THE CHILDBIRTH UTILIZATION IN HEALTH FACILITIES IN THE WORKING AREA OF SUNGAI LOKAN PHC TANJUNG JABUNG TIMUR REGENCY: A CROSS SECTIONAL STUDY
Lia Artika Sari1*, Yuli Suryanti1, Enny Susilawati1
- Department of Midwifery, Health Polytechnic of Jambi, Indonesia
* Corresponding author: Lia Artika Sari, Department of Midwifery, Health Polytechnic of Jambi, Indonesia, liaartikasari57@gmail.com
Cita questo articolo
ABSTRACT
Introduction: The low number of deliveries assisted by midwives or health workers is an indicator of the low utilization of health facilities by mothers in labor. This study analyzes the factors related to the utilization of childbirth in health facilities in the Sungai Lokan Community Health Center Work Area, Tanjung Jabung Timur Regency.
Materials and Methods: This research is an analytic observational using a cross-sectional approach involving 74 participants. The research was conducted from January to July 2019 in the Sungai Lokan Health Center Work Area, Tanjung Jabung Timur Regency.
Results: The results showed that the factor of the utilization of childbirth in health facilities was related to family culture (p = 0.0001) and family support (p = 0.003), while the service access factor was not related (p = 0.364).
Conclusion: The role of health workers in socializing the importance of utilizing health facilities as a place of delivery is significant in reducing maternal mortality
Keywords: Health Facilities, Family Culture, Family Support, Access To Services
INTRODUCTION
Maternal Mortality Rate (MMR) is one indicator of success in maternal health programs. MMR is a recapitulation of maternal deaths during pregnancy, childbirth, and the puerperium due to pregnancy, delivery, and postpartum problems or their management per 100,000 live births. Reducing maternal mortality due to complications of pregnancy and childbirth is one of the eight targets of the Millennium Development Goals (MDGs) [1]. Family planning, especially for postpartum mothers and unmet need groups, integrated reproductive health services; strengthened village midwives' function, strengthened the referral system, and reduced financial barriers [2,3].
The achievement of the Millennium Development Goals (MDGs) health workforce target needs to receive support from service providers who are health service providers who have a major role in achieving health development goals [4]. Health workers are also providers of health services to patients in accordance with their professional authority to make optimal health efforts. Midwife is one of the non-medical health workers in accordance with their competence and authority to provide midwifery services which are an integral part of health services [5,6]. Every day, some 7,000 babies die in the first month of life. In 2019, an estimated 2.4 million newborns died worldwide. High Maternal Mortality Rate (MMR) and Infant mortality (IMR) is caused by complications in pregnancy and labor [7]. More in the MDG's target on MMR, as stated in the Roadmap to Accelerate Achievement of the Millennium Development Goals in Indonesia, is to reduce from 228 per 100,000 live births in 2007 to 102 per 100,000 live births in 2015. Coverage of deliveries by health workers in health care facilities in Indonesia based on data from the Profile Indonesian Health in 2017 amounted to 5,078,636 with deliveries assisted by health workers totaling 4,222,506 (83.14%). In 2019, 90.95% of deliveries were assisted by health workers. Meanwhile, pregnant women who underwent childbirth assisted by health workers in health care facilities were 88.75% [1]. Thus, around 2.2% of deliveries are assisted by health workers but are not carried out in health care facilities. The coverage of deliveries in Jambi Province based on Indonesia's health profile data in 2017 was 69,774, with deliveries assisted by health workers at health facilities totaling 25,387 (76.37%) [8]. The government targets 85% of deliveries to be carried out in health care facilities. For this reason, the government seeks to improve the quality of quality health care facilities. It is a matter of being available and affordable [9]. The current condition, Puskesmas, as a primary health service facility owned by the government, already exists in every sub-district; it is just that it is still not evenly distributed so that it is less accessible to the public [10]. As a state administrator, the government is obliged to ensure equity and quality of health services for the community. Physically, equitable distribution of health services can be interpreted as affordability in topographical, demographic, and geographical aspects. Physical topographical affordability is the proximity of the population settlements to health service facilities. Affordability in the demographic aspect means that the Puskesmas can accommodate and serve the health needs of the entire population in the work area [9,11,12]. Another critical factor is the public's misconception about the competence of traditional birth attendants that they are birth attendants that are safe, inexpensive, and able to provide services that health workers cannot provide. It is exacerbated by the absence of family support, especially mothers or mothers-in-law to take advantage of health facilities as a place to give birth.
Several previous studies found that delivery coverage at health facilities was influenced by accessibility factors [13], family support [14,15], mothers knowledge [16]. The results of the study [17] show that one of the causes of neonatal death, in addition to the distance of access to health facilities, is also influenced by birth attendants, namely giving birth to a traditional birth attendant with a risk of causing neonatal death by 12.4 times compared to not giving birth to a traditional birth attendant.
Tanjung Jabung Timur Regency, Indonesia has 17 Health centers, with the number of deliveries in 2018 totaling 4,069, with deliveries assisted by health workers in health facilities totaling 1,512 (37.16%). Specifically, Sungai Lokan Village has one main health center and one secondary Health center with total deliveries in 2018 of 29.58%, namely out of 71 deliveries, health workers assisted only 21 deliveries in health facilities [18]. The low number of deliveries assisted by midwives or health workers is an indicator of the low utilization of health facilities by mothers in labor.
Based on the existing phenomena, we tried to examine the factors related to the utilization of childbirth in health facilities in the Sungai Lokan Community Health Center Work Area, Tanjung Jabung Timur Regency”.
MATERIALS AND METHODS
The research design is a cross-sectional survey. Data collection was carried out by the research team assisted by two midwives from January to July 2019 in the Sungai Lokan Health Center Work Area, Tanjung Jabung Timur Regency. The research population was all mothers who gave birth in the Sungai Lokan Public Health Center, Tanjung Jabung Timur Regency, with a sample of 74 mothers who gave birth and at the same time as respondents who were selected by total sampling with inclusion criteria, namely the mother's place of residence is accessible, the mother is in good health, the mother who lives at home with her in-laws while the mother who does not live at home with her in-laws was excluded from the study. Before the research was carried out, the researcher first asked the mother's consent as a prospective respondent, after the mother signed the consent letter to become a respondent, then the researcher conducted interviews using a questionnaire. The research questionnaire consisted of a questionnaire on Utilization of childbirth in health care facilities consisting of 10 questions, a family culture questionnaire consisting of 10 questions, family support consisting of 10 questions, and an Access to the service questionnaire consisting of 10 questions. when the questionnaire was distributed, the mother was accompanied by a member of the researcher until the questionnaire was completed by the mother.
The study was performed in accordance with the ethical considerations of the Helsinki Declaration. No economic incentives were offered or provided for participation in this study. Ethical eligibility is obtained from the Health Research Ethics Commission of the Health Polytechnic, Jambi Ministry of Health with the number: LB.02.06 / 2/110/2019.
Statistical analysis
Data are presented as numbers and percentages for categorical variables. Continuous data are expressed as the mean ± standard deviation (SD), or median with Interquartile Range (IQR). The chi-square test and Fishers exact test were performed to evaluate significant differences of proportions or percentages between two independent groups. Particularly Fishers exact test was used where the chi-square test was not appropriate. The variables measured were adequate delivery facilities as the dependent variable and family culture, family support, and access to services as independent variables. All tests with p-value (p) < 0.05 were considered significant. Statistical analysis was performed using SPSS app version 16.0.
RESULTS
The research results are then presented in the form of distribution tables and cross-tabulations and then narrated. The following will present research data on research variables, as follows:

Table 1. Frequency distribution of research variables in the working area of Sungai Lokan Public Health Center, Tanjung Jabung Timur Regency.
Table 1 shows that of the 74 respondents, most (71.6%) of respondents will not use health facilities, most (62.2%) of respondents with unsupportive culture, most (58.1%) of respondents do not. Most of them received support from their families (77.0%) were close to the place of service.

Table 2. Results of the analysis of the relationship between the utilization of childbirth in health care facilities with a family culture, family support, and access to services in the working area of
the Sungai Lokan Community Health Center, Tanjung Jabung Timur Regency
In Table 2, it can be seen from 46 respondents with a culture that does not support there are 40 people (87.0%) respondents who will not use health facilities. Meanwhile, out of 28 respondents with a supportive culture, 15 people (53.6%) will use health facilities. The results of statistical tests using the chi-square test obtained a value of p = 0.0001 (p <0.05), meaning that there is a socio-cultural relationship with the use of delivery services in health facilities. Respondents who do not receive family support have 39 people (90.7%) respondents who will not use health facilities. Meanwhile, of the 31 respondents who received family support, 17 (54.8%) respondents would use health facilities. The results of statistical tests using the chi-square test obtained a value of p = 0.003 (p <0.05), meaning that there is a relationship between family support and delivery services in health facilities. Of the 17 respondents with long distances to the four health facilities, 14 (82.4%) respondents would not use the health facilities. Meanwhile, out of 57 respondents with proximity to health facilities, 39 (68.4%) respondents would not use health facilities. The statistical test results using the Fisher Exact test obtained a value of p = 0.364 (p> 0.05), meaning that there is no relationship between distance to the place of service and the utilization of delivery services in health facilities.
DISCUSSION
The question components in family culture variables include the habits of family members to give birth still choose a traditional birth attendant as a birth attendant. In this study it was found that the role of traditional birth attendants was very central and became the family's choice as birth attendants. family habits in giving birth to traditional birth attendants that have been carried out for generations. This has become a culture not only for the respondent's family but also for most of the people in the study area and Indonesia in general. Cultural factors have a very big influence in the selection of birth attendants. Moreover, in rural areas, the position of traditional birth attendants is more respectable, their position is higher than that of midwives, so that from examinations, delivery assistance to postpartum care, many ask for help from traditional birth attendants.
Based on the research results on the socio-cultural community in the working area of the Sungai Lokan Public Health Centre, when approaching delivery, they choose to give birth at home, in addition to being hereditary, because they feel comfortable giving birth at their own home. Some dukuns accompany mothers during childbirth, and some even choose to give birth to be assisted by shamans alone. They also think that their previous children born with the help of a dukun are no different from those who are now being helped by a midwife, apart from feeling comfortable giving birth at their own home because they feel ashamed and reluctant to give birth in a health facility.
The limited use of the national language is also one of the difficulties for the community to communicate with health workers, most of who are not from the local area. So that communication difficulties also make people more comfortable giving birth at their own home and choosing a shaman to help the delivery process. It is in line with Yeni Aryani's research [19], which found that statistical tests showed a relationship between culture and the choice of place of delivery (p = 0.028). The results of the OR (Odds Ratio) of 3.162 indicate that mothers who receive support from culture have a 3.162 times greater chance of choosing a place of delivery in a health facility compared to mothers who do not receive support from culture. In line with research in Rural Uganda which states that for both men and women in the village, the cultural behaviour patterns of the community have the most substantial impact on birth choices [20]. A woman's relationship with her partner and family is also a factor in whether the mother will use health facilities for the birth process or not. In the family role variable, one component of the question in the questionnaire is the husband's role in determining the choice of place to give birth. The husband's role is very dominant in this study determining the place of delivery for the mother. The husband is the head of the household in a family, so the rules in the household should have deliberation with the husband. Therefore, how important is the role of the husband and family in making decisions for choosing the place of delivery. Based on this and previous studies, husband/family support can influence respondents to use health facilities as a place of delivery. It is due to the husband's/family's lack of knowledge about the importance of using health facilities, especially for childbirth due to lack of knowledge of Husband/family regarding the importance of health utilization and the advantages of giving birth in health facilities. Based on the research results from 74 respondents, most of the respondents did not receive support from their families in the working area of Sungai Lokan Public Health Centre, Tanjung Jabung Timur Regency, with a p-value <0.05. In line with previous research at Puskesmas XIII Koto Kampar, obtained p-value (0.010 < 0.05), this means that there is a socio-cultural influence with the selection of birth attendants [21].
The results of this study are also in line with previous research in the working area of the Muara Ancalong Health Centre, Kutai Timur Regency, which found that family support affected the choice of place of delivery with a p-value of 0.019, namely husband and parents, this indicates that the influence of the closest family is considerable on respondents' decision making in choosing a place to give birth [21]. Another study in Kenya showed that family support in the form of funds was associated with the utilization of childbirth in health facilities [22]. The distance from a mother's house to a health facility is closely related to transportation costs and the time it takes to reach it. The closer the distance of a mother's house to a health facility is, the cheaper the costs. Accessibility based on geographical dimensions is related to time and space, which is believed to shape access to health services significantly. If these obstacles are overcome, someone will still think to decide whether the distance is an obstacle. A study states that the low utilization of health services is due to the existence of barriers for the community in accessing preventive, curative, and promotive health services [13].
Based on the study results, from 74 respondents, most of the respondents were close to the place of service in the working area of Sungai Lokan Public Health Center, Tanjung Jabung Timur Regency. It will undoubtedly increase pregnant women's access to give birth to health facilities, but in reality, this condition is very contrary to the respondent's decision not to use health facilities as a place to give birth.
This study indicates that there is no significant relationship between a mother's access to health facilities and the choice of place of delivery. According to the researcher's assumptions, this occurs because people travel long distances by using transportation to get to the garden. Affordability is based on the perception of distance and the presence or absence of private or public vehicles to reach the nearest health facility. Respondents who choose delivery assistance by traditional birth attendants are generally people whose homes are closer to the traditional birth attendant, while respondents who choose birth assistance by midwives need more time to get services because of the longer distance.
Unlike previous research in the work area of the Kawangu Health Centre, the utilization of childbirth in health facilities was influenced by the ability to access health services (p < 0.001) [16]. In this study, transportation limitations with high costs and poor road structures caused pregnant women to prefer to give birth. The difference in the results of this study is that the ability to access services in our study is already high because the distance from pregnant women's homes to the PHC is very close and does not cost a lot, even though the dominant mother decides to be more comfortable giving birth at home.
Conclusions
Most of the respondents did not use health facilities in the working area of Sungai Lokan Health Centre, Tanjung Jabung Timur Regency. Utilization of delivery services in health facilities in the working area of Sungai Lokan Public Health Center, Tanjung Jabung Timur Regency, is related to family culture and family support, while access to services is not related.
Limitation
In this study, there are limitations such as the presence of some areas that cannot be reached by the research team so they cannot participate in the study. Then in this study using a cross-sectional design so that the information obtained by researchers is only limited to data when the research is conducted.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Competing interests statement
There are no competing interests for this study.
REFERENCES
- Kemenkes RI. Hasil utama RISKESDAS 2018. Jakarta: Kementerian Kesehatan Badan Penelitian dan Pengembangan Kesehatan. Jakarta; 2018.
- Paul VK, Sachdev HS, Mavalankar D, Ramachandran P, Sankar MJ, Bhandari N, et al. Reproductive health, and child health and nutrition in India: meeting the challenge. The Lancet. 2011;377(9762):332–49.
- Lule E, Ramana GN V, Ooman N, Epp J, Huntington D, Rosen JE. Achieving the millennium development goal of improving maternal health: determinants, interventions and challenges. 2005;
- Tangcharoensathien V, Mills A, Palu T. Accelerating health equity: the key role of universal health coverage in the Sustainable Development Goals. BMC medicine. 2015;13(1):1–5.
- Mansoor GF, Hashemy P, Gohar F, Wood ME, Ayoubi SF, Todd CS. Midwifery retention and coverage and impact on service utilisation in Afghanistan. Midwifery. 2013;29(10):1088–94.
- ten Hoope-Bender P, de Bernis L, Campbell J, Downe S, Fauveau V, Fogstad H, et al. Improvement of maternal and newborn health through midwifery. The Lancet. 2014;384(9949):1226–35.
- Unicef. Newborn and maternal mortality snapshot [Internet]. 2019. Available from: https://www.unicef.org/health/maternal-and-newborn-health
- Dinkes Kota Jambi. Profil Kesehatan Kota Jambi. Jambi; 2018.
