging center (for patient-provider communication), personal health record with additional diabetes information (e.g., laboratory values, eye examinations, foot screenings), learning library, and logbook to review historical data.
Franc et al., [28]. A reference nurse initiates the patient to the use of the DIABEO app on his smartphone. The patient enters relevant data (glycemia, physical activity, and ingested carbohydrates) and DIABEO calculates the insulin dose (an eventual dose adaptations). These data are sent every 2 h to a platform that is continuously visible by the reference nurse and the investigator.
Xu et al., [22]. The smartphone app for diabetes management was composed of 4 modules: syndrome differentiation, body differentiation and health preservation, thesaurus, and interactive follow-up. A reminder message would be received if the patients forget to complete that in time. The diabetes educators can track the data from the app and provide specific guidance and suggestions for the clients.
Zhang et al., [21]. Welltang app mainly comprises 4 parts: education, self-management (including records of SMBG, diet, exercise, medication, body weight, and other diabetes data), patient community, and communication between patients and clinicians. For clinicians, Welltang mainly provided the real-time uploading of data from patients.
Quinn et al., [24]. Mobile diabetes management software application (MDMA) allowed patients to enter diabetes self-care data (blood glucose values, carbohydrate intake, medications, and other diabetes management information) on a mobile phone and receive automated, real-time messages that were educational, behavioral, motivational, and specific to the entered data.
Sun et al., [23]. Patients uploaded the glucometer data to the mHealth management app which was then automatically transmitted to the medical server (glucometer was connected to the mobile phone via Bluetooth). The medical teams sent medical advice and reminders to patients to monitor their glucose levels via the personal messaging app or telephonically every 2 weeks.
Discussion
This systematic review provides an overview of studies on mobile applications in improving HbA1c and hypoglycemic control among T2DM patients. The highest decrease in HbA1c was 1.9% which is relatively high compared to several previous studies, which found a decrease in HbA1c of 0.49% [30] and 0.51% [31]. There was no subgroup analysis in studies involving patients in different age groups. In general, it can be concluded that mobile application interventions can provide the same benefits for younger (<55 years) or older (≥55 years) T2DM patients. It is inconsistent with findings from a previous systematic review [30], which suggested that ST interventions were more effective for younger T2DM patients than older patients. The mobile applications in the included studies are complex and generally include more than one component. Almost all studies evaluate mobile applications related to lifestyle modification and self-monitoring of blood glucose. Therefore, it is logical to conclude that a decrease in HbA1c is associated with improving the patient's lifestyle. Although quality improvement programs are usually multi-component, they are more oriented towards targeting changes in health care provider behavior or service delivery models [32]. Interventions using mobile applications have a stronger focus on empowering patient behavior change. A systematic review Barreira et al., [33] showed that exercise effectively reduced HbA1c. Of the four included studies, which have included a component of exercise adherence monitoring [23,26,27], this suggests that a mobile application may be an effective adjunct to controlling HbA1c, or It is more common to enhance lifestyle modification efforts among type 2 DM patients. These studies also suggest considering the mobile application as a complementary intervention that can be used in diabetes self-care strategies more effectively through lifestyle modification and self-monitoring blood glucose. In the included studies, self-monitoring of blood glucose was also included as part of a mobile application intervention, while its effectiveness in controlling DM was uncertain.
A previous systematic review study Xu et al., [34] concluded that SMBG only contributed to a 0.46% decrease in HbA1c. Available evidence suggests that SMBG can promote self-management, increase medication adherence rates, and improve the patient's ability to detect hypoglycemia [35]. However, the UK National Institute for Health and Care Excellence guidelines state that SMBG is not recommended as part of routine DM management but should be considered in subgroups of patients, such as those receiving insulin therapy and patients prone to hypoglycemia [36]. Current clinical practice guidelines recommend close monitoring of HbA1c and titration of drug therapy instead [37]. It was difficult for us to find relevant literature on mobile applications to reduce the risk of hypoglycemia in both type 1 and type 2 DM patients. Several studies that we included in this review made hypoglycemia a secondary outcome. The results obtained from the two studies stated that there was no significant difference between the intervention group and the control group. Reports of signs and symptoms of hypoglycemia occurred only once or twice in 1 year of follow-up [25,28]. However, post hoc analyses of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial indicated an increased hypoglycemia risk in type 2 diabetic participants with poorer glycemic control than subjects with more desirable HbA1c levels, irrespective of assigned treatment group [38]. Based on this statement, it can be concluded that from all studies included in this review, the mobile application can provide an effect on controlling hypoglycemia levels in Type 2 DM patients, although it is not clearly stated how the mechanism is. Little is known about the relationship between glycemic control and hypoglycemia in the usual care setting, where clinical decision-making about treatment intensity occurs and is modified throughout a patient's life [39].
Based on the two studies included in this review, it appears that there is no significant effect of the use of mobile phone applications on the quality of life of people with diabetes. The possible cause of no significant change in the quality of life before and after using the application is the age of the participants, most of which are in the elderly who feel less interested in using technology, especially smartphone-based [26]. The elderly need more intensive guidance regarding the use of technology applications, usually the elderly ask to be accompanied by family members or people who care for them. For the elderly who feel the exhaustion of their illness, they often hand over the responsibility to the people who take care of them [40,41].
Conclusion
In conclusion, mobile application can enhance HbA1c and hypoglycemia among T2DM patients. Because providing patient education face to face is time-consuming, the use of mobile application may be an effective complement or alternative for healthcare professionals to manage the rapidly increasing number of diabetes patients. Because providing patient education face to face is time-consuming, the use of mobile application as an educational media may be an effective complement or alternative for healthcare professionals to manage the rapidly increasing number of diabetes patients. The evidence suggests that organizations, diabetes educators, policy makers, and payers should consider these solutions in the design of diabetes self-management education and support services for population health and value-based care models. With the widespread adoption of mobile phones, digital health solutions that incorporate evidence-based, behaviorally designed interventions can improve the reach of and access to diabetes self-management education and ongoing support.
Limitation
We have identified several limitations in this study, including limited access to several good-quality databases, which are expected to provide broader search results. In addition, studies that matched our inclusion criteria were also very limited with regard to hypoglycemic control. We also considered potential bias related to different intervention/app, duration of intervention, and the limited numbers of RCTs included. Also, in the search strategy, some important databases are missing.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Competing interests statement
There are no competing interests for this study.
REFERENCES
- J.E. Shaw , R.A. Sicree PZZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Australia; 2010.
- Kementrian Kesehatan RI. Suara Dunia Perangi Diabetes. Jakarta; 2018.
- Decroli E. Diabetes Mellitus Tipe 2. I. Kam, Alaxander; Efendi Y, editor. Padang; 2019.
- Kementrian Kesehatan RI. Laporan Nasional hasil Riskesdas 2013. Jakarta: Badan Penelitian dan Pengembangan kesehatan; 2013.
- Kementerian Kesehatan RI. Laporan Nasional Riskesdas 2018. Jakarta: Badan Penelitian dan Pengembangan kesehatan; 2019.
- ADA. Standars Of Medical Care In Diabetes — 2017 Standards of Medical Care in Diabetes d 2017. The Journal of Clinical and Applied Research and Education. 2017;40(January):S48–56.