- Laksono AD, Mubasyiroh R, Laksmiarti R, Suharmiati EN, Sukoco NE. Aksesibilitas Pelayanan Kesehatan di Indonesia. Yogyakarta: PT Kanisius. 2016.
- Izati ARM. Trend Cakupan Kunjungan Ibu Hamil (K4) Dan Pertolongan Persalinan Oleh tenaga Kesehatan Di Propinsi Jawa Timur. Jurnal Ilmiah Kesehatan Media Husada. 2018;7(1):1–10.
- Senewe FP, Elsi E. Descriptive Analysis to environment health in less development, borderlands, archipelagoes and remote areas (DTPK-T). Media Litbangkes. 2014;24(3):153–60.
- Agustina R, Dartanto T, Sitompul R, Susiloretni KA, Achadi EL, Taher A, et al. Universal health coverage in Indonesia: concept, progress, and challenges. The Lancet. 2019;393(10166):75–102.
- Laksono AD, Sandra C. Analisis Ekologi Persalinan di Fasilitas Pelayanan Kesehatan di Indonesia. Buletin Penelitian Sistem Kesehatan. 2020;23(1):1–9.
- Suci CM. Hubungan Pengetahuan Ibu Dan Dukungan Keluarga Dengan Pemilihan Penolong Persalinan di Wilayah Kerja Puskesmas Pintu Padang Kabupaten Pasaman. Universitas Andalas; 2019.
- Fahriani M, Sitorus E. Hubungan Sikap Ibu Bersalin Dan Dukungan Keluarga Dengan Pemilihan Penolong Persalinan di Wilayah Kerja Puskesmas Nibung Kabupaten Musi Rawas Utara. An-Nadaa: Jurnal Kesehatan Masyarakat. 2020;6(1).
- Adriana N, Wulandari LPL, Duarsa DP, Adriana N, Wulandari LPL, Duarsa DP. Akses pelayanan kesehatan berhubungan dengan pemanfaatan fasilitas persalinan yang memadai di Puskesmas Kawangu. Public Health and Preventive Medicine Archive. 2014;2(2):175–80.
- Kusnan A, Rangki L. Faktor determinan proksi kejadian kematian neonatus di wilayah kerja Dinas Kesehatan Kabupaten Buton Utara. Berita Kedokteran Masyarakat. 2019;35(4):131–8.
- Lokan PDS. Profil Kesehatan Desa Sungai Lokan. 2018.
- Aryani Y, Islaeni I. Hubungan Dukungan Suami dan Budaya Dengan Pemilihan Tempat Persalinan. SEAJOM: The Southeast Asia Journal of Midwifery. 2018;4(1):8–14.
- Dantas JAR, Singh D, Lample M. Factors affecting utilization of health facilities for labour and childbirth: a case study from rural Uganda. BMC Pregnancy and Childbirth [Internet]. 2020;20(1):39. Available from: https://doi.org/10.1186/s12884-019-2674-z
- Nurhapipa N, Seprina Z. Factors Affecting in Choosing the Birth Mother in Health Care Delivery XIII Koto Kampar I. Jurnal Kesehatan Komunitas. 2015;2(6):283–8.
- Kawakatsu Y, Sugishita T, Oruenjo K, Wakhule S, Kibosia K, Were E, et al. Determinants of health facility utilization for childbirth in rural western Kenya: cross-sectional study. BMC pregnancy and childbirth. 2014;14(1):1–10.
DETERMINANTS OF BREASTFEEDING EXCLUSIVE IN THE WORKING AREA OF RUMBIA HEALTH CENTER, BOMBANA REGENCY: A CROSS SECTIONAL STUDY
Asnidawati1, Wa Ode Salma2*, Adius Kusnan3
- Public Health of Faculty, Haluoleo University, Kendari, Indonesia
- Nutrition department, Public Health of Faculty, Haluoleo University, Kendari, Indonesia
- Nursing department, Medical of Faculty, Haluoleo University, Kendari, Indonesia
* Corresponding Author: Wa Ode Salma, waode.salma@uho.ac.id, Nutrition department, Public Health of Faculty, Haluoleo University, Kendari, Indonesia
Cita questo articolo
ABSTRACT
Background: Breast’s milk is an excellent food for the growth and development of infants. The United Nations Children's Funds (UNICEF) and the World Health Organization (WHO) recommend that children only be exclusively breastfed for six months and continued until two years. This study analyzes the effect of family support, health workers, and socio-culture on exclusive breastfeeding in the working area of the Rumbia Health Center, Rumbia District, Bombana Regency.
Methods: This study involved 86 mothers who had babies aged 0-6 months who were registered and domiciled in the working area of the Rumbia Health Center spread over 4 Kelurahan and 1 Village, which were selected by purposive sampling using a cross-sectional design from February to April 2021. Data analysis using odds ratio (OR) and logistic regression at significance level < 0.05.
Results: The largest age group in the range of 20-35 years, as many as 68 people (79.1%), undergraduate as many as 32 people (37.2%), and income above Rp. 2.552.014, - / month as many as 60 people (69.8%). The results showed an effect of family support on exclusive breastfeeding (p = 0.002<0.05). There is no influence of socio-cultural factors on exclusive breastfeeding (p = 0.282>0.05) and the results of multivariate analysis of the most dominant variables associated with exclusive breastfeeding in the working area of Rumbia Health Center District Rumbia Bombana Regency is supported by health workers with an OR = 9.199 (p-value = 0.039<0.05).
Conclusions: This study concludes that the support of health workers plays a very important role in exclusive breastfeeding to infants aged six months, which can impact improving the health of toddlers.
Keywords: Determinant, breastfeeding exclusive, toddler, mother
INTRODUCTION
Breast milk is an ideal food for infant growth and development [1,2]. The United Nations Children's Funds (UNICEF) and the World Health Organization (WHO) recommend that children be breastfed exclusively for six months and continued until two years. Global research reports in 2018 showed that the rate of exclusive breastfeeding was quite low, only 41 percent [3]. Meanwhile, in Indonesia, data from the Basic Health Research (RISKESDAS) in 2018 showed that the rate of exclusive breastfeeding was only 37 percent [4]. It is known that the rate of exclusive breastfeeding is still low globally, and it is possible that in Indonesia, the coverage rate of exclusive breastfeeding is below 37% due to the consequences of the Covid-19 pandemic [5].
The study results in 19 developing countries show that socio-cultural factors such as maternal beliefs and other people are significantly strong barriers to exclusive breastfeeding [6–8]. Another study reported that in general, mothers know about breastfeeding, and the majority of respondents (97.3%) had breastfed their babies, 56.5% of them started within one hour after delivery, and 74.1% only gave exclusive breastfeeding until a mean age of 4 months and 30.7% had bottle-fed [9].
The importance of appropriate breastfeeding practices for the healthy growth and development of infants and children has been presented in various policy documents, and guidelines have been set on how to practice exclusive breastfeeding [10]. Social support is widely recognized as influencing the practice of breastfeeding exclusively for six months and continuing to breastfeed for at least two years [11,12]. In addition, health care worker supporting interventions have been shown to increase the rate of exclusive breastfeeding in many developing countries [13,14].
The coverage of achieving exclusive breastfeeding in 2017 in Southeast Sulawesi province for infants 0-6 months was 55.56%, and the coverage of achieving exclusive breastfeeding in 2018 increased by 72%. Although it increased from the previous year, it was not significant and still far from the national target (80%) and the target for Southeast Sulawesi Province (85%). Fluctuating achievements indicate that the exclusive breastfeeding improvement program is not standardized by related technical programs [15]. The working area of the Rumbia Health Center is 40.74%. It is still far from the target set, 50% [16].
The coverage of exclusive breastfeeding in the working area of the Rumbia Health Center has continued to decline over the last three years. It is known that the results of data observations at the Rumbia Health Center showed that data related to mothers who brought their babies to come to the Posyandu in March 2020 recorded only 63 babies and 14 babies who received exclusive breastfeeding while 49 babies were not exclusive. Still far from the expected target of 108 infants (aged 0-6 months). It means that only about 22% of babies get exclusive breastfeeding, and 78% of babies do not get exclusive breastfeeding.
The outbreak of the covid-19 virus has greatly impacted health services, especially Posyandu services in the working area of the Bombana district office, since it was announced that there were residents in Bombana Regency who were confirmed on Covid-19. Overall, Posyandu services at the Rumbia Health Center and other health centers in Bombana Regency are no longer organize the Integrated health service from April to May 2020; therefore, services, data collection, and counseling related to exclusive breastfeeding are not well controlled.
Based on the available scientific data and evidence, this research was conducted to find out how to the influence of family support, health workers, and socio-culture on exclusive breastfeeding in the working area of the Bombana District Health Office, especially at the Rumbia Health Center.
METHODS
Study design
This type of research is analytic observational using a cross sectional design with a purposive sampling technique, so that each participant in this study was selected based on the researcher's considerations.
Participants Sampling
This study involved 86 mothers who had babies aged 0-6 months who were registered and domiciled in the working area of the Rumbia Health Center spread over 4 Kelurahan and 1 Village
Procedure Inclusion and exclusion criteria
To control the quality of research data, the researchers conducted an initial screening by setting sample criteria. The sample inclusion criteria were mothers who had babies aged 0-6 months, mothers who did not experience psychosomatic disorders, while babies who were sick during the study and were born with low birth weight were excluded from the study.
Instruments
In this study involved 3 variables, namely family support, Healthcare worker support and Social-Culture. All variables in this study were measured using a questionnaire which was prepared by the researcher himself by taking into account relevant reference sources [17–19] and had been tested and declared valid and reliable.
Statistical Analysis
Data are presented as numbers and percentages for categorical variables. Continuous data are expressed as the mean ± standard deviation (SD), or median with Interquartile Range (IQR). Data analysis in this study used the Odds Ratio (OR) test to determine the factors associated with breastfeeding exclusivity and multivariate analysis used logistic regression to determine the determinants of breastfeeding exclusivity. The results of the p-value will be the basis for the independent variables to be included in the logistic regression test if p < 0.30, while the dependent variable in the study was the provision of Breastfeeding Exclusive, which was measured using a questionnaire. All tests with p-value (p) < 0.05 were considered significant. Statistical analysis was performed using SPSS app version 16.0.
Ethical consideration
All participants in this study have signed a letter of willingness to participate in the study. No economic incentives were offered or provided for participation in this study. The study was performed in accordance with the ethical considerations of the Helsinki Declaration. This research has been approved by the Haluoleo University Health Research Ethics Commission numbered: 21/KEPK-IAKMI/III/2021.
RESULTS
In the results of this study, the characteristics of the mother, distribution of research variables, results of bivariate and multivariate analysis are presented. The distribution of respondents' characteristics can be seen in the following Table 1:
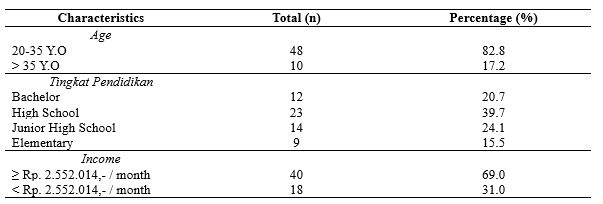
Table 1. Distribution of Respondents’ characteristics
Table 1 informs the largest age group in the range of 20-35 years, as many as 48 people (82.8%), high school as many as 23 people (39.7%), and income above Rp. 2.552.014, - / month as many as 40 people (69.0%).
Table 2 shows the distribution of the dominant study variables consisting of 50 people (58.1%) receiving family support, 67 mothers who received support from health workers (77.9%), and 79 mothers with good socio-culture. (91.9%). There is an effect of family support (p=0.002) and Healthcare worker support (p=0.004) on exclusive breast-feed. There is no influence of socio-cultural factors on the exclusive breastfeeding (p = 0.282).
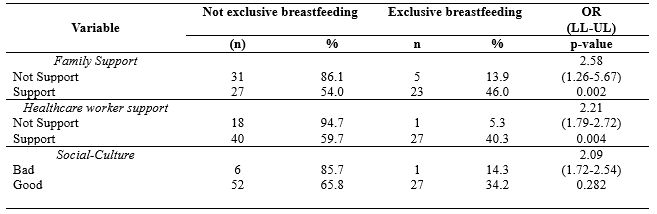
Table 2. Distribution of Study variable
Table 3 shows that after all independent variables were analyzed multivariate with logistic regression, the results obtained that the support of health workers had the greatest OR, namely 4.350 at 95% Cl with a lower limit value of 1.114 and an upper limit value of 75.974 because the confidence interval range was not. Including a value of 1 means that health workers support exclusive breastfeeding in the Work Area of the Rumbia Health Center, Rumbia District, Bombana Regency.
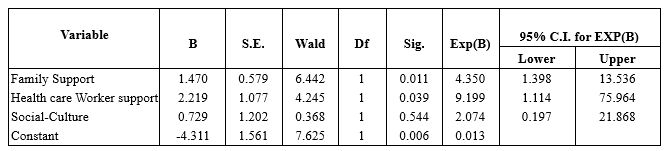
Table 3. Multivariate Analysis
DISCUSSION
- The Effect of Family Support on Exclusive Breastfeeding
The study results found that there was an effect of family support on exclusive breastfeeding in the working area of the Rumbia Health Center, Rumbia District, Bombana Regency. The results of this study are supported by several previous studies that state that exclusive breastfeeding success is closely related to family support, especially husbands and grandmothers of toddlers [20–22].
A mother needs support from the family in providing exclusive breastfeeding; support from the family will affect the mother's decision to give exclusive breastfeeding [23]. The success in providing exclusive breastfeeding by mothers is very dependent on the environment, one of which is the husband or family. If mothers get support from the surrounding environment, mothers can comfortably provide exclusive breastfeeding and take care of their children while working at home. Support or support from other people or closest people, both family support and support from health workers, is very important in the success or failure of breastfeeding [24]. The greater support to continue breastfeeding, it makes the greater the ability to continue breastfeeding. Husband and family support is very influential; a mother who lacks her husband, mother, sister, or even being scared, is influenced to switch to formula milk [25].
The success factor of exclusive breastfeeding, in addition to knowledge, to be cleared, is accompanied by the mother's own will. The role of health workers is very influential on the mother in the process of exclusive breastfeeding. The success of exclusive breastfeeding cannot be separated from family support because the family is the closest person who can encourage mothers to continue giving exclusive breastfeeding and the surrounding culture that encourages exclusive breastfeeding [26].
Family, apart from being a supporting factor, is also as retarder factor. The mother's desire to give exclusive breastfeeding should have been discussed with the family, especially people who will live with the mother when the baby is born, for example, husband, mother, mother-in-law long before the baby is born or at least during the pregnancy phase [27]. In still to families regarding the importance of breastfeeding, how to give exclusive breastfeeding and what support they can provide. It is important, because in some cases, a mother's failure to provide exclusive breastfeeding is precisely because of a misunderstanding from the family, for example, being given water, so the baby does not turn yellow, or adding a baby with formula milk because the baby cries and thinks the baby is still hungry and hungry. At that time, the baby's mother had difficulty refusing or resisting because the one who gave it was the mother-in-law and her biological mother. This event will be minimized when the mother and family have good breastfeeding knowledge and a strong agreement and commitment to supporting mothers in exclusive breastfeeding.
- The Effect of Health Worker Support on Exclusive Breastfeeding
The study results found that there was an effect of the support of health workers on exclusive breastfeeding in the working area of the Rumbia Health Center, Rumbia District, Bombana Regency. Furthermore, the results of the multivariate analysis of this study found that the most dominant variable influencing exclusive breastfeeding in the working area of the Rumbia Health Center, Rumbia District, Bombana Regency, was the support of health workers with an OR value of 9.633.