- Soelistijo SA, Novida H, Rudijanto A, Soewondo P, Suastika K, Manaf A, et al. Konsensus Pengelolaan Dan Pencegahan Diabetes Melitus Tipe 2 Di Indonesia 2015. Edisi I. Buku Konsensus DM Tipe-2. Jakarta: PB Perkeni; 2015. 11–14 p.
- Setyohadi B. Kegawatdaruratan Penyakit Dalam. Jakarta: Pusat Penerbitan Ilmu Penyakit Dalam; 2011.
- Sudoyo, A.W; Alwi, SB; Marcellus,S S. buku Ajar Ilmu Penyakit Dalam. 1st ed. Jakarta: EGC; 2007.
- Hudak, Carolyn. M; Gallo B. Keperawatan kritis Pendekatan Holistik. 8th ed. Jakarta: EGC; 2012.
- Sutawardana JH. Phenomenology Study The Experience Of Persons With Diabetes Mellitus. Nurseline Journal. 2016;1(1):159–75.
- Arnhold M, Quade M, Kirch W. Mobile applications for diabetics: a systematic review and expert-based usability evaluation considering the special requirements of diabetes patients age 50 years or older. Journal of medical Internet research. 2014;16(4):e2968.
- Brzan PP, Rotman E, Pajnkihar M, Klanjsek P. Mobile applications for control and self management of diabetes: a systematic review. Journal of medical systems. 2016;40(9):1–10.
- Rose KJ, Petrut C, L’Heveder R, de Sabata S. IDF Europe’s position on mobile applications in diabetes. Diabetes research and clinical practice. 2019;149:39–46.
- Tavsanli NG, Karadacovan A, Saygili F. The use of videophone technology (telenursing) in the glycaemic control of diabetic patients: a randomized controlled trial. Journal of Diabetes Research and Clinical Metabolism. 2013;2(1):1.
- Miller AS, Cafazzo JA, Seto E, Seto E. A Game Plan: Gamification Design Principles in mHealth Applications for Chronic. Health Informatics Journal. 2014;1–10.
- Kho SES, Lim SG, Hoi WH, Ng PL, Tan L, Kowitlawakul Y. The development of a diabetes application for patients with poorly controlled type 2 diabetes mellitus. CIN - Computers Informatics Nursing. 2019;37(2):99–106.
- Law M, Stewart D, Pollock N, Letts L, Bosch J, Westmorland M. Critical review form–quantitative studies. McMaster University: Occupational Therapy Evidence-Based Practice Research Group. 1998;
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of clinical epidemiology. 2009;62(10):e1–34.
- Sun C, Malcolm JC, Wong B, Shorr R, Doyle M-A. Improving glycemic control in adults and children with type 1 diabetes with the use of smartphone-based mobile applications: a systematic review. Canadian journal of diabetes. 2019;43(1):51–8.
- Zhang L, He X, Shen Y, Yu H, Pan J, Zhu W, et al. Effectiveness of Smartphone App–Based Interactive Management on Glycemic Control in Chinese Patients With Poorly Controlled Diabetes: Randomized Controlled Trial. Journal of medical Internet research. 2019;21(12):e15401.
- Huiwen XU, Yuan Y, Li Y, En TAKASHI AK. Effect of a traditional Chinese medicine theory-based mobile app on improving symptoms in patients with type 2 diabetes mellitus: A randomized controlled trial. Journal of Integrative Nursing. 2021;3(3):97–105.
- Sun C, Sun L, Xi S, Zhang H, Wang H, Feng Y, et al. Mobile phone–based telemedicine practice in older chinese patients with type 2 diabetes mellitus: randomized controlled trial. JMIR mHealth and uHealth. 2019;7(1):e10664.
- Quinn CC, Shardell MD, Terrin ML, Barr EA, Park D, Shaikh F, et al. Mobile diabetes intervention for glycemic control in 45-to 64-year-old persons with type 2 diabetes. Journal of Applied Gerontology. 2016;35(2):227–43.
- Quinn CC, Shardell MD, Terrin ML, Barr EA, Ballew SH, Gruber-Baldini AL. Cluster-randomized trial of a mobile phone personalized behavioral intervention for blood glucose control. Diabetes care. 2011;34(9):1934–42.
- Holmen H, Torbjørnsen A, Wahl AK, Jenum AK, Småstuen MC, Årsand E, et al. A mobile health intervention for self-management and lifestyle change for persons with type 2 diabetes, part 2: one-year results from the Norwegian randomized controlled trial RENEWING HEALTH. JMIR mHealth and uHealth. 2014;2(4):e3882.
- Waki K, Fujita H, Uchimura Y, Omae K, Aramaki E, Kato S, et al. DialBetics: a novel smartphone-based self-management support system for type 2 diabetes patients. Journal of diabetes science and technology. 2014;8(2):209–15.
- Franc S, Hanaire H, Benhamou P-Y, Schaepelynck P, Catargi B, Farret A, et al. DIABEO system combining a mobile APP software with and without Telemonitoring versus standard care: a randomized controlled trial in diabetes patients poorly controlled with a Basal-Bolus insulin regimen. Diabetes Technology & Therapeutics. 2020;22(12):904–11.
- Li X, Yu S, Zhang Z, Radican L, Cummins J, Engel SS, et al. Predictive modeling of hypoglycemia for clinical decision support in evaluating outpatients with diabetes mellitus. Current Medical Research and Opinion. 2019;35(11):1885–91.
- Hou C, Carter B, Hewitt J, Francisa T, Mayor S. Do mobile phone applications improve glycemic control (HbA1c) in the self-management of diabetes? A systematic review, meta-analysis, and GRADE of 14 randomized trials. Diabetes care. 2016;39(11):2089–95.
- Wu IXY, Kee JCY, Threapleton DE, Ma RCW, Lam VCK, Lee EKP, et al. Effectiveness of smartphone technologies on glycaemic control in patients with type 2 diabetes: systematic review with meta‐analysis of 17 trials. Obesity Reviews. 2018;19(6):825–38.
- Tricco AC, Ivers NM, Grimshaw JM, Moher D, Turner L, Galipeau J, et al. Effectiveness of quality improvement strategies on the management of diabetes: a systematic review and meta-analysis. The Lancet. 2012;379(9833):2252–61.
- Barreira E, Novo A, Vaz JA, Pereira AMG. Dietary program and physical activity impact on biochemical markers in patients with type 2 diabetes: A systematic review. Atencion primaria. 2018;50(10):590–610.
- Xu Y, Tan DHY, Lee JY. Evaluating the impact of self‐monitoring of blood glucose frequencies on glucose control in patients with type 2 diabetes who do not use insulin: a systematic review and meta‐analysis. International journal of clinical practice. 2019;73(7):e13357.
- Berard LD, Blumer I, Houlden R, Miller D, Woo V. Monitoring glycemic control. Canadian journal of diabetes. 2013;37:S35–9.
- Chung WK, Erion K, Florez JC, Hattersley AT, Hivert M-F, Lee CG, et al. Precision medicine in diabetes: a consensus report from the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes care. 2020;43(7):1617–35.
- Nolan K, Shearn P, Gholitabar M, Richardson J. NICE Update NICE public health guidance update.
- Lipska KJ, Warton EM, Huang ES, Moffet HH, Inzucchi SE, Krumholz HM, et al. HbA1c and risk of severe hypoglycemia in type 2 diabetes: the Diabetes and Aging Study. Diabetes care. 2013;36(11):3535–42.