According to the theory, the support of officers is very helpful, where the support of officers has a big influence on exclusive breastfeeding [22]. A health worker is responsible for health workers who provide health services to individuals, families, and communities. If health workers actively socialize with the community, they can change traditions or habits that can slowly harm health, such as providing complementary foods to infants before six months [28]. Thus, the public will know and understand more about traditional practices that can be detrimental to health so that they will change their behavior and mindset towards what they know from the health worker [29]. The encouragement of health workers can influence respondents to have a high intention of giving exclusive breastfeeding to their babies. The success of breastfeeding mothers requires health workers, especially perinatal service workers such as midwives who are trained and understand the ins and outs of the breastfeeding process. They are the first to help mothers give birth to give breast milk to babies. The role of health workers is the beginning of the mother's success or failure in exclusive breastfeeding. Knowledge, attitudes, and actions of health workers such as midwives are the determinants of the readiness of officers in managing breastfeeding mothers with lactation management (lactation management) so that the implementation of exclusive breastfeeding increases.
This study is in line with previous studies concluding that there is a relationship between the support of health workers and exclusive breastfeeding (p-value = 0.0001) with a PR of 2.48, meaning that mothers who receive support from midwives have a 2.48 times greater chance of breastfeeding independently—exclusively compared to mothers who received less support from the midwife [28]. Furthermore, in line with other research in South Tomohon, it shows a relationship between the support of health workers in exclusive breastfeeding for six months in the Pangolombian Community Health Center, South Tomohon District, p-value = 0.008 [30].
- The Influence of Socio-Cultural Factors on Exclusive Breastfeeding
The results showed no influence of socio-cultural factors on exclusive breastfeeding in the working area of the Rumbia Health Center, Rumbia District, Bombana Regency. Breastfeeding cannot be separated from the cultural order. Every breastfeeding from mother to child will be related to the social culture that exists in the community. Behavior is formed by habits that are colored by social culture. Everyone is always exposed and touched by environmental habits and is influenced by the community, either directly or indirectly. Behavior that habits and beliefs have shaped about exclusive breastfeeding will impact the mother's desire to give exclusive breastfeeding to children. This socio-cultural will affect the success of exclusive breastfeeding; respondents who have good socio-cultural categories will show success in exclusive breastfeeding. The good social culture indicates it in providing exclusive breastfeeding, as many as 27 people (34.2%) and those who do not give exclusive breastfeeding, as many as 52 people (65.8%) while out of 7 respondents with poor socio-culture giving exclusive breastfeeding, one person (14.3%) and who did not give exclusive breastfeeding were six people (85.7%). The beliefs and traditions that exist in the community lead to the community's mindset on the actions taken to respond to something. Beliefs that exist in society are very important in shaping a person's behavior.
A study conducted [31] in Athens, Greece, found that the breastfeeding process is often not determined by biological factors but is mainly based on habits, traditions, and behaviors in society. Tradition is a social behavior where the behavior is passed down from generation to generation by going through socialization. A tradition determines the values and morals of society because tradition contains rules according to the community about what should be done.
Habits are carried out from generation to generation and carried out by the community, the judge, and assumes that it is the most correct and good thing [32]. The mother's beliefs and desires to imitate the mother's intention to breastfeed her baby. The respondent's intention to do exclusive breastfeeding is influenced by the mother's own beliefs and beliefs [33]. Logically, the existence of a tradition in Rumbia District regarding breastfeeding is closely related to the mother's intentions and expectations regarding exclusive breastfeeding success. Traditions and beliefs develop a pattern to lead people's behavior to do things under the traditions and beliefs that exist in their environment, such as colostrum contained in breast milk are not good and dangerous for babies, special teas or liquids are needed by babies before breastfeeding, and babies will experience a lack of nutrients for growth if only given breast milk [34].
Unfulfilled breast milk needs will cause malnutrition in children—some dietary restrictions at certain times and certain types of food that should not be eaten while breastfeeding. The lack of knowledge of mothers about nutrition and their beliefs causes nutritional problems for their children and impacts the body's defense against infection and delays in growth and development [35]. Interventions promoting behavior change should focus on dispelling less than optimal beliefs and practices into beliefs to build positive breastfeeding practices, involving family support (partners and other family members) as they are an important source of information about breastfeeding [36,37]. Changing people's habits and beliefs is not an easy task, so the role of health workers is very much needed to carry out activities to increase exclusive breastfeeding programs. Guidelines for increasing exclusive breastfeeding programs cannot be separated from the reproductive process of mothers after giving birth, which is expected to change the behavior of people who initially do not believe in the benefits and benefits of breastfeeding to believe and slowly leave the culture and tradition of giving additional food to infants aged 0-6 months. which can interfere with health [38].
The development of community and religious leaders is an important strategy for the health workforce because people tend to obey the directions of trusted people around their environment than people outside their environment. Community empowerment about the importance of exclusive breastfeeding for babies is known by all levels of society, which is expected to provide support and motivation for breastfeeding mothers and can automatically improve reproductive health.
CONCLUSIONS
The success of the Breastfeeding exclusive program is strongly influenced by various factors such as family support such as husbands and grandmothers of toddlers, as well as support from health workers through promotional programs when mothers of toddlers visit health care facilities, as well as socio-cultural factors that are believed by the family such as the existence of dietary restrictions for babies of a certain age, babies born must be given sweet food immediately, at a certain age babies must be given food in traditional events.
This study suggests the importance of the role of health workers in providing a good understanding to families about the benefits of exclusive breastfeeding until the baby is 6 months old.
Limitations study's
In this study, there are limitations such as the presence of some areas that cannot be reached by the research team so they cannot participate in the study. Then in this study using a cross-sectional design so that the information obtained by researchers is only limited to data when the research is conducted.
Clinical implications of research
The results of this study can be the basis for health workers in maximizing the role of the family in supporting mothers to provide exclusive breastfeeding to infants and paying attention to the socio-cultural background of the family, especially mothers in providing interventions in the field, especially regarding exclusive breastfeeding.
ACKNOWLEDGEMENT
We would like to express our gratitude to several parties who have provided support for our research. To the chief of the Poltekkes Jambi in her support in providing suggestions and input for the development of this research, and to mothers who have actively participated as respondents in this research.
FUNDING STATEMENT
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
CONFLICT OF INTEREST
The author(s) declares no conflict of interest.
REFERENCES
- Meier PP, Patel AL, Bigger HR, Rossman B, Engstrom JL. Supporting breastfeeding in the neonatal intensive care unit: Rush Mother’s Milk Club as a case study of evidence-based care. Pediatric Clinics. 2013;60(1):209–26.
- Piemontese P, Liotto N, Mallardi D, Roggero P, Puricelli V, Giannì ML, et al. The effect of human milk on modulating the quality of growth in preterm infants. Frontiers in pediatrics. 2018;6:291.
- Osibogun OO, Olufunlayo TF, Oyibo SO. Knowledge, attitude and support for exclusive breastfeeding among bankers in Mainland Local Government in Lagos State, Nigeria. International breastfeeding journal. 2018;13(1):1–7.
- Kementerian Kesehatan. Profil Kesehatan Indonesia. Jakarta: Depkes RI; 2018.
- Unicef. Breastfeeding: a mother’s gift, for every child. Unicef; 2018.
- Balogun OO, Dagvadorj A, Anigo KM, Ota E, Sasaki S. Factors influencing breastfeeding exclusivity during the first 6 months of life in developing countries: a quantitative and qualitative systematic review. Maternal & child nutrition. 2015;11(4):433–51.
- Nsiah-Asamoah C, Doku DT, Agblorti S. Mothers’ and Grandmothers’ misconceptions and socio-cultural factors as barriers to exclusive breastfeeding: A qualitative study involving Health Workers in two rural districts of Ghana. PloS one. 2020;15(9):e0239278.
- Henry BA, Nicolau AIO, Américo CF, Ximenes LB, Bernheim RG, Oriá MOB. Socio-Cultural factors influencing breastfeeding practices among low-income women in Fortaleza-Ceará-Brazil: a Leininger’s Sunrise Model Perspective. Enfermería Global. 2010;19:1–13.
- Akinyinka MR, Olatona FA, Oluwole EO. Breastfeeding knowledge and practices among mothers of children under 2 years of age living in a military barrack in Southwest Nigeria. International Journal of MCH and AIDS. 2016;5(1):1.
- Tampah-Naah AM, Kumi-Kyereme A, Amo-Adjei J. Maternal challenges of exclusive breastfeeding and complementary feeding in Ghana. PloS one. 2019;14(5):e0215285.
- Laugen CM, Islam N, Janssen PA. Social support and exclusive breast feeding among Canadian women. Paediatric and perinatal epidemiology. 2016;30(5):430–8.
- Casal CS, Lei A, Young SL, Tuthill EL. A critical review of instruments measuring breastfeeding attitudes, knowledge, and social support. Journal of Human Lactation. 2017;33(1):21–47.
- Boateng M. Knowledge, attitude and practice of exclusive breastfeeding among mothers in Techiman, Ghana. Itä-Suomen yliopisto; 2018.
- Imdad A, Yakoob MY, Bhutta ZA. Effect of breastfeeding promotion interventions on breastfeeding rates, with special focus on developing countries. BMC public health. 2011;11(3):1–8.
- Dinkes Propinsi Sultra. Profil Kesehatan Propinsi Sulawesi Tenggara 2019. Kendari: Bidang Data dan Informasi; 2019.
- Dinkes Kabupaten Bombana. Profil Kesehatan. Rumbia: Bidang Data dan Informasi Kab/Bombana; 2019.
- Ramadani M. Dukungan keluarga sebagai faktor dominan keberhasilan menyusui eksklusif. Media Kesehatan Masyarakat Indonesia. 2017;13(1):34–41.
- Sitohang FD, Kahar IA, Sirait A. Faktor yang Berhubungan dengan Pemberian Asi Eksklusif pada Bayi Usia 6-12 Bulan di Wilayah Kerja Puskesmas Sigalingging Kabupaten Dairi Tahun 2017. Jurnal Ilmiah Keperawatan Imelda. 2019;5(1):568–78.
- Fajar NA, Purnama DH, Destriatania S, Ningsih N. Hubungan Pemberian ASI Eksklusif dalam Prespektif Sosial Budaya di Kota Palembang. JOURNAL-JIKM: JURNAL ILMU KESEHATAN MASYARAKAT. 2018;9(3):226–34.
- Nuzulia F. Hubungan antara dukungan keluarga dengan pemberian ASI eksklusif pada bayi di Desa Bebengan Kecamatan Boja Kabupaten Kendal. Jurnal Keperawatan Maternitas. 2013;1(1).
- Ratnasari D, Paramashanti BA, Hadi H, Yugistyowati A, Astiti D, Nurhayati E. Family support and exclusive breastfeeding among Yogyakarta mothers in employment. Asia Pacific journal of clinical nutrition. 2017;26(Supplement):S31.
- Kusumayanti N, Nindya TS. Hubungan dukungan suami dengan pemberian asi eksklusif di daerah perdesaan. Media Gizi Indonesia. 2017;12(2):98–106.
- Ku C, Chow SKY. Factors influencing the practice of exclusive breastfeeding among Hong Kong Chinese women: a questionnaire survey. Journal of clinical nursing. 2010;19(17‐18):2434–45.
- La Aga, Erwin AL. Cakupan dan Determinan Pemberian ASI Eksklusif di Pemukiman Kumuh Dalam Perkotaan di Kecamatan Tallo Kota Makassar. Majalah Kesehatan FKUB. 2019;6(1):44–55.
- Novena K. Hubungan Dukungan Keluarga terhadap Keberhasilan ASI Eksklusif pada Bayi Usia 0-6 Bulan di BPM Nihayatur Rokhmah Kuningan Kabupaten Blitar. STIKes Patria Husada Blitar; 2019.
- Hety DS, Susanti IY, Adiesti F, Muhith A. Maternal Knowledge, Husband’s Support, Cultural Support and Role of Health Workers in the Exclusive Breastfeeding Program at Mojosari Health Center. In: Proceedings of the Third International Seminar on Recent Language, Literature, and Local Culture Studies. Proceedings Series Journals Search EAI; 2020.
- Deslima N, Misnaniarti M, Zulkarnain HM. Analisis Hubungan Inisisi Menyusu Dini (IMD) Terhadap Pemberian ASI Eksklusif di Wilayah Kerja Puskesmas Makrayu Kota Palembang. JUMANTIK (Jurnal Ilmiah Penelitian Kesehatan). 2019;4(1):1–14.
- Zuhrotunida. Hubungan Dukungan Tenaga Kesehatan Dengan Keberhasilan ASI Eksklusif di Puskesmas Kutabumi. IMJ (Indonesian Midwifery Journal). 2018;1(2).
- Mi’rad KA, Agushybana F, Margawati A. Study of Madurese Perception and Behavior towards Maternal Health in Jember Regency. International Journal of Multicultural and Multireligious Understanding. 2020;7(3):273–82.
- Anita, Wantania J, Korompis M. Hubungan Antara Pengetahuan Ibu, Fasilitas Pelayanan Kesehatan, Dukungan Keluarga Dan Dukungan Petugas Dengan Pemberian Asi Ekslusif 6 Bulan Di Wilayah Kerja Puskesmas Pangolombian Kecamatan Tomohon Selatan. Paradigma. 2016;4(2).
- Daglas M, Antoniou E. Cultural Views and Practices Related to Breastfeeding. Health science journal. 2012;6(2):353.
- Kusnan A, Binekada IMC, Usman AN. The proxy determinant of complementary feeding of the breastfed child delivery in less than 6 months old infant in the fishing community of Buton tribe. Enfermeria clinica. 2020;30:544–7.
- Yusrina A, Devy SR. Faktor Yang Mempengaruhi Niat Ibu Memberikan ASI Eksklusif di Kelurahan Magersari, Sidoarjo. Jurnal Promkes: The Indonesian Journal of Health Promotion and Health Education. 2016;4(1):11–21.
- Hatta GR. Pedoman Manajemen Informasi Kesehatan di sarana pelayanan kesehatan. Jakarta: Universitas Indonesia. 2008.
- Salma WO, Suhadi LOMS, Irma A, Karo M. Rendahnya Pemberian ASI Eksklusif Pada Anak Etnik Pesisir Berhubungan dengan Kejadian Penyakit Tropis. Penguatan dan Inovasi Pelayanan Kesehatan. 2019;87.
- Wanjohi M, Griffiths P, Wekesah F, Muriuki P, Muhia N, Musoke RN, et al. Sociocultural factors influencing breastfeeding practices in two slums in Nairobi, Kenya. International breastfeeding journal. 2016;12(1):1–8.
- Joseph FI, Earland J. A qualitative exploration of the sociocultural determinants of exclusive breastfeeding practices among rural mothers, North West Nigeria. International breastfeeding journal. 2019;14(1):1–11.
- Batubara NS. Pengaruh Sosial Budaya Terhadap Pemberian ASI Eksklusif di Wilayah Kerja Puskesmas Batunadua Kota Padangsidimpuan Tahun 2015. Jurnal Kesehatan Ilmiah Indonesia (Indonesian Health Scientific Journal). 2016;1(1):59–66.
Occupational Health and Safety for Nurses: Literature Review
Antonio Brusini.1
- Nurse in Sports Medicine, AUSL Modena, Alma Mater Studiorum university tutor, Bologna
Corresponding author: Brusini A., nurse in Sports Medicine at AUSL Modena, master's degree in "Management of Sport and Motor Activities". Email: antoniobrusini87@outlook.it
Cita questo articolo
ABSTRACT
Introduction: The prevention of occupational accidents in the sphere of occupational health and safety is an important issue in the Italian work setting; health workers, and especially nurses, are continually exposed to the risk of work-related accidents, which can affect the quality of care provided.
Aim: The aim of this review is to investigate the nurse's perceived level of preparedness with regard to occupational safety.
Methods: A narrative review of the literature was conducted using some of the main databases such as PubMed, CINAHL and Cochrane.
Results: The studies analysed show that Italian nurses have little knowledge about occupational health and safety legislation.
Conclusions: Establishing specific postgraduate training events and identifying specific legislation for healthcare personnel could represent essential steps towards implementing this specific knowledge.
Keywords: Prevention; Training; Nurses; Healthcare workers
Introduction
Occupational safety has always been a central issue in the Italian working environment [1]: in 2019, 641,638 accidents at work were reported by December 2019 (640,723 in 2018), 100,905 of these took place on the journey between home and workplace (98,446 in 2018) and 540,733 in the workplace (542,277 in 2018), with 1089 fatal accidents at work (1133 in 2018) [2].