- Hong S, Preswala L, Harris YT, Romao I, Ross DW, Paz HA, et al. Hypoglycemia in Patients with Type 2 Diabetes Mellitus and Chronic Kidney Disease. Kidney360. 2020;
- Androutsou T, Kouris I, Anastasiou A, Pavlopoulos S, Mostajeran F, Bamiou D-E, et al. A smartphone application designed to engage the elderly in home-based rehabilitation. Frontiers in Digital Health. 2020;2:15.
- Paiva JO V, Andrade RMC, de Oliveira PAM, Duarte P, Santos IS, Evangelista AL de P, et al. Mobile applications for elderly healthcare: A systematic mapping. PloS one. 2020;15(7):e0236091.
![]() This work is licensed under a Creative Commons
This work is licensed under a Creative Commons
Attribution-NonCommercial-NoDerivatives 4.0 International License.
Nurses' experiences and emotions in the face of changes caused by the COVID-19 pandemic: a phenomenological study
Sara Muzzicato1, Lorenza Garrino2, Vincenzo Alastra2, Valeria Miazzo1
- Opera San Camillo Foundation, Turin
- Master Executive Narrative Practices in Care Professions, COREP, Turin
*Corresponding author: Sara Muzzicato, Department of Rehabilitation, Recovery and Functional Rehabilitation Level 2, Fondazione Opera San Camillo, Turin. Email: sara.muzzicato@gmail.com
Cita questo articolo
ABSTRACT
Introduction: Following the Covid-19 pandemic, healthcare personnel had to face a very difficult period linked to the healthcare emergency, with important repercussions from a professional and personal point of view. These aspects have been explored by numerous researches on an international level, but only a small number of articles have investigated the phenomenon in the Italian context. The aim of this research is to describe the experience of healthcare workers in a Covid ward, exploring their emotional responses.
Materials and Methods: The study consists of a qualitative research with a phenomenological approach according to Giorgi. Narrative interviews were used with healthcare workers who worked in a Covid ward at the San Camillo health centre in Turin, a hospital specialising in second level functional recovery and re-education.
Results: Through the field research, 12 interviews were collected, involving 9 nurses and 3 social-health workers, working in a ward dedicated to the care of Covid-19 patients. The common themes that emerged concerned: the beginning of the Covid operator's "journey", characterised by a profound change in professional life since the beginning of the pandemic; the whirlwind of emotions and feelings experienced (fear, feeling blocked, annulled, powerless, depersonalised by suits and masks, anguish due to both physical and psychological isolation, etc.); relations with family members and friends; the relationship with the patient's family; relations with the operators' families; the risk of contagion and the fear of infecting oneself and one's loved ones; the group as a handhold for not giving up, as a point of strength, union and trust; the awareness of change with the desire to take one's own life back into one's own hands, taking advantage of the good things this time can give.
Conclusions: The research highlights the ability of the operators to identify positive aspects in the experiences lived, the union and trust in the group and the support of the family despite the strong fear of contagion. There are also important suggestions to reinforce strategies for dealing with such health emergencies and the importance for each individual in feeling accompanied throughout the process, in the difficult challenges they face.
Keywords: Covid-19, Experiences, Nursing, Narrative, Phenomenological approach.
INTRODUCTION
On 31 December 2019, Chinese Health Authorities reported to the World Health Organisation a cluster of cases of pneumonia of unknown aetiology in the city of Wuhan, in China's Hubei province. On 9 January 2020, the Centre for Disease Control and Prevention of China reported that a new coronavirus (SARS-CoV-2)[1] was identified as the causative agent of the respiratory disease later named Covid-19. China made public the genome sequence that enabled a diagnostic test and on 30 January 2020, the World Health Organisation (WHO)[2] declared the Coronavirus outbreak in China to be an "International Public Health Emergency" [3,4]. From then on, the word 'COVID-19' has indicated the disease associated with the SARS-CoV-2 virus (severe acute respiratory syndrome coronavirus 2), characterised by mild symptoms (fever, sore throat, fatigue, muscle pain, loss of taste and smell) or more severe symptoms (pneumonia, respiratory failure)[5]. Such symptoms have often led to the need for intensive care[6,7], thus causing high pressure on hospitals struggling to cope with too many patients to care for [8]. In this catastrophic scenario linked to the epidemic, Italy was one of the countries most affected[9]. Between the beginning of February and 30 November 2020, 1,651,229 positive Covid-19 cases were diagnosed by Regional Reference Laboratories and reported to the Italian National Institute of Health (NIH) - Italian National Integrated Surveillance System by 20 December 2020[10].
The pandemic has had different intensities and lethality in Italy compared to the rest of Europe. Differences in lethality rates are explained by: demographics, as mortality tends to be higher in older populations with co-morbidities; characteristics of the healthcare system, where there are organisational shortcomings, initial delays in understanding the severity of the emergency, deficits in infection tracking systems, hospitals overwhelmed by admissions, etc.; differences in the number of people tested; and different levels of virus aggressiveness[11].
Italy faced an unprecedented health crisis, with serious shortages of health professionals and difficulties in procuring personal protective equipment. New organisational models had to be implemented and hospital inpatient facilities had to be rapidly transformed into units suitable for the care of pandemic patients[12].
The NIH weekly bulletin of 28 April 2020 stated that 47.4% of the cases of infection among healthcare personnel were nurses[13].
In Italy[14] according to the provincial records, 40 nurses died, 32 of whom with the Covid-19 disease (positive swab), 4 with Covid-related illness (for whom the viral pathology was a favourable factor) and 4 (positive in any manner) for whom the mode of death was suicide[15]. A different view of the same phenomenon is reported by the monitoring as of 15 June 2020 conducted by INAIL (Italian National Institute for Insurance against Accidents at Work). INAIL, considering the accident reports referring only to insured workers, certified that there were a total of 236 deaths from Covid-19, of which 40% were healthcare professionals and 61% were nurses. In this complex epidemiological and healthcare framework, healthcare personnel reported the consequences of significant psychophysical stress with experiences and emotions still largely to be explored. Arasli et al. (2020)[16] explored experiences during the Covid-19 pandemic through testimonies written by nurses on social media through qualitative research. The study showed a high level of stress among healthcare professionals related to the risk and fear of becoming infected. Labrague et al. (2020)[17], through a quantitative study conducted in a region of the Philippines, highlighted high dysfunctional levels of anxiety in frontline nurses, while recording an increase in their resilience. On the Italian scene, Catania et al. (2020)[18] carried out qualitative research involving nurses from all regions of the peninsula. This study highlighted the enormous impact of COVID-19 on nurses, the need to identify new working practices, and highlighted the high-risk nature of nursing, exacerbated by the difficulty in Personal Protective Equipment (PPE) availability. In addition to reporting the high levels of stress experienced by the interviewees, the element of narratives also highlighted the resilience of the nursing community. Qualitative research was conducted by De Vito et al.[19], through the narratives of paediatric doctors and nurses in the paediatric emergency room of the Regina Margherita hospital. The authors emphasise how much the number of admissions in the paediatric sector had fallen, reflecting profoundly on changes in care, but also on the relationship itself with and between patients.
The results of the study show how the act of describing helped participants to process and understand their experience. Storytelling provided a cathartic means for participants to reformulate the events they experienced, rationalising them and making sense of them. In the Turin landscape, the experiences of nursing students were investigated. Garrino et al. (2021)[20], through a qualitative study, emphasised the changes induced by Covid-19 in nursing education. The need to use distance learning and the impossibility of doing internships during the pandemic period created many difficulties in training students. The narrative approach[21] and reflective thinking[22] aim to capture the latent aspects and hidden meanings of the complex pandemic reality[23,24].
The aim of the research is to describe the experience of health workers on a Covid ward, exploring their experiences and emotions.
MATERIALS AND METHODS
Study design
In this study, a qualitative methodology was used to investigate subjective phenomena, based on the assumption that fundamental truths about reality are rooted in people's lived experiences. This method allows for exploration of experiences by the person who has them, attempting to describe the meanings that the individual creates and gives to that experience, understanding the structure, nature and form, as perceived by the individual[25]. This survey aims to understand the experience of nurses and social workers during the first wave in a ward caring for Covid-19 patients, and who are now called upon again to provide the same type of care, in order to find out how the workers in question have responded to a pandemic emergency which, in addition to involving the work aspect, has invaded the personal sphere.
Background
The San Camillo hospital, as a hospital specialising in second-level functional recovery and rehabilitation, provides intensive rehabilitation treatment in the post-acute phase of the illness. The hospital has five departments that fulfil this function.
In November 2020, during the second wave of the pandemic, two wards were dedicated to the care of Covid patients. The health workers of these two wards, defined as 'COVID staff', had to cope with this new situation with various difficulties that have also characterised many healthcare facilities in Italy, but in this second phase they were able to use sufficient and appropriate PPE. The COVID wards of the facility were designed for a maximum capacity of 20 beds and intended for the care of patients coming from the intensive care units of other hospitals and in the sub-acute phase. Other patients in the early stages of the disease came directly from the emergency rooms of local hospitals, which could not cope with all the demand at that time. During admission, the intention was to stabilise the clinical condition and ventilatory support consisted of a Venturi mask or nasal cannulae, not having the tools provided in intensive care, such as assisted ventilation or intubation of the patient. The hospitalisation continued until the swab was negative, although the symptoms had already receded. Few of these patients died in the facility. The research was conducted in only one of the two Covid departments (with the participation of three respondents who worked in the second department, but who had worked sporadic shifts in the Covid department under consideration).
Participants
In this study, nurses and social workers (OSS) working in the Covid ward of the San Camillo hospital in Turin agreed to participate. Participants include the researcher (MS), in the role of observer-participant.
Mode of data collection
The study was based on a collection of semi-structured interviews consisting of 11 open-ended questions (Box 1) and proposed directly to the persons involved by email[26,27]. Respondents participated on a voluntary basis. Non-probabilistic, purposive sampling continued until data saturation, collected between 15 December 2020 and 15 January 2021. The questions for the semi-structured interviews were elaborated with the narrative interview method[28] and were chosen through the "SIFA" method, in order to try to explore each sphere of interest regarding Feelings, Ideas, Functions/Activities of the client, Expectations[29].
Methods of data analysis
For data analysis, the phenomenological method according to Giorgi (2008)[30] was used (Box 2). The interviews were read over and over again, seeking personal assessments through a suspension of judgement. Subsequently, an attempt was made to find common areas of meaning describing the most important themes reported by the interviewees[31,32]. The analysis was conducted independently by researchers S.M., L.G., V.A. and V.M. They then compared their work using the triangulation method[33]. During the analysis, the researchers reflected on their own values and suspended judgements, knowledge and ideas about the phenomenon under study[34].
Ethical consideration
The persons involved voluntarily agreed to answer the interview and signed an informed consent on the use and processing of the data. The research was authorised by the Health Directorate and the General Directorate of the San Camillo Hospital.
RESULTS
Through field research, 12 interviews were collected. Table 1 shows the socio-demographic data of the participants.
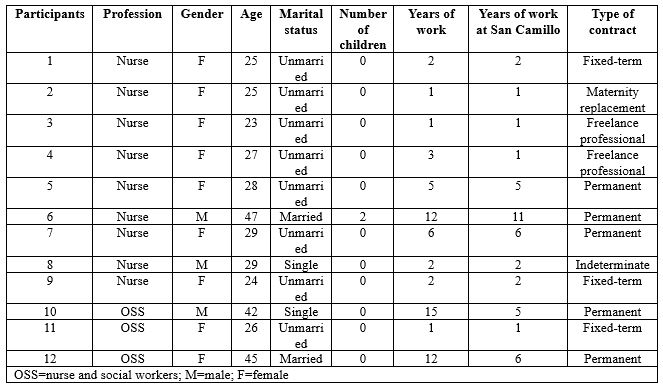
Table 1 - Social and personal data of participants
The average age of those involved is 30, with a minimum age of 23 and a maximum age of 47. All operators were professionally trained in Italy. None have postgraduate or Master's degrees. Several main and recurring themes emerged from the analysis of the interviews. These macro-categories bring us back to the experience of the participants. Terminology as presented and written by the interviewees themselves is reported, outlining the importance of the meanings expressed by them. The following themes emerged: the beginning of the Covid worker's 'journey' and the whirlwind of emotions and feelings that accompanied that (fear, feeling stuck, helpless, powerless, concerns for one's family in relation to the risk of contagion and the fear of infecting oneself and loved ones), the group as a foothold to keep going, a point of strength, union and provider of trust, the awareness of change, the cognition of time and the constructive vision of the experience (table 2).
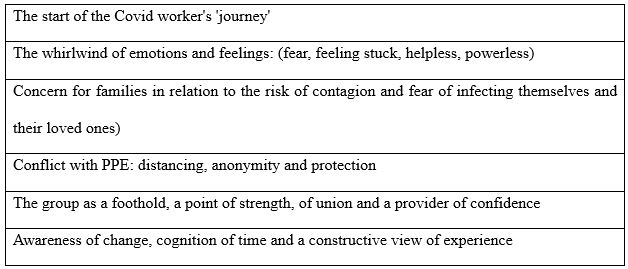
Table 2 – Main themes emerging from the analysis
The start of the Covid worker's 'journey'
The interviews reveal the profound change that occurred in the participants' professional lives at the beginning of the pandemic. Most of them talk about the impossibility of choosing whether to work in a Covid department or not, often indicating it as a decision linked to a sense of duty fulfilment.
[...] "It wasn't really a personal choice to join the Covid team... I happened to be there, and I was probably OK with that." [...] (interview 1)
[...] "I didn't really have a choice in deciding whether I could work closely with Covid-positive patients... So compared to my start in a Covid department, I can't even explain how it came about." [...] (interview 3)
Participants underline the initial impact they had following the news, accompanied by a set of feelings that were difficult to deal with at the time and to talk about later. They describe thoughts, emotions and sensations and there are often conflicting feelings, accompanied by fear, anxiety and stress.
[...] "Literally thrown into the deep end... My thoughts were questions. Why? Why? Why? So many questions that had no answers." [...] (interview 8)
[...] "I'm still trying to figure it out... on the front line in a Covid ward... I wasn't chosen, I found myself there almost by accident." [...] (interview 7)
In the interviews, the theme of travel emerges significantly, as a symbol of uncertainty and restlessness in trying to know and explore unknown places; as well as the theme of battle, almost as if they had to fulfil a destiny already written in their professional profile.