A key area for safeguarding workers, including nurses, is training, which is a useful tool for working safely [3]. Indeed, the risk of injury has increased during the COVID-19 pandemic period (131,090 reports of injuries due to COVID-19 infection in the workplace in 2020 [4]). Fewer accidents would lead to reduced expenditure, related to the cost of treatment, lost working days and replacement of the injured worker. In the UK, for example, in the 2011–12 season, there was a quantifiable loss of 10.4 million working days and a consequent reduction in productivity linked to work-related stress injuries.
The specific high-risk topics to be covered during the course include accident risks; general mechanical risks; general electrical risks; machinery; equipment; falls from height; explosion risks; chemical risks; mists, oils, fumes, vapours, dusts; labelling; carcinogenic risks; biological risks; physical risks; noise; vibration; radiation; microclimate and lighting; display screens; PPE; work organisation; working environments; work-related stress; manual handling of loads; handling of goods (lifting equipment, means of transport); signposting; emergencies; safety procedures with reference to the specific risk profile (high in this case); escape and fire procedures; organisational procedures for first aid; accidents and near misses; other risks. Any further training is at the discretion of the employer, who may decide to give his or her staff additional training [6,7].
Objective
The aim of this study is to investigate, through a narrative review of the literature, nurses' knowledge of occupational safety.
Methods
PubMed, CINAHL and Cochrane databases were used as a search medium, and all databases were searched on 28/02/2021 for the set of keywords: 'occupational', 'health', 'safety', 'nurse', without Boolean operators between them. No time limit was given to the research, and only English-language sources were taken into account.
This search yielded 422 results on the Cochrane database (using the 'all text' filter); the same search yielded 2418 results on the Pubmed database and 631 results on CINAHL; of these, 3 articles could not be traced (2 on PubMed and 1 on CINAHL). Only studies that discussed the topic of occupational health and safety training and that had carried out a survey in the form of a questionnaire or other methods on training or nurses' perceptions of training in their workplaces were included. Studies involving an education or training programme for nurses who had carried out a survey of subject knowledge prior to the intervention then performed in the study were also taken into account. The selected studies were carried out on a nursing population or included nurses among other professions in the sample. The outcomes to be studied were the survey responses of the studies on the level of preparedness in the field of occupational safety and, if not reported in quantitative terms, the authors' considerations.
Results
Articles concerning the figure of the 'Occupational Health Nurse/Nursing' were excluded (Table 1), as it is a figure that specifically deals with occupational health and safety but is not present in Italy, as were repeat sources. After reading the title, 22 sources on Cochrane, 515 on PubMed and 80 on CINAHL were retained.
All articles other than primary studies were excluded. After reading the abstract and the article, 10 articles were selected (1 on Cochrane and Pubmed, 5 on Pubmed and CINAHL, 4 on Pubmed only). Duplicate results were skimmed after the results selection. 2 results concern nurses together with other health professionals, 1 result involves nurses and nursing managers.
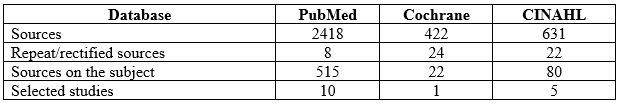
Table 1: Databases consulted, sources found and selected
The detailed procedure used in the selection of articles is presented as a flow chart in Figure 1.

Figure 1. Diagram showing the stages of the review and article selection
Table 2 shows the studies classified by author, year, health personnel involved in the study, method, number of participants and results.
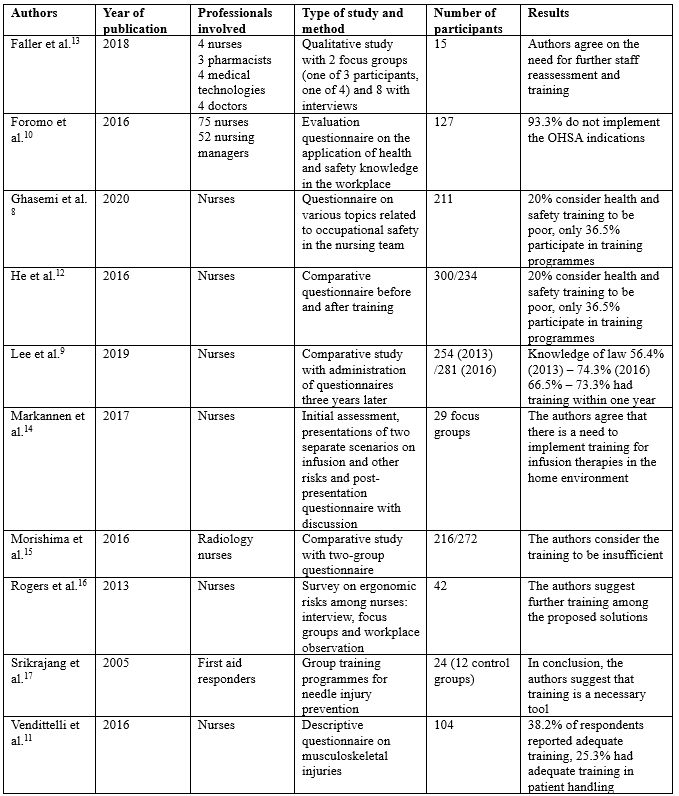
Table 2: Citations on training for nurses and healthcare professionals in the literature found, in alphabetical order by the author. OHSA 'Occupational Health and Safety Act', MAPO Movimentazione Assistita Pazienti Ospedalieri (Assisted Handling of Hospital Patients)
Ghasemi [8] conducted a study surveying 211 nurses by asking questions on various topics related to teamwork safety (nurse relationships, accumulated fatigue, communication with physiatrists, supervisor attitude, nursing unit conditions, error reporting, and nursing training), finding that 20% of respondents considered health and safety training to be poor, and only 36.5% participated in occupational safety training programmes. Lee [9] surveyed knowledge of the law that came out in California in 2012 on patient handling, one year (2013) and three years (2016) later, finding 56.4% of nurses in 2013 and 74.3% of nurses in 2016 were familiar with the current law, with those figures changing to 66.5% and 73.3% respectively for nurses who had received training in patient handling within the past year. Foromo [10] administered an evaluation questionnaire to 75 nurses and 52 'nursing managers' asking whether health and safety regulations were implemented in the workplace and found that 93.3% were not implementing the correct instructions. Vendittelli [11] administered an online questionnaire with scales of 1 to 5 (and the optional possibility to write comments) to 104 nurses who graduated between 2011 and 2014 (offered to 435 in total, with only 104 participating), marking demographics, training (and incidence) in occupational safety, including in mobility procedures, and general nursing training, with only 38.2% stating that they had received adequate training specific to their operating unit, and only 25.3% stating that they had adequate time for training in patient handling. He [12] administered a comparative questionnaire between two groups, before and after a training programme on the topic of HIV/AIDS, and the awareness of HIV/AIDS-related knowledge improved significantly after the training (correct answers increased from 67.9% to 82.34%, on risk perception from 54.4% to 66.6%).
Faller [13] conducted a qualitative study with various healthcare professionals using instruments such as interviews and focus group discussions on some focal points (experience of accidents at work, implementations, barriers and strategies to improve safety), and eight groups with semi-structured interviews, and indicated the genuine need for further training and investigation of staff competences in the field of safety. Markannen [14] worked mainly on prevention in infusion practice, presenting possible working situations in focus groups, with pre- and post-intervention evaluation questionnaires, and agreeing on the need to implement training in home care. Morishima [15] administered a questionnaire to two groups of health professionals, one in 2008 and one in 2010, on the subject of radiation: whether there are different types (24.5% responded positively in 2008 and 40.3% in 2010), about the external protection procedure (17.6% and 26.7% positive responses respectively), the correct distance to the machine (31.5% and 41.5%) and the correct position of the dosimeter (60.8% and 55.1%). Rogers [16] conducted an investigation into the ergonomic risks of the nursing profession through focus groups, interviews and workplace observations of 42 registered nurses in five hospitals in North Carolina, finding training to be one of the main tools in preventing ergonomic risks. Finally, Srikrajang [17] conducted a study on a group of 24 emergency and laboratory health workers (including a control group of 12), demonstrating improvements with the use of training tools in preventing needlestick injuries.
Discussion
The literature review identified few sources, most agreeing that participants in the various studies show structural deficiencies in occupational health and safety training, calling for thorough training interventions. The results show that a significant number of nurses are not familiar with their state's occupational health and safety legislation, and there are many nurses who are not familiar with risk factors and how to work as safely as possible. In fact, the pandemic period, as pointed out by Giorgi [18], highlighted a particular situation for care staff with consequent stress due both to the working conditions resulting from a higher-than-normal workload due to the emergency both in terms of working hours and in terms of working conditions (overload of patients and the continuous use of personal protective equipment (PPE) to which they were not accustomed, except in very few departments, greater emotional involvement) and to the condition that in some settings was already present before the pandemic. Moreover, there is continuous exposure to biological risk due to possible contagion between patient and operator and between operators, no longer represented almost exclusively by contact with biological liquids, although as shown by Maida [19], there is still a need for training also in this type of risk. The COVID-19 pandemic, therefore, exaggerated the possibility of an accident at work, without any clear preparation for the event. The lack of training on the correct handling of the equipment, and the impossibility of training during the lockdown period, led to a substantial change in the training offer in the field of occupational health and safety, with an increase in online portals. The example of FadinMed (https://www.fadinmed.it/) was necessary, as it offered courses, together with the Ministry's portals, useful for training on the use of PPE during a pandemic.
A possible improvement in an Italian perspective for nurses would be the conferral of the management of training topics on occupational health and safety by the professional order (for each health category, it is compulsory to be registered; nurses must be registered with the Professional Order of Nurses, FNOPI): in the case of nurses, it could also give indications based on the work task (therefore, after a risk assessment per department and per health figure). To give a practical example, a nurse who has a higher rate of patient handling (with a high MAPO index, a rating scale for patient handling risk, above 1.51), must be trained to do so as safely as possible, and not at the discretion of the employer, but as a matter of obligation (although indications with MAPO indexes above 1.51 and especially 5 strongly recommend further training) [20].
It must also be said that the FNOPI already has a programme of courses (including in occupational health and safety training under COVID-19). However, if the use of CME has been made compulsory (the training credits for post-basic training, a quota of 150 for the three-year period, and at least 25 per year), the topics and courses to be followed still remain the choice of the professional. Therefore, a differentiation of the type of courses to be carried out in addition to the statutory ones would be necessary according to the task and location of work (Kim [21] in his study investigated 1672 nurses of childbearing age on the subject of radiation risks and found that 50.3% had not received training, and only 25.1% had received it regularly), to be included in the category of CME, and more control in the private sector. In addition, it would be appropriate to standardise the subjects of biohazard and clinical risk (and the use of PPE), given the current pandemic situation, and to organise refresher training more frequently. Also, at university level, well before the career stage, there should be a greater emphasis worldwide on occupational safety [22,23], following the American example as shown by Whitaker [24], where occupational safety and health courses are taught in more than 80% of American universities and nursing schools.
Finally, it is also necessary to run courses that encourage healthcare personnel to implement healthy lifestyles and proper management of work-related stress: sport and a positive approach to leisure time, which can be combined with family life, can help to properly manage work-related stress and reduce the risk of burnout [25]. This article explores an important open question, that of the safety of the worker (in this case, the nurse), his or her level of preparedness, and how we can work to improve it. This is an issue that is not given much consideration in Italy, and in the future, it is hoped that more studies will be carried out in this regard.
Conclusions
It is necessary to evaluate the occupational health and safety system for nurses and in universities, in order to have better-prepared professionals in the world of work in the health sector, by implementing training systems and creating a continuous survey of nurses' knowledge, by frequently administering tools such as questionnaires and other evaluation systems, thereby inviting nurses to continue studying the topic after their basic training. In addition, the training system must also be consolidated at the university level, which is the true starting point of a nurse's career. It is extremely important to consider that, along with training, work should also be undertaken on non-individual measures to reduce accidents (continuous research into collective protection systems and a continuous supply of increasingly high-quality PPE are examples of this), and more responsibility should be given to Prevention and Protection Service Managers, supervisors and nursing coordinators, for example, and greater collaboration with universities, with an annual update of the Nursing Guidelines and Procedures, and to work on an individual level on considerations that improve the quality of work and life outside the healthcare working environment, inviting companies to take an interest in the personal situation of employees and to help them to fulfil the concept of health as defined by the WHO in 1948 ("a state of complete physical, mental and social well-being"). In addition, there is a need for improved mechanisms in university curricula and postgraduate training (in terms of frequency and content).
Limitations of the Study
The limitations of the study are represented by the selection of considerably diverse samples: the possibility of researching any studies of a national nature, which are not currently present in the international literature, would have focused the research by giving a more precise overview of our country, together with the use of other databases and with the aid of grey literature. The data may be subject to bias as it does not include feedback from institutional channels, and is based on data in databases from doctors and health professionals in different countries. ISTAT data may be out of date and obsolete, in addition to the difficulty in distinguishing between accidents in the different health sectors.
Funding statement
This research did not receive any form of funding.
Conflicts of Interest
The author declares that he/she has no conflicts of interest associated with this study.