[...] "I didn't feel chosen, I felt enlisted in an impromptu army for an impromptu battle... I was there, so I had to fight... I had the fear and adrenaline of those who leave without knowing the destination and the consequences of their journey." [...] (interview 4)
A whirlwind of emotions and feelings: fear, feeling stuck, helpless, powerless
Concerning the emotions felt during this long experience by the health workers, many of them found themselves facing different difficulties, multiple fears and feelings, one of the main ones being isolation, not only physical but also psychological.
[...] "I avoided even the contact allowed by the Decrees, I isolated myself completely, more than was necessary... All you can do is wake up in the morning and wonder when it will end... I would have liked to live fully, not at the mercy of anxiety and worry. [...] (interview 1)
[...] "I would arrive home drained, feeling nothing but tiredness that muffled all the outside world." [...] (interview 2)
[...] "I see myself as someone who put aside feelings and sensations to face a big battle, so today I don't even remember what I was feeling... We have lost all consciousness, we no longer saw well, we no longer heard well, we no longer spoke much..." [...] (interview 3)
Respondents write that they feel alone in this battle, misunderstood, stuck and aimless, depersonalised, helpless due to the suits and masks, powerless before an invisible enemy so difficult to defeat.
[...] "When I finish a shift, I feel like I have finished a test under stress... as though I had passed a test... many times I felt like I hadn't made it, as though the ground was sinking from under my feet, other times I felt empty, as though under that suit there was almost nothing left... as if I had failed, as if I hadn't done enough." [...] (interview 4)
[...] "I remember the fear... and the tiredness because I had been alone in facing that new beginning so physically and psychologically intense... The whole condition of isolation puts a lot of pressure on you psychologically... I felt powerless, a nobody before something so big... I felt like a wrapper, a container whose contents had been disposed of along with the protective suit." [...] (interview 5)
The family and the risk of contagion: the fear of infecting oneself and one's loved ones
A topic that is repeated in almost every narrative is the importance of family affection. This theme is often addressed in the interviews, emphasising the importance that health workers attached to the support given by their loved ones, but at the same time linked to the constant fear of infecting themselves and consequently their families.
[...] "If I get infected will I be sick? And at home? If mum and dad get ill? Who will take care of Granny if we are sick? What if Granny gets sick?" [...] (interview 1)
[...] "I was afraid though, afraid of not being up to it and afraid of infecting myself and my loved ones." [...] (interview 2)
[...] "The biggest fear I had was that I would get worse and that I could infect my partner... that last idea drove me mad." [...] (interview 5)
There was a high level of stress among the interviewees, which, despite everything, also contributed to an increase in attention and precautions regarding safety regulations, the correct use of personal protective equipment and the correct way of disposing of it.
[...] "At the onset, I didn't have tumultuous emotions, it was the people next to me who were really very worried and I honestly experienced their emotion... The first thing I think about when I start my shift is that I must not get sick, so I must do everything I can to avoid infection." [...] (interview 3)
[...] "I try to be focused because you can let your guard down due to tiredness and then risk getting infected." [...] (interview 12)
Conflict with PPE: distancing, anonymity and protection
The interviews reveal the perceptions of nurses and social workers obliged to wear "all those layers of latex", exploring their experiences in relation to the care provided to their patients on the Covid ward. Nurses and social workers talk of overalls, double gloves, double masks, footwear, goggles and face shields which, while vital for working on Covid wards, have raised barriers between staff and patients.
[...] "A person covered from head to toe without knowing what he looks like or not remembering his name, as if he wasn't human... and all I know of this person are his brown eyes surrounded by a mask and a big suit." [...] (interview 1)
[...]“"Halfway between astronauts and aliens!" [...] (interview 2)
[...]“I never imagined that I would keep my physical and moral distance from a patient in such a way that I could become one of the many operators, just any operator, someone easily replaceable... I didn't use to feel naked unless wearing a gown, visor and mask, whereas now I do." [...] (interview 3)
[...]“"So many little white men, completely covered by overalls, gowns, masks, gloves and visor, almost clumsy in their movements and practically indistinguishable from each other... What I miss most is being able to show my smile to the patients, free from masks, and to shake their hands, free from those multiple layers of gloves." [...] (interview 5)
[...]“Living diving suits... it's as though there were a thousand barriers, a thousand layers separating us...a gentle caress with double latex gloves is not the same..."[...] (interview 6)
The group as a foothold for not giving up: strength, unity and trust
From the interviews, it emerges that the group has been a strong point, an important support for the health workers to go on and not give up.
[...] "I have never believed in the motto 'unity is strength' as I do now... in April there were so many brave little soldiers, in November we were one giant soldier...I don't feel alone, never; I feel escorted, I feel that someone is looking out for me as I am looking out for someone else... the working group has become a family... I would get through this as long as I had this team to rely on." [...] (interview 4)
[...] "I am grateful to her for that moment, for understanding me and giving me strength when she was probably also on her last legs. We hugged each other when we left the hospital, amidst tears. I don't think I could have done it without her that day." (Interview 6)
[...] "We have been able to overcome some difficult moments only thanks to our unity. (Interview 7)
According to the interviewees, coping with such a complex period with one's team helped to increase cohesion, strengthen group dynamics and was often the driving force needed to cope with stressful situations.
[...] "The wonderful team I have the honour of sharing this experience with has become very cohesive. We all worked together for the same goal on the same road, holding hands, hugging ideally, supporting each other, experiencing the same feelings, falling down and helping each other up." [...] (interview 3)
[...]“"I believe that the greatest strength came from the working group, which I have never before felt close to me, or rather part of me... in the group set up for the Covid emergency, I really found a rock to rely on. We work with common principles, side by side to achieve the same goals. What I perceive between us is harmony, respect and sharing"[...] (interview 5)
Awareness of change: time, self-work, constructive view of the experience
What emerges from the interviews is the strength and the desire to take charge of one's own life again, the desire to make it through this pandemic, trying to find a positive side, not to throw everything away, to seize what good can come from this experience. From the words of those interviewed, one can see a devastating past and present, which has affected people greatly, but also a future full of hope.
[...] "I hope to be myself with some more awareness, especially about what was taken for granted before Covid... I'm happy to still feel like myself, to not want to give in to the suffering that Covid forced us to face every day." [...] (interview 2)
[...]“"I worked on myself like we all did...The nurse I loved to be is here somewhere, she is not gone... My job will go back to that wonderful normality I loved, with some more experience, some scars that won't go away, some indelible memories..."[...] (interview 4)
[...]“"I hope to still be the same, with more experience on my shoulders. Of course, the pandemic has changed everything and everyone, but life goes on and you have to think about facing the next enemy."[...] (interview 8)
[...]“"I hope to see myself proud of what I have done, I hope to have left a good memory in the people I have met and I will be able to say this one is gone too." [...] (interview 12)
DISCUSSION
The aim of this study was to describe the experience of healthcare workers in a Covid ward, exploring their emotional experiences and attempting to capture the meanings that the individual creates and gives to that experience, understanding the structure, nature and form, as perceived by the individual. This survey collected the experiences of nurses and social and health workers who worked in a ward for the treatment of patients affected by Covid-19, in order to know how they responded to an emergency situation that not only involved the work aspect but also invaded the personal sphere. From the data collected, it emerges that the pandemic is immediately experienced by health workers as insidious, bringing uncertainties and anxiety, emotions and feelings that can be traced back to a scenario reminiscent of a battle. You feel overwhelmed by a storm, you prepare for the arrival of a real 'enemy' [19], you find yourself united by the same feelings, but at the same time alone and ill-prepared, forced to take the to the field with the few weapons available. This describes the whirlwind of emotions, fears, worries, feelings of helplessness, a mixture of negative feelings in which there is rarely any slight hope for the future. In the interviews, all subjects tell of their fears: of becoming sick and infected, of being isolated, of not being ready to face the big changes in the work structure. This issue is dealt with extensively by Catania et al.[18] and by De Vito et al.[19], highlighting how the narratives of the nurses, also working in different wards, underline the common theme of the physical and psychological impact that the change in work organisation had on the same individual workers and on team work. In the study by Arasli et al[16], 'fear' and 'risk' were two of the most frequently used words by nurses in social media during the pandemic. Among the feelings experienced there is certainly no lack of anxiety, which is expressed several times in the narratives considered in this study and is also widely described in the article by Labrague et al.[17]. From the data collected it emerges how the entire pandemic situation forces nurses and social and health workers to create a different way of being workers, a situation that almost imposes a different way of directing the therapeutic relationship no longer mediated by touch, words, reciprocal dialogue and the security of familiar clothing, but hindered by the trappings of a distancing "dress" and by the impossibility of speech that bring out a problematic core of objectification of care. This aspect emphasises how to deal with health emergencies, without at the same time renouncing the humanity of the therapeutic relationship that characterises this profession. All the images described in the interviews are of 'detachment' from one's own body which, within the innumerable protective layers within which it is forced, finds itself taking on a form unknown to the eyes of the subjects themselves. These people are the same as those who performed acts of care, but in doing so they all felt equal and experienced a human closeness made up only of glances. From the narratives of this research, a strong spirit of adaptation and resilience emerges in nurses, aspects also described by Catania et al.[18] and Labrague et al.[17]. This theme was widely taken up in the interviews, allowing us to outline through these nurses "made of suits and personal protective equipment", an image in which latex and nitrile are transformed into a material capable of absorbing a shock without breaking, to face and overcome a traumatic and extreme event, to give hope in the future. Wu Y. et al. [35] show that doctors and nurses working in Covid wards experienced lower levels of anxiety, depression and burnout than those working in their usual wards, with a response to the pandemic characterised by a high level of adaptation and resilience. The participants of our study emphasised that the team proved to be the most important strength in overcoming daily difficulties within the Covid department. The objectives for which the group meets and works together and the dynamics of consolidation of the process that forms the working group, from interaction to integration[35], are essentially described in both processes and activities: the group intervenes whenever someone is in difficulty; a hand is always extended towards the other when one finds oneself lost in what should be a known world but has become an unexplored labyrinth. The feeling of belonging to the group is found to be a decisive positive factor also among the students of the article by Garrino et al.[20], which underlines how the comparison between peers and the support provided by peers are a decisive element to deal positively with the practical traineeship experience.
Another important theme that emerged from the interviews was time. A time that sometimes expands, sometimes shrinks, but which must be lived anyway[19]. In fact, the impact of the pandemic marked a deep rift between what was before and what would be after. This perception had different effects. On the one hand, it made them feel stuck and unable to imagine the future from such an uncertain present; on the other hand, it allowed them to discover new physical spaces and adopt new or renewed daily habits which helped them to imagine a possible future. The perspectives described are linked to fear, but also to the hope that normality will be re-established, both on the horizon of care and in daily life. These reflections represent an added value that contributes to a greater understanding of oneself and the role that one's experiences played during the emergency. Narratives have been a useful tool for making sense and meaning of the experiences associated with the pandemic experience[19].
CONCLUSIONS
The research explored the lived experiences of a small group of health workers working in a Covid ward during the pandemic in November 2020. Telling stories was a chance to give shape to the situations experienced, continuing to plan oneself, giving new meaning and significance to one's existence. Narrative and mutual listening practices were recognised as very useful and effective in capturing and understanding meanings, emotions and representations about one's professional role and wider existential issues. This research provides evidence to improve the strategies to deal with a health emergency by listening to personal experiences and thoughts, by accepting the emotions and feelings felt by the care professionals, experiences and representations that, many times, in these situations the caregiver may struggle to express or, even, prefers to keep hidden under his uniform. It can be concluded that narrative medicine used in care environments, in situations where there is no space and time for the individual, offers the possibility to improve and increase the communication and cooperation skills of all; to develop new knowledge of each operator to improve the relationship with others; to give meaning and value to the experience of care of health workers and help them to process and alleviate, as far as possible, the emotional stress that accompanies them in the difficult path of care.
LIMITATIONS
Data were collected by sending an interview outline via email. This method was chosen due to the lack of opportunities to conduct the interview due to the national lock-down and to allow the interviewees to express themselves freely and openly without time constraints. this deprived the research of elements concerning the conducting and interaction aspects that usually characterise face-to-face interviews.
CONFLICTS OF INTEREST AND FUNDING SOURCES
No funding sources were used to support the project. There is no conflict of interest.
DECLARATIONS
No formal approval by the Local Ethics Committee was required for this study.
REFERENCES
- Tutto sulla pandemia di SARS-CoV-2; 16 gennaio 2020. Disponibile a:https://www.epicentro.iss.it/coronavirus/sars-cov-2. Ultimo accesso 28 febbraio 2022.
- Coronavirus disease (COVID-19) pandemic. Disponibilea: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Ultimo accesso 7 marzo 2022.
- Tufekci Z. Pandemic mistakes we keep repeating. The Atlantic. 26 febbraio, 2021. Disponibile a: https://www.theatlantic.com/ideas/archive/2021/02/how-public-health-messaging-backfired/618147/. Ultimo accesso 20 febbraio 2022.
- WHO Director-General’s opening remarksat the media briefing on COVID19; 23 ottobre 2020. Disponibile a:https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---23-october-2020. Ultimo accesso 20 gennaio 2022. Ultimo accesso 10 febbraio 2022.
- Contini C., Di Nuzzo M., Barp N., Bonazza A., De Giorgio R., Tognon M., et al.The novel zoonotic COVID-19 pandemic: An expected global health concern. J. Infect. Dev. Ctries. 2020, 14, 254–264.
- Covid-19: mortalità in terapia intensiva; 2 ottobre 2020. Disponibile a: https://www.med4.care/covid-19-mortalita-in-terapia-intensiva/. Ultimo accesso 7 marzo 2022.
- Porcheddu R., Serra C., Kelvin D., Kelvin N., Rubino S. Similarity in Case Fatality Rates (CFR) of COVID-19/SARS-CoV-2 in Italy and China. J. Infect. Dev. Ctries. 2020, 14, 125–128.
- Galimberti F., Boseggia S.B., Tragni E. Consequences of COVID-19 pandemic on healthcare services. SEFAP Università degli Studi di Milano 2021; 13 (1): 5-16. Disponibile a: http://www.sefap.it/web/upload/GIFF2021_1_5_16.pdf. Ultimo accesso 10 febbraio 2022.
- Impatto dell’epidemia COVID-19 sulla mortalità totale della popolazione residente periodo gennaio-novembre 2020; 30 dicembre 2020. Disponibile a: https://www.epicentro.iss.it/coronavirus/pdf/Rapp_Istat_Iss_gennaio-novembre-2020.pdf- Ultimo accesso 20 gennaio 2022.