REFERENCES
- Ruggiero N, Magna B, Cornaggia N, Rosa AM, Ferrero O, et al., Effectiveness of Health and Safety at Work Services (PSAL) in reducing occupational injuries in Lombardy Region, Med Lav. 2018 Feb 20;109(2):110-124 DOI:23749/mdl.v109i2.6472
- ISTAT data, URL:https://dati.inail.it/opendata/default/Qualidati/index.html
- Gagliardi D, Marinaccio A, Valenti A, Iavicoli S, Occupational safety and health in Europe: lessons from the past, challenges and opportunities for the future, Ind Health. 2012;50(1):7-11
- INAIL, Coronavirus emergency, 131,000 work-related infections reported to INAIL, Report, 22/01/2021, URL:https://www.inail.it/cs/internet/comunicazione/news-ed-eventi/news/news-denunce-contagi-covid-31-dicembre-2020.html
- European Agency for Safety & Health at Work EU-OHSA, Calculating the cost of work-related stress and psychosocial risks in the workplace – Literature overview), 2014, doi:10.2802/20493
- Legislative Decree no. 81 of 9 April 2008, 'Consolidated Act on Occupational Health and Safety", Implementation of Article 1 of Law no. 123 of 3 August 2007 on the protection of health and safety in the workplace, (published in the Official Gazette no. 101 of 30 April 2008 – Suppl. Ordinary Supplement no. 108)
- Permanent Conference for relations between the State, the Regions and the Autonomous Provinces of Trento and Bolzano, 21 December 2011, Agreement between the Minister of Labour and Social Policy, the Minister of Health, the Regions and the Autonomous Provinces of Trento and Bolzano for worker training, pursuant to Article 37, paragraph 2, of Legislative Decree 9 April 2008, no. 81 (published in the Official Gazette General Series no. 8 of 11/02/2012)
- Ghasemi F, Aghaei H, Askaripoor T, Ghamari F, Analysis of occupational accidents among nurses working in hospitals based on safety climate and safety performance: a Bayesian network analysis, Int J Occup Saf Ergon. 2020 Jul 14;1-7
- Lee S-J, Lee JH, Harrison R, Impact of California's safe patient handling legislation on musculoskeletal injury prevention among nurses, Am J Ind Med. 2019 Jan;62(1):50-58
- Foromo MR, Chabeli M, Satekge MM, Survey on the implementation of the Occupational Health and Safety Act at an academic hospital in Johannesburg, Curationis. 2016 Sep 28;39(1):e1-e10
- Vendittelli D, Penprase B, Pittiglio L, Musculoskeletal Injury Prevention for New Nurses, Workplace Health Saf. 2016 Dec;64(12):573-585
- He L, Lu Z, Huang J, Zhou Y, Huang J, et al., An Integrated Intervention for Increasing Clinical Nurses' Knowledge of HIV/AIDS-Related Occupational Safety, Int J Environ Res Public Health. 2016 Nov 7;13(11):1094
- Faller EM, Miskam NB, Pereira A, Exploratory Study on Occupational Health Hazards among Health Care Workers in the Philippines, Ann Glob Health. 2018 Aug 31;84(3):338-341
- Markkanen P, Galligan C, Quinn M, Safety Risks Among Home Infusion Nurses and Other Home Health Care Providers, J Infus Nurs. Jul/Aug 2017;40(4):215-223
- Morashima Y, Chida K, Katahira Y, Seto H, Chiba H, Tabayashi K, Need for radiation safety education for interventional cardiology staff, especially nurses, Acta Cardiol. 2016 Apr;71(2):151-5
- Rogers B, Buckheit K, Ostendorf J, Ergonomics and nursing in hospital environments, Workplace Health Saf. 2013 Oct;61(10):429-39
- Srikrajang J, Pochamarn C, Chittreecheur J, Apisarnthanarak A, Danchaivijitr S, Effectiveness of education and problem solving work group on nursing practices to prevent needlestick and sharp injury, J Med Assoc Thai. 2005 Dec;88 Suppl 10:S115-9
- Giorgi G, Lecca LI, Alessio F, Finstad GL, Bondanini G, et al., COVID-19-Related Mental Health Effects in the Workplace: A Narrative Review, Int J Environ Res Public Health. 2020 Oct 27;17(21):7857
- Maida CM, Aprea L, Calamusa G, Campisi F, Favaro D, et al., Blood and body fluids exposure of healthcare workers in a university hospital of Palermo, Italy: a fourteen years long surveillance, Ann Ig. 2020 Sep 29;32(6). doi: 10.7416/ai.2020.2380
- Cantarella C, Stucchi G, Menoni O, Cairoli S, Manno R, et al., MAPO Method to Assess the Risk of Patient Manual Handling in Hospital Wards: A Validation Study, Hum Factors. 2020 Nov;62(7):1141-1149
- Kim O, Sun Kim M, Jung Jang H, Lee H, Kang Y, et al., Radiation safety education and compliance with safety procedures-The Korea Nurses' Health Study, J Clin Nurs. 2018 Jul;27(13-14):2650-2660
- McCullagh MC, Berry P, A Safe and Healthful Work Environment: Development and Testing of an Undergraduate Occupational Health Nursing Curriculum, Workplace Health Saf. 2015 Aug;63(8):328-32
- Jahangiri M, Malakoutikhah M, Choobineh A, Zare A, Nurses' uncertainty about medical gloves safety during the COVID-19 pandemic, J Healthc Qual Res. 2021 Apr 27;S2603-6479(21)00037-3. doi: 10.1016/j.jhqr.2021.03.009
- Whitaker S, Wynn P, Williams N, Occupational health teaching for pre registration nursing students, Nurse Educ Today. 2002 Feb;22(2):152-8
- Vitale E, Cesano E, Germini F, Prevalence of Burnout among Italian Nurses: a descriptive study, Acta Biomed. 2020 Sep 7;91(4):e2020117. doi: 10.23750/abm.v91i4.9008
THE EFFECT OF BABY MASSAGE ON THE SLEEP QUALITY OF 3-12 MONTHS BABIES IN PRIVATE MIDWIVE JAMBI CITY
Atika Fadhilah Danaz Nasution, *Nuraidah, Imelda
Department of Midwifery, Health Polytechnic of Jambi, Indonesia
* Corresponding Author: Nuraidah, Department of Midwifery, Health Polytechnic of Jambi, Indonesia. E-mail: nuraidah.poltekkes869@gmail.com
Cita questo articolo
ABSTRACT
Introduction: Sleep needs in infants 3-12 months are not only in terms of quantity but also quality. Good quality sleep provides benefits to the fulfilment of physical and psychological needs. One method of meeting these needs is baby massage. A common reason for mothers to give baby massages is the child's habit of fussing at night and often waking up, and they say that after the massage, their child becomes calm at night. This study aims to analyze the effect of baby massage on the sleep quality of infants aged 3-12 months at private midwife Muji Kenali Asam in Jambi City.
Material and Methods: This pre-experimental study consisted of a one-group pretest-posttest design for a group of 68 infants aged 3-12 months. The questionnaire was compiled into a google form, and the link was distributed to each mother. Data processing consists of editing, coding, tabulating and statistical tests (Wilcoxon test) at the limit of significance value of 0.05.
Results: The study results that can be described are that most of the sleep quality of infants aged 3-12 months before the intervention was sufficient at 45.6%, and for poor quality, it was 27.9%. After the intervention, most infants aged 3-12 months were good in sleep quality by 45.5% and sufficient sleep quality by 52.9%. The results of the Wilcoxon test revealed the effect of infant massage on infant sleep quality with a significance value of p-value = 0.001.
Conclusion: Baby massage tends to improve the baby's sleep quality. Therefore Midwifery students need to acquire baby massage skills and promote the method to mothers, particularly those with babies 3-12 months.
Keywords: Baby Massage, Sleep Quality, Pre Experimental, Infants Aged 3-12 Months
INTRODUCTION
Infancy is a golden period for maximum growth and development of children and needs special attention [1]. Sleep is one of the factors that affect the growth and development of babies because, during sleep, the baby's brain growth reaches its peak and produces three times more growth hormone than when the baby wakes up [2].
As published by the World Health Organization (WHO) in 2012, about 33% of babies have sleep problems. In Melbourne, Australia, found that 32% of mothers reported repeated occurrences of sleep problems in infants [3]. In 2016, Sekartini reported that 80 children aged less than three years, 51.3% of them had sleep disorders [4]. Another study of 385 respondents in Jakarta, Bandung, Medan, Palembang and Batam reported that 44.2% of the night sleep hours were less than 9 hours, waking up more than three times and staying awake at night for more than one hour [5].
Sleep quality is influenced by several factors, namely appropriate rest needs, environment, physical exercise, nutrition and disease. Remember the importance of sleep time for babies, then the need for sleep must really be so as not to adversely affect its development. Quality sleep is determined by the presence of sleep disturbances, the baby is said to have sleep disturbances if the baby is awake at night for more than one hour [6].
Sleep has a significant effect on mental, emotional and physical health and the immune system [7]. The development of infant sleep is related to age and brain maturity, so the total amount of sleep needed is reduced, followed by a decrease in the proportion of Rapid Eyes Movement (REM) and non-REM. Sleep needs are not only seen from the aspect of quantity but also quality [8]. With good sleep quality, the baby's growth and development can be achieved optimally [9].
Sleep problems in children have various impacts, which have not been fully detailed, including growth disorders, cardiovascular disorders, cognitive function and daily behavior [10]. Several studies have stated that disruptive behaviour disorders, such as attention-deficit/hyperactivity disorder (ADHD), are sometimes caused by an undiagnosed sleep disorder [11]. Academic abilities at various age levels can also be affected by undetected sleep disturbances [12].
For the importance of sleep time for the development of the baby, then this need must be met entirely to avoid adverse effects on its development [13]. One of the efforts that can be done to improve the quality and quantity of baby sleep is massaging [14]. Baby massage is very beneficial for the health and development of babies. Regular baby massage will help reduce levels of stress hormones (catecholamines) and increase levels of immune substances in infants (immunoglobulins) while also stimulating digestive and excretory functions and increasing the baby's weight [15]. Massage can stimulate the release of endorphins that can reduce pain, so the baby becomes calm and reduces the frequency of crying. This massage also improves the quality and quantity of the baby's sleep [16].
An increase in the quantity of infant sleep after the massage is associated with increased levels of serotonin secretion [14]. Serotonin is the primary transmitter substance that triggers sleep by suppressing the activity of the reticular activating system and other brain activities [17].
Research conducted at the Touch Research Institute of America on 20 children massaged for 2x15 minutes within five weeks experienced 50% changes in brain waves compared to before the massage. These brain wave changes occur by decreasing alpha waves and increasing beta waves so that babies can sleep more soundly [18]. Based on research from the Warwick Medical School and the Institute of Education from the University of Warwick, examining nine kinds of baby massage movements performed on 598 babies under six months of age, the results showed that baby massage could make sleep patterns more regular because it is influenced by the sleep hormone melatonin which is influenced by baby massage performed [19].
The Muji Private Midwife is located in Kenali Asam, Jambi city, which provides baby massage services. An average of 25 babies is massaged per month. The results of interview with the baby's mother who came for baby massage, because babies like to wake up in the middle of the night, and the next day they like to cry and like to fuss. Based on this phenomenon, we are interested in examining the effect of infant massage on the sleep quality of infants aged 3-12 months in the Muji Private Midwife in Jambi City.
METHODS
The research method used in this study was a pre-experimental study with a pretest and posttest one group design conducted on infants at PMB Muji Kenali Asam Jambi City with 68 babies aged 3-12 months. Infants in the study who met the inclusion criteria set by the researcher, including infants aged 3-12 months, parents of babies willing to be respondents, babies who were breastfed and babies who were massaged three times during the study. The procedure for implementing baby steps in this study is guided by the baby massage procedure that has been used in previous studies [6,15,19] as follows: first, the researcher prepared baby oil, then a towel or blanket as a tool. The next step was to massage the legs, abdomen, and chest, massage the hands, face and finally massage the back. This procedure was carried out three days in a row, where every day, five babies received the intervention. Researchers measured sleep quality before implementing infant massage using a standardized questionnaire that has been tested for validity and reliability referring to Morrell's Infant Sleep Questionnaire (MISQ) [20] and A Brief Screening Problems (BSP) [21], and after three massages, the quality of sleep was measured again using the same questionnaire. No economic incentives were offered or provided for participation in this study. The study was performed in accordance with the ethical considerations of the Helsinki Declaration. This research has obtained ethical feasibility from the Health Research Ethics Commission of the Health Polytechnic of the Ministry of Health Jambi with LB.02.06/2/130/2020.
Statistical analysis
Data are presented as numbers and percentages for categorical variables. Continuous data are expressed as the mean ± standard deviation (SD), or median with Interquartile Range (IQR). The Wilcoxon test was performed to evaluate significant differences between two dependent groups. All tests with p-value (p) < 0.05 were considered significant. Statistical analysis was performed using SPSS app version 16.0
RESULTS
Research results are presented in the form of frequency distribution tables and inferential analysis tables. The characteristics of the baby are presented in the following table:

Table 1 Distribution of Babies by Gender, and Age
Based on the table above, the gender of the respondents is almost the same, with the difference between women being less than men, mostly aged 3 – 5 months 44.1% and both aged 6 – 8 months 26.5%. This data shows that the babies who come to PMB Muji are mostly babies aged three months to 8 months.
Distribution of baby's sleep quality before and after a baby massage can be seen in the following table:

Table 2. Distribution of Respondents Based on Sleep Quality of Babies Age 3-12 Months before Massage
Table 2 shows that the sleep quality of babies aged 3-12 months before baby massage was mostly of adequate quality, namely 31 respondents (45.6%). After stepping on the baby, most of the baby's sleep quality was adequate, namely 52.9%, there was an increase in good quality to 45.6%, only one had poor sleep quality.
The results of the inferential test using the Wilxocon test obtained the mean and standard deviation values as well as the p-value as presented in the following table:

Table 3. The effect of massage on the sleep quality of infants aged 3-12 months
Before the intervention, the mean score is 4.3235, and after the intervention, the mean score found is 5.3382. The mean difference between before and after the intervention is 1.0182. It can be seen that there has been an increase in the quality of sleep for babies 3-12 months after massaged which is 1. 0182. The results of the p-value showed that there was an effect of the baby's grip on the baby's sleep quality with sig. 0.001.
DISCUSSION
The sleep quality of infants aged 3-12 months before the massage mainly was adequate (45.6%) and less (27.9%). It is because many babies are fussy when they go to sleep (37%), babies look weak and cry when they wake up in the morning (73.5%), and babies always look fussy, cry and find it difficult to fall back asleep when they wake up (70.6%). The above situation occurs because the baby lacks sleep.
Inadequate sleep and poor sleep quality can lead to physiological and psychological balance disorders. Physiological impacts include decreased daily activities, fatigue, weakness, poor neuromuscular coordination, slow healing process and decreased immune system. At the same time, the psychological impact includes more unstable emotions, anxiety, and lack of concentration, lower cognitive abilities and combined experiences [22,23].
Many infants 3-12 months experienced less sleep. According to data obtained, 44.1% sleep less than 9 hours at night. Many factors may cause a baby to lack sleep, such as health status where an unhealthy baby will interfere with sleep, an uncomfortable environment such as too noisy, too hot, too cold, lighting that makes the baby sleepless and restless, psychological factors such as an anxious baby, there are scary sounds that make the baby feel scared which has an impact on sleeping often wakes up. The last is the dietary factor that also determines the baby's comfortable sleep or not. Babies who do not eat/are hungry or consume foods that contain gas cause bloating or drink too much at night, so they often wake up to urinate. In line with Wahyuni [24], babies who sleep enough without waking up frequently at night will be fitter and less fussy. Babies are said to have sleep disorders if they sleep less than 9 hours at night, wake up more than three times and wake up more than 1 hour.
Based on the results of data analysis after the baby was massaged, the sleep quality of infants aged 3 -12 months mainly was of sufficient quality (52.9%) and good quality (45.6%). Only 1.5% of infants experienced poor sleep quality. According to respondents, most of the babies who had been massaged (94.1%) looked cheerful and fit when they woke up and most stated that the babies did not look weak and cried when they woke up in the morning (95.6%). The quality and quantity of baby sleep affect physical development and emotional development [4]. Babies who get enough sleep without waking up are fitter and less fussy the next day. Not only has that, but lack of sleep also had an impact on the baby's thinking ability. If the body is tired, the quality of thinking becomes low. As a result, the baby cannot respond well. Babies who are sleep deprived become fussier, whiny and have trouble sleeping. For this solution, the baby needs to be massaged.
The baby is fast asleep after the massage because through the massage and the brain waves can change. This change occurs by decreasing alpha waves and increasing beta and theta waves proven by EEG (Electroencephalography) [17]. As for one baby after being given a baby foothold but did not show good sleep quality, according to research studies, it may be caused by several factors such as the habit of drinking milk before bed will also affect the quantity and quality of baby sleep. Meanwhile, the baby's bed environment is not comfortable, and the crowd in the family.
The effect of the baby's sleep quality is seen from the difference in mean values before and after massage. The mean value of the baby's sleep quality before massage was 4.3235 and after massage the mean was 5.3382 with a mean difference of 1.0182, this means that the baby after massage experienced an increase in sleep quality by 1.0182 points. p-value shows the effect of baby massage on baby's sleep quality with sig. 0.001. Another study on the relationship of massage infants with pattern and sleep in infants concluded that the touches given during infant massage were associated with increased infant sleep quality as indicated by an increase in the number of infant sleep duration and a reduction in infant sleep disturbances [25]. In contrast to this study, a study in Yogyakarta found that there was no effect between Infant Massage on weight gain and infant sleep quality [26].
CONCLUSIONS
Infant massage affects the sleep quality of infants aged 3-12 months before and after the intervention with a mean difference of 1.0182, which means that massage can improve the quality of infant sleep by 1.0182 points with a p-value of 0.001 (p <0.05).
LIMITATION
The limitation of this study is that it does not control other factors that can affect the quality of baby sleep, and than this intervention was only carried out in one place, namely at PMB Muji Kenali Asam Jambi City.
ACKNOWLEDGEMENT
We would like to express our gratitude to several parties who have provided support for our research. To the chief of the Poltekkes Jambi in her support in providing suggestions and input for the development of this research, and to mothers who have actively participated as respondents in this research.
CONFLICT OF INTEREST
The author(s) declares no conflict of interest.
FUNDING STATEMENT
The author(s) received no financial support for the research, authorship, and/or publication of this article.
REFERENCES
- Imai CM, Gunnarsdottir I, Thorisdottir B, Halldorsson TI, Thorsdottir I. Associations between infant feeding practice prior to six months and body mass index at six years of age. Nutrients. 2014;6(4):1608–17.
- Minarti NMA, Utami KC. Pengaruh Pijat Bayi Terhadap Kualitas Tidur Bayi Usia 3-6 Bulan Di Wilayah Kerja Puskesmas II Denpasar Timur Tahun 2012. Jakarta: EGC. 2012.
- Price AMH, Wake M, Ukoumunne OC, Hiscock H. Outcomes at six years of age for children with infant sleep problems: longitudinal community-based study. Sleep Medicine. 2012;13(8):991–8.
- Sekartini R, Adi NP. Gangguan tidur pada anak usia bawah tiga tahun di lima kota di Indonesia. Sari pediatri. 2016;7(4):188–93.
- Muawanah S. Efek Pemberian Massage Bayi Dapat Meningkatkan Kualitas Tidur Bayi Normal Usia 0–6 Bulan. Jurnal Ilmiah Fisioterapi. 2019;2(1):27–34.
- Sadiman S, Islamiyati I. Efektifitas Pijat Bayi terhadap Peningkatan Berat Badan, Lama Waktu Tidur dan Kelancaran Buang Air Besar. Jurnal Kesehatan Metro Sai Wawai. 2020;12(2):9–16.
- Haack M, Mullington JM. Sustained sleep restriction reduces emotional and physical well-being. Pain. 2005;119(1–3):56–64.
- Jiang F. Sleep and early brain development. Annals of Nutrition and Metabolism. 2019;75(1):44–54.
- Kusumastuti NA, Tamtomo D, Salimo H. Effect of massage on sleep quality and motor development in infant aged 3-6 months. Journal of maternal and child health. 2016;1(3):161–9.
- Tanjung MFC, Sekartini R. Masalah tidur pada anak. Sari Pediatri. 2016;6(3):138–42.
- Retnaningsih D, Kustriyani M. Hubungan Antara Kualitas Tidur dengan Konsentrasi Belajar pada Anak Usia Sekolah di SD Negeri 3 Candisari Kecamatan Purwodadi Kabupaten Grobogan. Jurnal Ners Widya Husada. 2018;1(1).
- Sidiarto LD. Perkembangan Otak dan Kesulitam Belajar Pada Anak. Penerbit Universitas Indonesia (Ul-Press); 2007.
- Sadeh A, Gruber R, Raviv A. Sleep, neurobehavioral functioning, and behavior problems in school‐age children. Child development. 2002;73(2):405–17.
- Dieter JNI, Field T, Hernandez-Reif M, Emory EK, Redzepi M. Stable preterm infants gain more weight and sleep less after five days of massage therapy. Journal of pediatric psychology. 2003;28(6):403–11.
- Pamungkas BA, Susilaningsih EZ, Kp S, Kep M. Pengaruh Pijat Bayi Terhadap Kualitas Tidur Bayi Umur 0-6 Bulan di Puskesmas Kartasura. Universitas Muhammadiyah Surakarta; 2016.
- Harahap NR. Pijat Bayi Meningkatkan Berat Badan Bayi Usia 0-6 Bulan. Jurnal Kesehatan Prima. 2019;13(2):99–107.
- Handayani N, Azza A, Rhosma S. Pengaruh Pijat Bayi Terhadap Kualitas Tidur Bayi Usia 3-5 Bulan di Desa Plalangan dan Desa Ajung Kecamatan Kalisat. 2015.
- Afriyanti D. Effects of Baby Massage Using Lavender Aromatherapy In Fulfillment Of Sleep Need Among Baby Age 6-12 Months In The Working Area Nilam Sari Health Center Bukittinggi In 2017. Journal of Midwifery. 2018;3(1):13–24.
- Haryanti RS. Pengaruh loving tauch baby massage terhadap pola tidur batita. Profesi (Profesional Islam): Media Publikasi Penelitian. 2019;17(1):61–8.
- Morrell JMB. The infant sleep questionnaire: a new tool to assess infant sleep problems for clinical and research purposes. Child Psychology and Psychiatry Review. 1999;4(1):20–6.
- Sadeh A. A brief screening questionnaire for infant sleep problems: validation and findings for an Internet sample. Pediatrics. 2004 Jun;113(6):e570-7.
- Eliza S. Hubungan Pijat Bayi dengan Lamanya Tidur Bayi Usia 0-12 Bulan. Java Health Jounal. 2014;1(1).
- Akib H, Merina ND. The Influence of Baby Massage on Baby Sleep Quantity in Bedadung Village, Sumbersari Subdistrict Jember District. Jurnal Kesehatan dr Soebandi. 2018;6(1).
- Afrina DN, Rahayu UB, Wahyuni Ss. Pengaruh Baby Solus Per Aqua (Spa) Terhadap Kuantitas Tidur Bayi Usia 6-9 Bulan. Universitas Muhammadiyah Surakarta; 2012.
- Roth DE. The Relationship Massage Infant With Pattern And Sleep In Infants. journal of pediatric. 2010;
- Fauziah A, Wijayanti HN. Pengaruh Pijat Bayi terhadap Kenaikan Berat Badan dan Kualitas Tidur Bayi di Puskesmas Jetis Yogyakarta. PLACENTUM: Jurnal Ilmiah Kesehatan dan Aplikasinya. 2018;6(2):14–9.
THE ROLE OF HYPERBARIC OXYGEN THERAPY IN FOURNIER'S GANGRENE: LITERATURE REVIEW
Vincenza Giordano 1 *, Luca Cardillo 2
- Nurse with Master's Degree in Nursing and Midwifery Sciences, AORN Antonio Cardarelli
- Nurse and Business Trainer at A.S.L Napoli 2 NORD (Hospital Santa Maria delle Grazie)
*Corresponding Author: Dr. Vincenza Giordano, Nurse with Master's Degree in Nursing and Midwifery Sciences, AORN Antonio Cardarelli
E-mail: enza-giordano@hotmail.it
Cita questo articolo
ABSTRACT
Introduction: Fournier's Gangrene is a severe necrotising infection that can be fatal if not recognised and treated immediately. Treatment consists of a combination of conventional therapy with a multidisciplinary approach (early diagnosis, surgical debridement, antibiotic therapy, intensive care and reconstructive surgery) and adjuvant therapy with hyperbaric oxygen therapy sessions.
Objective: To identify the role and evaluate the efficacy of hyperbaric oxygen therapy in Fournier's gangrene.
Method: To conduct the following narrative review a research question was outlined using the PIO methodology. Subsequently, a literature review was conducted using the PubMed, Scopus and CINAHL Complete databases from December 2020 to February 2021.
Results: Eight studies emerged from the literature review showing that the use of adjuvant Hyperbaric oxygen therapy (HBOT) in combination with classical treatment has beneficial effects and enhances the efficacy of hyperbaric oxygen therapy, resulting in lower mortality rates, in contrast to the average number of hospital days spent in intensive care, which do not undergo any significant change. But in contrast to mortality, the average number of days spent in intensive care differed significantly in favour of the standard treatment group.
Conclusion: The combined effect of hyperbaric oxygen therapy with conventional therapy offers a significant advantage in the management of FG; furthermore, HBOT is associated with a significant survival advantage.
Keywords: Fournier's gangrene, Fournier's disease, Hyperbaric oxygen therapy and HBOT
INTRODUCTION
Necrotising fasciitis, better known as "Fournier's Gangrene" (FG), is a polymicrobial infection caused by aerobic and anaerobic microorganisms acting synergistically to cause severe soft tissue infection (NSTI), targeting the genital, perineal and perianal region [1,2]. The term, coined by the scholar Wilson, first appeared in the scientific world in 1952 [3]. FG is now considered a rare disease [4-6], predominantly affecting males (10 to 1 ratio) with a mean age of 50 years [4,7], with an incidence rate ranging from 0.3 to 15.5 cases per 100000 inhabitants [8,9]. It is associated with high morbidity and mortality between 3% and 67% [4]. FG has a subtle and rapid pathogenesis, so much so that some authors have divided the disease into 4 phases[5]: (i) the initial phase occurs within 24-48 hours and is associated with non-specific symptoms, such as itching, oedema, erythema and partial hardening of the affected tissues; (ii) the second phase is brief and invasive with the presence of local inflammatory manifestations; (iii) the third phase is the necrotic phase in which there is a rapid deterioration, which may evolve into septic shock, with the risk of spreading necrosis to the anterior abdominal wall and thighs; (iv) the fourth phase is one of spontaneous repair which occurs after a few months, during which epithelial regeneration and healing take place [5]. From an aetiological point of view, the bacteria responsible for this infection include group A Streptococcus as the most common monomicrobial culprit [10,11], while Escherichia coli, Bacteroides, Staphylococcus, Proteus, Streptococcus, Pseudomonas and Enterococcus are among the polymicrobial culprits [12,13]. Microorganisms have been found in the urogenital tract and in the digestive tract: the causes of bacterial presence in the urogenital tract are urethral stenosis, scrotal abscesses, orchitis, epididymitis, renal abscess, ureteral trauma, renal calculosis, bladder and penile cancer, prostate biopsy and catheterization [14,15], while the presence of bacteria in the digestive tract is found in outbreaks originating from perianal abscesses, colorectal tumours, appendicitis, acute diverticulitis, Crohn's disease, incarcerated hernias and perforation of the rectum, particularly caused by a foreign body [16,17]. Without treatment, the process may not only rapidly spread to the abdominal wall, dorsal region, upper limbs and retroperitoneum, but also lead to sepsis, multi-organ failure and death [1,18,19]. Systemic diseases listed as risk factors for the development of FG include: diabetes mellitus, alcoholism, hypertension, obesity, smoking, immune suppressive conditions such as HIV infection, radiotherapy and chemotherapy [4,7,20-23]. In terms of semeiotics, the most frequent manifestations include pain, erythema, oedema and necrosis of the scrotum or the perianal and perineal region, often associated with fever and chills [24-26]. Other symptoms are mostly localised and include the presence of blisters, crackles, cyanosis and malodorous discharge; however, it should be emphasised that the skin manifestations are the 'tip of the iceberg', while the infection spreads rapidly and aggressively along deep fascial planes [27,28]. The FGSI (Fournier's Gangrene Severity Index) scale is used to estimate the severity of Fournier's gangrene. It uses 9 parameters: temperature, pulse, respiratory rate, sodium, potassium and creatinine levels, haematocrit, leukocytosis and bicarbonate levels. Each parameter is assigned a score from 0 to 4. A high FGSI score denotes a worse prognosis [29]. Treatment of FG includes management of sepsis according to guidelines (early diagnosis, surgical debridement, antibiotic therapy, intensive care and reconstructive surgery) [30] and hyperbaric oxygen therapy (HBOT) is highly recommended whenever possible [31].
Hyperbaric oxygen therapy is a therapeutic approach that involves the use of 100% pressurised oxygen, which is delivered in an airtight chamber. HBOT has a bactericidal action on anaerobes and reduces the activity of endotoxins in the presence of high oxygen levels. This treatment has provided benefits such as improved neutrophil phagocytic action, fibroblast proliferation and angiogenesis, reduced oedema, absence of free radicals and increased intracellular transport of antibiotics [32,33]. Adverse effects associated with this treatment approach are relatively rare, but there are not enough studies that have investigated the role of HBOT in FG [34,35]. Among the few studies presented in literature, adverse events include barotrauma of the tympanic membrane and paranasal sinuses, the possibility of sudden onset of epileptic seizures and pulmonary and central nervous system toxicity caused by oxygen[36]. However, the use of hyperbaric oxygen therapy in the management of FG is widely discussed, sometimes even controversially, because clinical evidence regarding HBOT in these infections is scarce and of generally low quality and, moreover, the use of hyperbaric oxygen therapy is not standard of care in many centres, so much so that some authors recommend HBOT as an adjuvant treatment [37], while others do not recommend it as routine use in the management of FG [38]. This literature review aims to investigate the role that HBOT plays in Fournier's gangrene, its effectiveness and influence on some variables. Some studies show that HBOT reduces the extent of necrosis, mortality, morbidity rates [39,40] and the need for further surgery [41]. The strength of this review is to highlight that, although oxygen therapy is a second-line treatment, in all the studies reported in this review, it still plays a decisive role in the treatment of Fournier's gangrene, as it allows restitutio ad integrum.
Objective of the study
Identify the role and evaluate the effectiveness of hyperbaric oxygen therapy in Fournier's gangrene.
MATERIALS AND METHODS
Study design
A narrative review of the literature was conducted using an evidence method. To conduct the review, a research question was outlined using the Population, Intervention, Outcome (PIO) methodology. The PIO specifies the population to be studied, the intervention to be implemented and the outcomes (Table 1).

Table 1. Question according to the PIO method. FG= Fournier's gangrene
Research strategy
The research of the articles was carried out through the following databases PubMed, Scopus and CINAHL Complete in the time period from December 2020 to February 2021.
The following keywords were used:
"Fournier’s Gangrene", "Fournier’s Disease", "Gangrena de Fournier", "Hyperbaric Oxygen Therapy", "hbot", "hyperbaric oxygen" and "oxygen therapy".
For each MeSH term, the respective synonyms have been identified in each database. Next, advanced search terms were set up, using the Boolean operators 'OR' and 'AND' to cross terms in different combinations and make the search more specific. The only limit included is the date of publication: only articles published within the last 10 years were taken into account.
The formulation of the keywords and MeSH terms was carried out jointly by the two authors in order to comply with validity criteria and reduce search bias . Similarly, the authors also collaborated in the retrieval of articles and full-texts and their respective evaluations, to identify reports relevant to the research topic. The search terms are shown in Table 2.
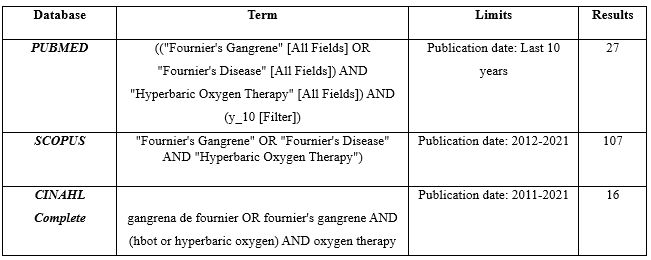
Table 2. Search terms
Inclusion and exclusion criteria
The following criteria were set for the search. We included (a) primary studies; (b) studies carried out on the adult population of both sexes; (c) studies published in the past 10 years. We excluded: (A) secondary studies; (b) editor's reviews and / or letters to the editor; (c) studies with subjects under the age of 18; (d) studies in which the role of hyperbaric oxygen therapy was not fully exposed. The detailed procedure used in the selection of articles is presented below in the form of a flow chart shown in Figure 1.