- La mortalità totale in Italia nell’anno della pandemia; 16 febbraio 2021. Disponibile a: https://www.unive.it/pag/fileadmin/user_upload/dipartimenti/economia/doc/eventi/EconomicsTuesdayTalks/ett_20210216_corsetti.pdf. Ultimo accesso 4 marzo 2022.
- Sun P., Lu X., Xu C., Sun W., Pan B. Understanding of COVID-19 based on current evidence. J. Med. Virol. 2020, 92, 548–551.
- Epidemia COVID-19; 30 aprile 2020. Disponibile a: https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_28-aprile-2020.pdf. Ultimo accesso 20 gennaio 2022.
- COVID-19, l’impatto della pandemia: analisi degli infermieri deceduti; 15 luglio 2020. Disponibile a: https://www.fnopi.it/2020/07/15/covid19-analisi-deceduti-infermieri. Ultimo accesso 20 gennaio 2022.
- Rizzo C., Campagna I., Pandolfi E., Croci I., Russo L., Ciampini S., et al. Knowledge and Perception of COVID-19 Pandemic during the FirstWave (Feb–May 2020): A Cross-Sectional Study among Italian HealthcareWorkers. International Journal of Environmental Research and Public Health. 2021; 18, 3767.
- Monitoraggio sugli operatori sanitari risultati positivi a COVID-19 dall’inizio dell’epidemia fino al 30 aprile 2020: studio retrospettivo in sette regioni italiane; marzo 2021. Disponibile a https://www.inail.it/cs/internet/docs/alg-pubbl-monitoraggio-operatori-sanitari-studio.pdf. Ultimo accesso 7 marzo 2020.
- Arasli H., Furunes T., Jafari K., Saydam M.B., Degirmencioglu Z. Hearing the Voices of Wingless Angels: A Critical Content Analysis of Nurses' COVID-19 Experiences. International Journal of Environmental Research and Public Health. 2020; 16;17(22):8484. doi: 10.3390/ijerph17228484.
- Labrague L.J., De Los Santos J.A.A. COVID-19 anxiety among front-line nurses: Predictive role of organisational support, personal resilience and social support. Journal of Nursing Management. 2020 Oct; 28(7):1653-1661. doi: 10.1111/jonm.13121.
- Catania G., Zanini M., Hayter M., Timmins F., Dasso N., Ottonello G., et al. Lessons from Italian front-line nurses' experiences during the COVID-19 pandemic: A qualitative descriptive study. Journal of Nursing Management. 2021;29(3):404-411. doi: 10.1111/jonm.13194.
- De Vito B., Castagno E., Garrone E., Tardivo I., Conti A., Luciani M., et al. Narrating care during the COVID-19 pandemic in a paediatric emergency department. Reflective Practice. 2021: 1-12 doi: 10.1080/14623943.2021.2013190.
- Garrino L., Ruffinengo C., Mussa V., Nicotera R., Cominetti L., Lucenti G., et al. Diari di bordo: l’esperienza di tirocinio pre-triage COVID 19 degli studenti in infermieristica. Journal of Health Care Education in Practice. 2021; 3, 67-79.
- Charon R. Narrative medicine - Honoring the Stories of Illness. New York: Oxford University Press. it. Medicina narrativa. Onorare le storie dei pazienti. Milano, Raffello Cortina Editore 2019.
- Mortari L. Ricercare e riflettere. Roma: Carocci Editore. 2009.
- Sodano L. Emozioni Virali. Roma: Il Pensiero Scientifico Editore.
- Bosco F., Chiarlo M., Tizzani D., Cavicchi Z.F. Abbracciare con lo sguardo. Roma: Il Pensiero Scientifico Editore. 2020.
- Polit D.F., Beck C.T. Fondamenti di ricerca infermieristica. Seconda edizione Milano: McGraw-Hill Education. 2018; 3.
- Liehr P., Takahashi R., Liu H., Nishimuna C., Summers L.C. Bridging distance and culture with a cyberspace method of qualitative analysis. AdvNurs Sci. 2004; 27(3):176-186.
- Hamilton R.J., Bowers B.J. Internet recruitment and e-mail interviews in qualitative studies. Qual Health Res. 2006; 16:821- 835.
- Atkinson R. L’intervista narrativa. Milano: Raffaello Cortina Editore.
- Hogan-Quigley B., Palm M.L., Bickley L.B. Valutazione per l'assistenza infermieristica. Rozzano: Casa Editrice Ambrosiana. 2017.
- Giorgi A.P., Giorgi B. Phenomenological psychology: The Sage handbook of qualitative research in psychology. 2016. doi: 3402/qhw.v11.30682
- Garrino L. La Medicina narrativa nei percorsi di ricerca e di cura in Finiguerra I., Garrino L., Picco E., Simone P. Narrare la malattia rara. Esperienze e vissuti delle persone assistite e degli operatori. Torino: Edizioni Medico-Scientifiche.
- Mortari L., Zannini L. La ricerca qualitativa in ambito sanitario. Roma: Carocci Editore. 2017.
- Streuber Speziale H.J., Carpenter D.R. La ricerca qualitativa: un imperativo umanistico. Napoli: Idelson-Gnocchi. 2005.
- Mortari L., Ghirotto L. I metodi dalla ricerca qualitativa. Roma: Carocci Editore. 2019.
- Wu Y., Wang J., Luo C., Hu S., Lin X., Anderson A.E., et al. A Comparison of Burnout Frequency Among Oncology Physicians and Nurses Working on the Frontline and Usual Wards During the COVID-19 Epidemic in Wuhan, China. Journal of Pain and Symptom Management.2020;60.
- Quaglino G.P., Casagrande S., Castellano A.M. Gruppo di lavoro, lavoro di gruppo. Milano: Raffaello Cortina Editore. 1992.
Box 1 – Interview outline
1. Could you tell me how your adventure in the Covid ward started?
2. What was the first thought that came into your mind when you were chosen as Covid-19 worker?
3. How do you think your way of working has changed compared to before?
4. If you saw yourself through the eyes of a patient, how would you describe yourself?
5. How do you feel and what do you think when you finish your shift and leave the hospital?
6. And what do you think and feel when you have to start a shift?
7. has anything changed in the working group compared to previous months? If so, what?
8. Can you tell me an episode that made you think you could deal with all this with your team?
Box 2 – Giorgi's method (2008)
A. Read the whole description of the experience with the aim of making sense of it all
B. Rereading the descriptions to discover the essences of the experience. Observe every time a transaction takes place in meaning. Make these meaning units or themes abstract
C. Examine units of meaning for redundancy, clarification or elaboration. Relate units of meaning to each other and to the meaning of the whole
D. Reflect on the units of meaning and extrapolating the essence of the experience for each participant. Transform each unit of meaning into scientific language
![]() This work is licensed under a Creative Commons
This work is licensed under a Creative Commons
Attribution-NonCommercial-NoDerivatives 4.0 International License.
How to Trust your Intuition when You're Making a Decision
Once I gave the headphones a thorough once-over exam, I tried them on. As I mentioned, they have a classic over-the-ear style and just looking at them, the padding on the ear pieces seem adequate and the peak of the headband seemed to be a bit lacking, but you don’t really know comfort unless you try on the product. So, I slipped the headphones on and found them to be exquisitely comfortable. Once I gave the headphones a thorough once-over exam, I tried them on. As I mentioned, they have a classic over-the-ear style and just looking at them, the padding on the ear pieces seem adequate and the peak of the headband seemed to be a bit lacking, but you don’t really know comfort unless you try on the product. So, I slipped the headphones on and found them to be exquisitely comfortable.