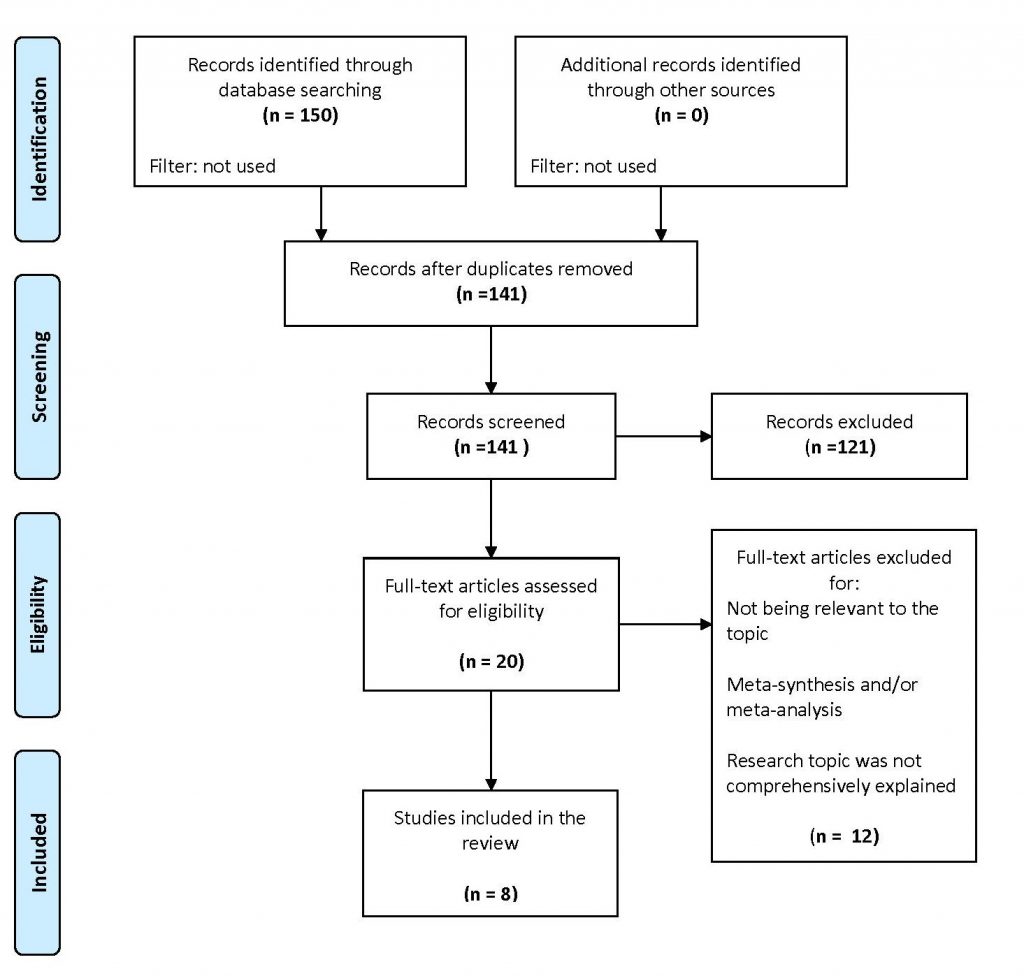
Figure 1. PRISMA Flow Diagram of the literature review
Our search strategy yielded a total of 150 preliminary stage articles (27 on Pubmed ,107 on Scopus and 16 on CINAHL Complete). 9 duplicate articles were excluded. The remaining 141 were assessed by title and abstract, 121 were discarded because they were not relevant to the objective or inconsistent with the inclusion criteria. Of the 20 remaining articles, after reading the full-text, 12 records were discarded as they were secondary studies or not relevant to the research question. 8 articles were included in the review after a full evaluation of the text. The two authors independently conducted the literature review and no discrepancies emerged between the evaluators.
RESULTS
Eight studies relevant to our question emerged and Table 3 summarises their characteristics and results. Fournier's Gangrene is a severe necrotising infection that can be fatal if not detected and treated immediately. Treatment consists of a combination of conventional therapy with a multidisciplinary approach (early diagnosis, surgical debridement, antibiotic therapy, intensive care and reconstructive surgery) and adjuvant therapy with hyperbaric oxygen therapy sessions. This is confirmed in the articles that follow. A retrospective study [42] has shown that the use of adjuvant HBOT, in combination with classic treatment is associated with reduced mortality: this percentage was lower in the group treated with HBOT than in the control group treated with the standard approach ( 3.7% vs 28.8%). This finding is further confirmed in other studies [43,44]: in the retrospective, multicentre observational study by Anheusera et al. [44], mortality in patients treated with HBOT was 0% vs. 4.4% mortality for patients not receiving adjuvant treatment. In the latter study, as opposed to mortality, a variable on which it is important to pay attention was the average days spent in intensive care, which differed significantly in favour of the standard treatment group. In fact, the frequency of wound debridement and hospital stay were significantly higher in the hyperbaric oxygen therapy group (13 vs 5 debridements and 40 vs 22 days). However, the latter contrasts with a retrospective, multicentre study present in the literature [45], in which the variables of length of hospital stay, direct costs of hospital stay, complications and mortality in the three FG classes (minor, moderate and major), regardless of treatment, were not significantly different. In contrast, subjects receiving adjuvant therapy with HBOT had a lower rate of complications (45% vs. 66%) and deaths (4% vs. 23). In a retrospective analysis of 60 patients, first treated with broad-spectrum antibiotics and then undergoing surgery within 24 hours of admission, it was observed that fasciotomy alone was an insufficient treatment and that in many patients debridement was necessary (average of 3.1 debridements), combined with early diagnosis, intensive care and in some cases colostomy, with the addition of hyperbaric oxygen therapy sessions, which demonstrated an increase in survival [46]. In this study, 12 patients were treated with HBOT, with a survival rate of 100% (12/12 patients), compared to 66.7% (32/48) of patients who did not undergo HBOT. In addition, hyperbaric oxygen therapy, as shown in Chao et al's case-control study [29] of 28 subjects, reduces infection rates and improves prognosis, although the most effective method for FG remains surgical treatment. However, due to the depth of the retroperitoneal space, the presence of large cavities and soft tissue, the lesions are diffuse and it is often difficult to completely debride the necrotic tissue during surgery. Therefore in such conditions, hyperbaric oxygen therapy used as an adjunct to standard therapy can reduce debridement sessions and times, shorten the length of drainage tube use, reduce healing time and improve the prognosis process of FG. In this study, as in previous studies, the experimental group had a lower mortality rate than the non-HBOT control group (12.5% vs. 33.3%). These findings are supported by two studies: a retrospective and descriptive study conducted by accessing the medical records of 34 FG patients who underwent HBOT from 1989 to 2014 [47] and a single-center, case-control study involving 341 subjects, which described the potential benefits of HBOT in FG from a pathophysiological perspective (inflammation, modulation of reperfusion injury and facilitation of wound healing), with respective reduction in mortality [48].
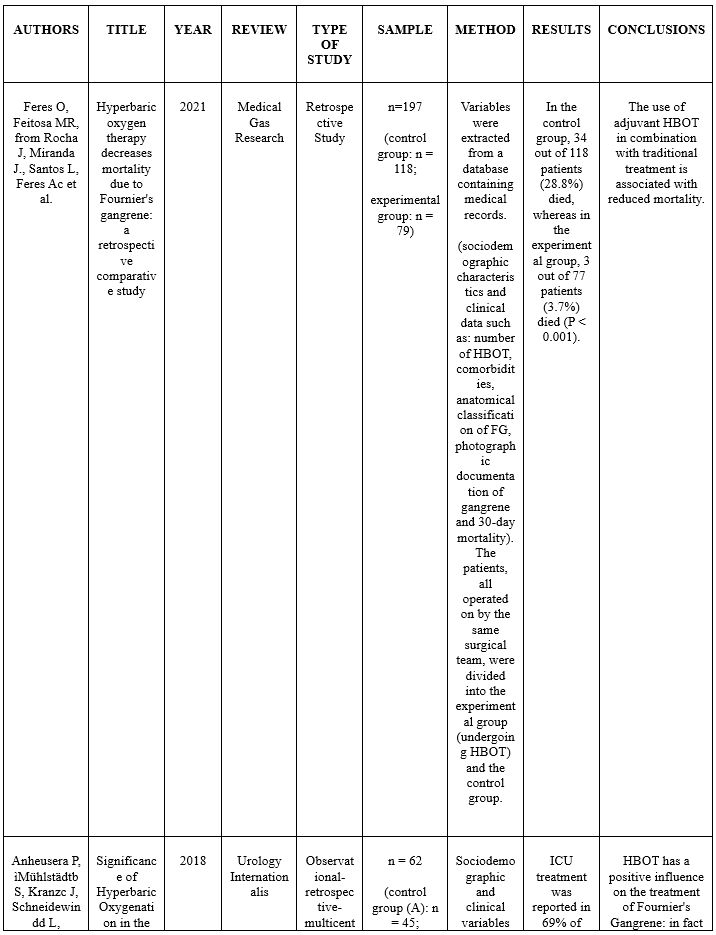
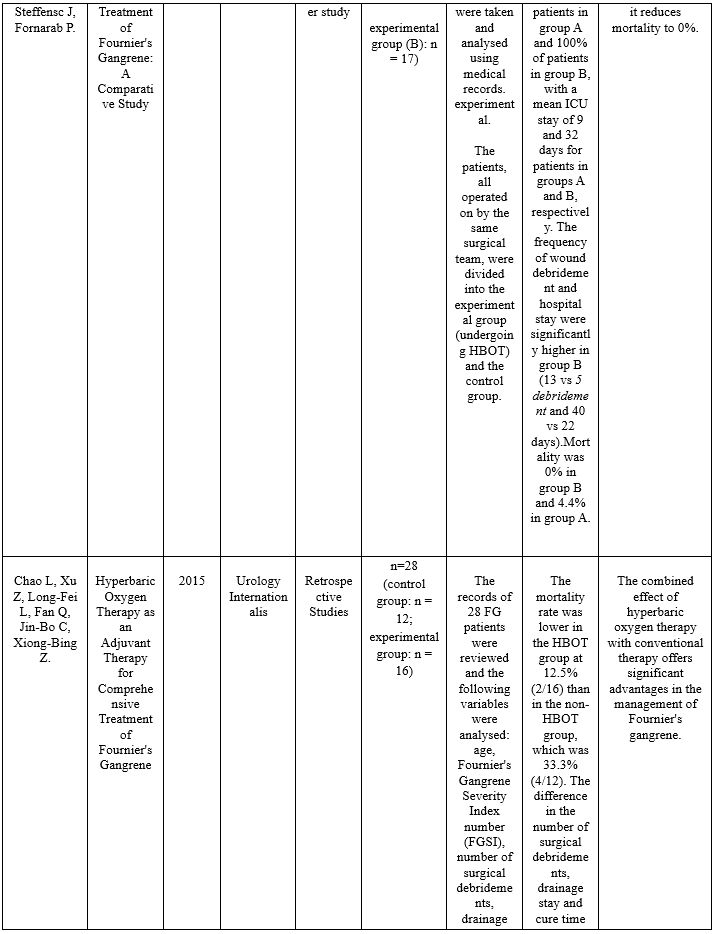
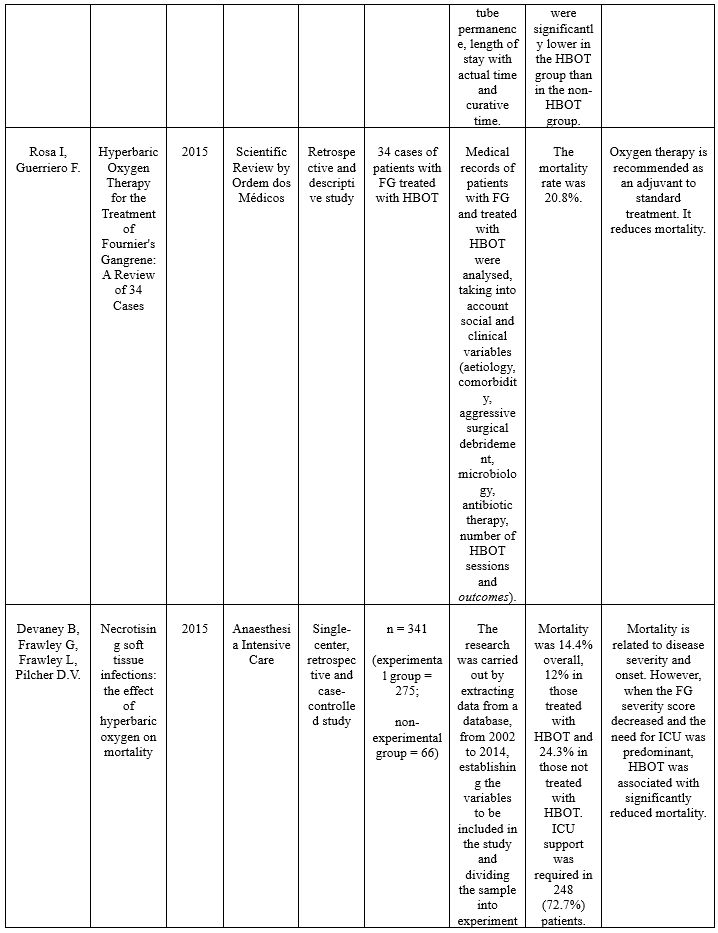
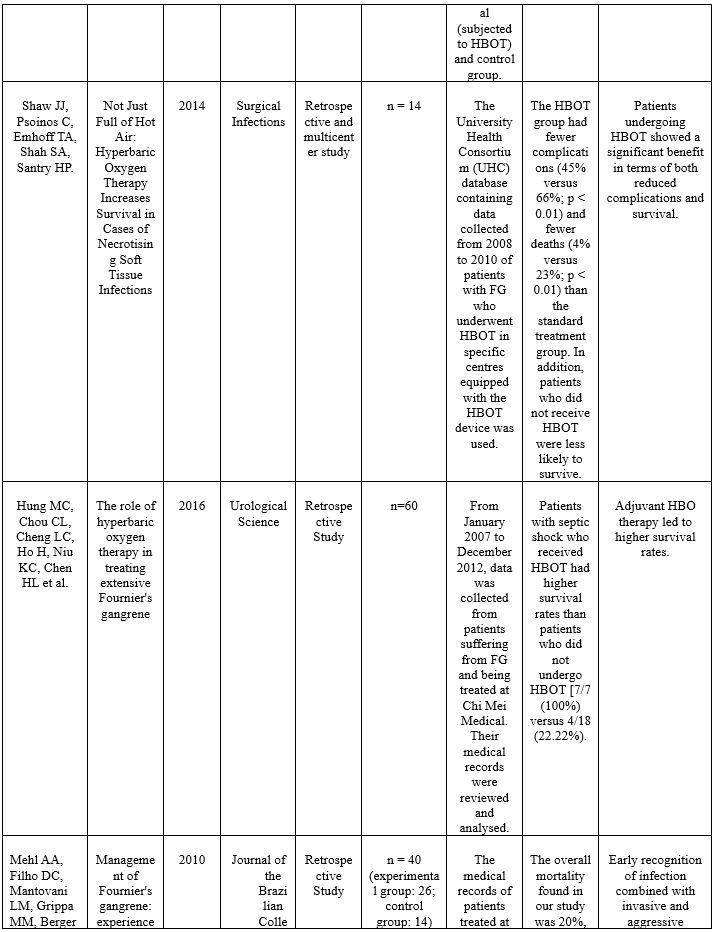
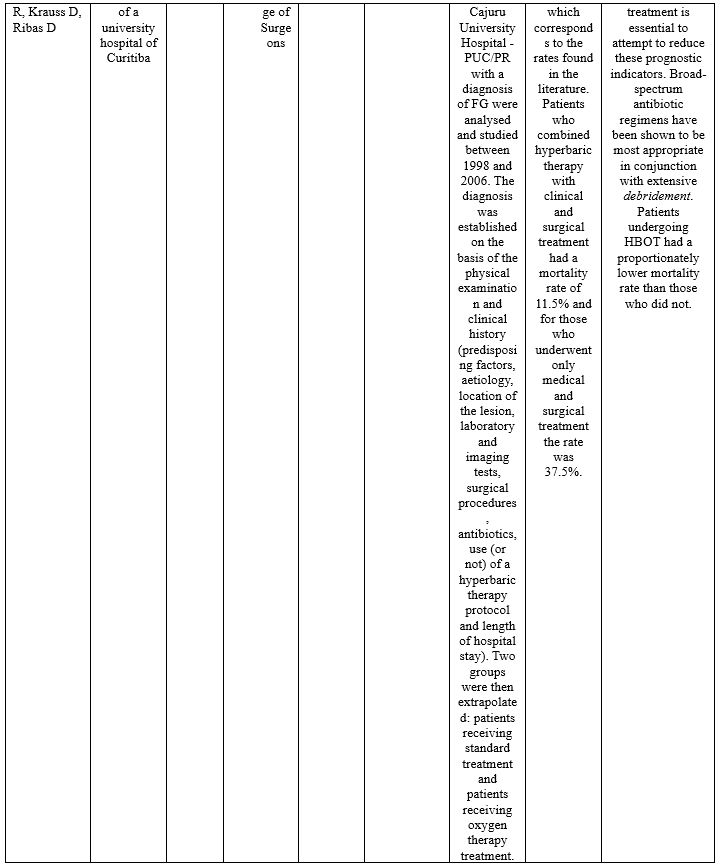
Table 3. Analysis of the studies included within the review.