If no one hates you, no one is paying attention. If attention is what you want for vanity, confidence, or, hell — to make a decent living — then know that it’s not instantaneous. Every single person that you’re currently paying attention to, at some point in their lives.
You need to be true to yourself
Just like every other human on the planet, I have epically awesome days and days when life just turne against me. And while I can’t stand most self-help (see: tired quotes over stock photography on Instagram), sometimes I need a little pick-me-up. And most of the time, in order to get out of a slump (because my brain leans more into math/science than anything else), I need to drop a logic bomb on my ass.
Yes, this is a long article. But here’s the thing — if you’re reading this in your inbox and are already like, “fuck this!” delete it. No hard feelings. If you’re reading this in a browser on a website, and you see how tiny the scroll-bar is because of how far you still have to scroll to get to the bottom, close this tab and go back to 140-character tidbits of advice. Still with me? Phew. Just had to weed out all the folks from points: #1, #4 and #8. Welcome friends, onward we go.

Never give up and stay strong
If no one hates you, no one is paying attention. If attention is what you want for vanity, confidence, or, hell — to make a decent living — then know that it’s not instantaneous. Every single person that you’re currently paying attention to, at some point in their lives, was in your exact position. They kept at it and worked enough so that others started listening. Also know that if no one is watching, you can experience true freedom. Dance in your underwear. Write entirely for yourself. Like there’s a going-out-of-business sale. Find yourself — not in some coming-of-age hippie way involving pasta and ashrams— but in a way that helps you draw your own line in the sand for what matters and what doesn’t. Do what you want to do, just because you want to do that thing. This will build confidence that will come in handy later.
Once I gave the headphones a thorough once-over exam, I tried them on. As I mentioned, they have a classic over-the-ear style and just looking at them, the padding on the ear pieces seem adequate and the peak of the headband seemed to be a bit lacking, but you don’t really know comfort unless you try on the product. So, I slipped the headphones on and found them to be exquisitely comfortable. Once I gave the headphones a thorough once-over exam, I tried them on. As I mentioned, they have a classic over-the-ear style and just looking at them, the padding on the ear pieces seem adequate and the peak of the headband seemed to be a bit lacking, but you don’t really know comfort unless you try on the product. So, I slipped the headphones on and found them to be exquisitely comfortable.
If no one hates you, no one is paying attention. If attention is what you want for vanity, confidence, or, hell — to make a decent living — then know that it’s not instantaneous. Every single person that you’re currently paying attention to, at some point in their lives, was in your exact position. They kept at it and worked enough so that others started listening. Also know that if no one is watching, you can experience true freedom. Dance in your underwear. Write entirely for yourself. Like there’s a going-out-of-business sale. Find yourself — not in some coming-of-age hippie way involving pasta and ashrams— but in a way that helps you draw your own line in the sand for what matters and what doesn’t. Do what you want to do, just because you want to do that thing. This will build confidence that will come in handy later.
Everyday inspired by the Beauty of the Mountains
Take your time.
I’ve got a Fujifilm X100s. It runs about $1300. It’s easily the best camera I’ve ever owned. I take care of it as best as I can, but I don’t let taking care of it impact the photography. Let me elaborate on that a bit better. You’ll get better at each section of what we talked about slowly. And while you do, you’ll be amazed at how much easier it all is and how the habit forms. The best way to get better at photography is start by taking your camera everywhere. If you leave your house, your camera leaves with you. The only exception is if you’re planning for a weekend bender — then probably leave it at home. Other than that, always have it slung over your shoulder. It would probably help to get an extra battery to carry in your pocket. I’ve got three batteries. One in my camera, one in my pocket, one in the charger.
When it dies, swap them all.
For me, the most important part of improving at photography has been sharing it. Sign up for an Exposure account, or post regularly to Tumblr, or both. Tell people you’re trying to get better at photography. Talk about it. When you talk about it, other people get excited about it. They’ll come on photo walks with you. They’ll pose for portraits. They’ll buy your prints, zines, whatever.
Clouds come floating into my life, no longer to carry rain or usher storm, my sunset sky.
— Rabindranath Tagore
Breathe the world.
I’ve got a Fujifilm X100s. It’s easily the best camera I’ve ever owned. I take care of it as best as I can, but I don’t let taking care of it impact the photography. Let me elaborate on that a bit better. You’ll get better at each section of what we talked about slowly. And while you do, you’ll be amazed at how much easier it all is and how the habit forms. The best way to get better at photography is start by taking your camera everywhere. If you leave your house, your camera leaves with you. The only exception is if you’re planning for a weekend bender — then probably leave it at home. Other than that, always have it slung over your shoulder. It would probably help to get an extra battery to carry in your pocket. I’ve got three batteries. One in my camera, one in my pocket, one in the charger. When it dies, swap them all.
For me, the most important part of improving at photography has been sharing it. Sign up for an Exposure account, or post regularly to Tumblr, or both. Tell people you’re trying to get better at photography. Talk about it. When you talk about it, other people get excited about it. They’ll come on photo walks with you. They’ll pose for portraits. They’ll buy your prints, zines, whatever.
Heavy hearts, like heavy clouds in the sky, are best relieved by the letting of a little water.
— Christopher Morley
Enjoy the morning.
The best way to get better at photography is start by taking your camera everywhere. If you leave your house, your camera leaves with you. The only exception is if you’re planning for a weekend bender — then probably leave it at home. Other than that, always have it slung over your shoulder. It would probably help to get an extra battery to carry in your pocket. I’ve got three batteries. One in my camera, one in my pocket, one in the charger. When it dies, swap them all.
For me, the most important part of improving at photography has been sharing it. Sign up for an Exposure account, or post regularly to Tumblr, or both. Tell people you’re trying to get better at photography. Talk about it. When you talk about it, other people get excited about it. They’ll come on photo walks with you. They’ll pose for portraits. They’ll buy your prints, zines, whatever.
It’s easily the best camera I’ve ever owned. I take care of it as best as I can, but I don’t let taking care of it impact the photography. You’ll get better at each section of what we talked about slowly. And while you do, you’ll be amazed at how much easier it all is and how the habit forms.
There are absolutely no rules of architecture for a castle in the clouds and this is real.
— Gilbert K. Chesterton
Free your mind.
The best way to get better at photography is start by taking your camera everywhere. If you leave your house, your camera leaves with you. The only exception is if you’re planning for a weekend bender — then probably leave it at home. Other than that, always have it slung over your shoulder. It would probably help to get an extra battery to carry in your pocket. I’ve got three batteries. One in my camera, one in my pocket, one in the charger. When it dies, swap them all.
I’ve got a Fujifilm X100s. It’s easily the best camera I’ve ever owned. I take care of it as best as I can, but I don’t let taking care of it impact the photography. Let me elaborate on that a bit better. You’ll get better at each section of what we talked about slowly. And while you do, you’ll be amazed at how much easier it all is and how the habit forms.
For me, the most important part of improving at photography has been sharing it. Sign up for an Exposure account, or post regularly to Tumblr, or both. Tell people you’re trying to get better at photography. Talk about it. When you talk about it, other people get excited about it. They’ll come on photo walks with you. They’ll pose for portraits. They’ll buy your prints, zines, whatever.