DISCUSSION
The aim of the review was to identify the role and assess the effectiveness of hyperbaric oxygen therapy in Fournier's Gangrene. From the studies analysed, it is clear that the primary treatment of Fournier's Gangrene uses a multidisciplinary approach based on conventional therapy (early diagnosis, surgical debridement , antibiotic therapy, intensive care and reconstructive surgery). In recent years, hyperbaric oxygen therapy has shown to have an adjuvant role in the treatment of FG, but at the same time a decisive one, as it has allowed a return ad integrum with or without surgery. In fact, due to the depth of the retroperitoneal space, the large cavities and non-linear tissue, and the diffuse lesions, it is often difficult to define and carry out a complete debridement of the necrotic tissue during surgery, so that tissue hypoxia and infection factors interact and in the post-operative period, poor drainage or the onset of other factors favour the spread of the disease. Therefore it becomes necessary in such conditions, to find an adjuvant therapy that can reduce the infection rates and improve the prognosis. HBOT acts as a bactericide and/or bacteriostatic against anaerobic bacteria by increasing the formation of oxygen free radicals and restores the bactericidal capacity of leukocytes in hypoxic wounds by increasing tissue oxygen tension; in addition, HBOT interacts synergistically with several antibiotics to enhance their effect and thus reduce complications that may occur. Oxygen therapy is commonly started as soon as patients are stabilised (after initial debridement) and continued until the wound is completely healed. HBOT as an adjunctive therapy may reduce debridement sessions and drainage tube time in situ; but the efficacy of hyperbaric oxygen therapy is demonstrated by the exponential decrease in mortality rates reported in all studies, even in those patients where FG is associated with critical situations such as septic shock. It is not possible, however, to conclude that HBOT has a real positive influence on the reduction of average days of hospitalisation and treatment in intensive care units and consequently on health care expenditure, as the studies in the literature are conflicting. In fact, although HBOT has potential in FG therapy, not all hospitals have or can allow the patient rapid access to hyperbaric chambers and the degree of critical illness accompanying gangrene often precludes access to oxygen therapy. Moreover, there is no established treatment protocol for HBOT and given the rarity of FG cases, it is often very difficult to carry out studies, which is why the role of hyperbaric oxygen therapy is much discussed and, at the same time, a matter of controversy. It must be said that there has not been enough studies carried out in the literature to introduce this type of therapy as a first-line treatment in the clinical routine, but only as a second-line treatment, supporting standard therapy (early diagnosis, surgical debridement, antibiotic therapy, intensive care and reconstructive surgery).
CONCLUSION
The results in the literature review suggest that the combined effect of hyperbaric oxygen therapy with conventional therapy offers a significant advantage in the management of FG and that HBOT is associated with a significant survival benefit. Multicentre studies with a larger sample size are needed to confirm these observations, but are difficult to conduct due to the rarity of FG and the limited availability of HBOT in some centres. With a better understanding of the disease and treatment experience, the management of FG could see significant developments in the future.
ABBREVIATIONS
FG (Fournier's gangrene)
FGSI (Fournier's Gangrene Severity Index)
HBOT (Hyperbaric oxygen therapy)
ICU (Intensive Care Unit)
PIO (Population, Intervention, Outcome)
Conflicts of interest
The authors state that they have no conflicts of interest associated with this literature review.
Funding
The authors declare that they have not received any form of funding and that the study has no financial sponsor.
REFERENCES
- Atakan, IH, Kaplan M, Kaya E, Aktoz,, & Inci, O. A life-threatening infection: Fournier’s gangrene. International Urology and Nephrology. 2002; 34: 387-392.
- Morpurgo E & Galandiuk S. Fournier’s gangrene. Surgical Clinics of North America, 2002; 82: 1213-1224.
- Wilson B. Necrotizing fasciitis. The American Journal of Surgery. 1952; 18: 416-431.
- Shyam DC & Rapsang AG. Fournier's gangrene. Surgeon. 2013; 11: 222–232.
- Horta R, Cerqueira M, Marques M, Ferreira P, Reis J, Amarante J. Fournier’s gangrene: from urological emergency to plastic surgery. Actas Urol Esp. 2009; 33: 925–929.
- Sorensen MD, Krieger JN, Rivara FP, Broghammer JA, Klein MB, Mack CD, et al. Fournier's gangrene: population based epidemiology and outcomes. Journal of Urology. 2009; 181: 2120-6.
- Eke N. Fournier's gangrene: a review of 1726 cases. British Journal of Surgery. 2000; 87: 718-728.
- Khamnuan P, Chongruksut W, Jearwattanakanok K, Patumanond J, Tantraworasin A. Necrotizing fasciitis: epidemiology and clinical predictors for amputation. International Journal of General Medicine; 2015; 8: 195–202.
- Bocking N, Matsumoto CL, Loewen K, Teatero S, Marchand-Austin A, Gordon J et al. High incidence of invasive group A streptococcal infections in remote indigenous communities in northwestern Ontario, Canada. Open Forum Infectious Disease. 2016; 4: ofw243.
- Stevens DL & Bryant AE. Necrotizing soft-tissue infections. The New England Journal of Medicine, 2017; 377: 2253–2265.
- Wong CH, Chang HC, Pasupathy S, Khin LW, Tan JL, Low CO. Necrotizing fasciitis: clinical presentation, microbiology, and determinants of mortality. The Journal of Bone and Joint Surgery American. 2003; 85, (A): 1454–1460.
- Basoglu M, Ozbey I, Atamanalp S, Yildirgan MI, Aydinli B, Polat O et al. Management of Fournier's gangrene: review of 45 cases. Surgery Today. 2007; 37 (7): 558-563.
- Nomikos IN. Necrotizing perineal infections (Fournier's disease): old remedies for an old disease. International Journal of Colorectal Disease. 1998; 13 (1): 48–51.
- Clayton MD, Fowler JE, Sharifi R & Pearl R.K. Causes, presentation and survival of fifty-seven patients with necrotizing fasciitis of the male genitalia. Surgery, Gynecology, Obstetrics archives. 1990; 170: 49-55.
- Korkut M, Içöz G, Dayangaç M, Akgun E, Yeniay L., Erdogan, O et al. Outcome analysis in patients with Fournier's gangrene: report of 45 cases. Disease of the Colon & Rectum. 2003; 46: 649-652.
- Murakami M, Okamura K, Hayashi M, Minoh S, Morishige I. & Hamano K. Fournier's gangrene treated by simultaneously using colostomy and open drainage. Journal of Infection; 2006; 53; and 15-18.
- Ochiai T, Ohta K, Takahashi M, Yamazaki S. & Iwai T. Fournier's gangrene: report of six cases. Surgery Today. 2001; 31: 553-556.
- Safioleas M, Stamatakos M, Mouzopoulos G, Diab A, Kontzoglou K & Papachristodoulou A. Fournier’s gangrene: exists and it is still lethal. Surgical Clinics of North America. 2006; 38: 653-657.
- Jeong HJ, Park SC, Seo IY & Rim JS. Prognostic factors in Fournier gangrene. International Urology and Nephrology; 2005 12: 1041-1044.
- McKay TC & Waters WB Fournier's gangrene as the presenting sign of an undiagnosed human immunodeficiency virus infection. Journal of Urology. 1994; 152: 1552-1554.
- Sarani B, Strong M, Pascual J & Schwab CW. Necrotizing fasciitis: current concepts and review of the literature. Journal of the American College of Surgeon. 2009; 208: 279-88.
- Cardoso JB & Féres O. Grangena de Fournier. Medicina. 2007; 40: 493-9.
- Torremadé Barreda J, Millán Scheiding M, Suárez Fernández C, Cuadrado Campaña JM, Rodríguez Aguilera J, Franco Miranda E, et al. Fournier gangrene. A retrospective study of 41 cases. Cirugía Española. (English Ed). 2010; 87: 218-23.
- Uppot RN & Levy HM. Patel PH. Case 54: Fournier gangrene. Radiology. 2003; 226: 115-117.
- Smith GL, Bunker CB & Dinneen MD. Fournier's gangrene. British Journal of Surgery, 1998; 81: 347-355.
- Rotondo N. Fournier’s gangrene: an unusual presentation of sepsis. The Journal of Emergency Medicine. 2002; 23: 413-414.
- Saffle JR, Morris SE & Edelman L.Fournier's gangrene: management at a regional burn center. J Burn Care Res.2008; 29: 196-203
- Villanueva-Sáenz E, Martínez Hernández-Magro P, Valdés Ovalle M, Montes Vega J, Alvarez-Tostado FJF. Experience in management of Fournier's gangrene. Tech Coloproctol. 2002; 6: 5-13
- Chao L, Xu Z, Long-Fei L, Fan Q, Jin-Bo C & Xiong-Bing Z. Hyperbaric Oxygen Therapy as an Adjuvant Therapy for Comprehensive Treatment of Fournier's Gangrene. Urology Internationalis 2015; 94 (4): 453-8.
- Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shocks. Intensive Care Medicine. 2008; 34 (1): 17–60.
- Jallali N, Withey S & Butler PE. Hyperbaric oxygen as adjuvant therapy in the management of necrotizing fasciitis. American Journal of Surgery. 2005; 189 (4): 462-466
- de Nadai TR, Daniel RF, de Nadai MN, da Rocha JJ, Féres O. Hyperbaric oxygen therapy for primary sternal osteomyelitis: a case report. Journal of Medical Case Report.2013; 7:67.
- Parra RS, Lopes AH, Carreira EU, Feitosa MR, Cunha, FQ, Garcia SB et al. Hyperbaric oxygen therapy ameliorates TNBS-induced acute distal colitis in rats, Medical Gas Reserch. 2015; 5.6.
- Plafki C, Peters P, Almeling M, Welslau W & Busch R. Complications and side effects of hyperbaric oxygen therapy. Aviation, Space, and Environmental Medicine. 2000; 71: 119–124.
- Lo T, Song C, Alismail A, et al. Hyperbaric oxygen therapy: how safe is it for critically ill patients? Critical Care Medicine. 2014; 42: A1520.
- Smerz RW. Incidence of oxygen toxicity during the treatment of dysbarism. Undersea & Hyperbaric Medical Society.2004; 31: 199–202
- D'Agostino Dias M, Fontes B, Poggetti RS, Birolini D. Hyperbaric oxygen therapy: types of injury and number of sessions--a review of 1506 cases. Undersea & Hyperbaric Medical Society.2008; 35: 53-60.
- Mindrup SR, Kealey GP, Fallon B. Hyperbaric oxygen for the treatment of fournier’s gangrene. Journal of Urology. 2004; 173: 1975-1977.
- Creta M, Longo N, Arcaniolo D, Giannella R., Cai T, Cicalese A et al. Hyperbaric oxygen therapy reduces mortality in patients with Fournier's Gangrene. Results from a multi-institutional observational study. Minerva Urology and Nefrology.2020; 72: 223-228.
- Hollabaugh RS, Dmochowski RR, Hickerson WL, Cox CE. Fournier's gangrene: therapeutic impact of hyperbaric oxygen. Plast Reconstructive Surgery.1998; 101: 94-100.
- Korhonen K, Hirn M, Niinikoski J. Hyperbaric oxygen in the treatment of Fournier’s gangrene. European Journal of Surgery. 1998; 164: 251-255.
- Feres O, Feitosa MR, Ribeiro da Rocha JJ, Miranda JM, Dos Santos LE, Féres AC et al. Hyperbaric oxygen therapy decreases mortality due to Fournier's gangrene: a retrospective comparative study. Medical Gas Research 2021; 11 (1): 18-23.
- Mehl AA, Filho DC, Mantovani LM, Grippa MM, Berger R, Krauss D, Ribas D. Management of Fournier's gangrene: experience of a university hospital of Curitiba. Rev Col Bras Cir. 2010; 37 (6): 435-41.
- Anheusera P, Mühlstädtb S, Kranzc J, Schneidewindd L, Steffensc J, Fornarab P. Significance of Hyperbaric Oxygenation in the Treatment of Fournier's Gangrene: A Comparative Study. Urology Internationalis 2018; 101: 467–471.
- Shaw JJ, Psoinos C, Emhoff TA, Shah SA, Santry HP. Not Just Full of Hot Air: Hyperbaric Oxygen Therapy Increases Survival in Cases of Necrotizing Soft Tissue Infections. Surgical Infections. 2014; 15 (3): 328-335.
- Hung MC, Chou CL, Cheng LC, Ho H, Niu KC, Chen HL et al. The role of hyperbaric oxygen therapy in treating extensive Fournier's gangrene Urological Science 2016; 27 (3): 148-153.
- Rosa I & Guerriero F. Hyperbaric Oxygen Therapy for the Treatment of Fournier's Gangrene: A Review of 34 Cases. Scientific Review by Ordem dos Médicos 2015; 28 (5): 619-623.
- Devaney B, Frawley G, Frawley L, Pilcher D.V. Necrotising soft tissue infections: the effect of hyperbaric oxygen on mortality. Anaesthesia Intensive Care. 2015; 83 (6): 685-92.
La paura nell’anziano: una ricerca intervento basata sull’osservazione partecipe
Giulia Bindi1 and Gabriele Giacomelli*2
- Dipartimento di infermieristica ospedaliera, A. O. U. Careggi, Firenze
- Dipartimento di infermieristica territoriale, USL Toscana Centro
* Corresponding Author: Gabriele Giacomelli, Assistenza Infermieristica Territoriale USL Toscana Centro & Scuola di Scienze della Salute, Facoltà di Medicina e Chirurgia, Corso di Laurea in Infermieristica, Università Firenze (Italia). E-mail: gabriele@relazioniesalute.it
Cita questo articolo
ABSTRACT
Introduzione: La fragilità dell’anziano è fisica e psichica e su di entrambe vi è influenza degli eventi stressanti della vita. Le paure che insorgono possono essere determinate da stereotipi che spesso egli tende ad accettare e che lo portano a ritenersi incapace fino ad un lento declino intellettuale. Questa ricerca ha l'obiettivo di approfondire le conoscenze sulle paure dell’anziano ricoverato e sperimentare la “presenza dell’infermiere” come possibile intervento.
Materiali e Metodi: All'interno di un Reparto “Cure Intermedie” è stata svolta una ricerca qualitativa con osservazione partecipante (studio osservazionale descrittivo tipo “serie di casi”). I dati raccolti sono stati analizzati attraverso il metodo l’analisi del contenuto.
Risultati: Dalle osservazioni di 13 pazienti (9 donne e 4 uomini; età media 71 anni), sono emersi principalmente contenuti positivi come “Gioia (47)”, “Attesa (35)” e “Offerta-ricordo (33)”. Il contenuto "Paura (16)” diversamente dalla bibliografia consultata è risultato presente ma non preponderante.
Discussione: Dall’analisi approfondita del materiale pare emergere che gli aspetti negativi comprendenti la “Paura” sono tra loro molto collegati ma il grosso nucleo di sofferenza viene destabilizzato dagli aspetti affettivi (speranza, aspettativa, amore) che arriva ad una prospettiva positiva (gioia, piacere, gratitudine). “Ascolto” e “disponibilità” sono stati i principali interventi attuati durante l’osservazione e coerentemente a quanto descritto in letteratura hanno permesso di registrare un impatto positivo sui pazienti. Un approfondimento è stato dedicato al concetto di “Offrire-dono” inteso come atto di riconoscimento attivo da parte del paziente verso l’operatore, con le sue implicazioni simboliche e psicologiche. Nell’analisi del materiale sono anche stati presi in considerazione aspetti legati alla psicologia positiva e allo “human caring”, come l’importanza e l’effetto del sorriso, della presenza fisica, dell’empatia nella condivisione e i risvolti nell’ambito di cura.
In base agli indicatori della Diagnosi Infermieristica di Paura di Lynda Juall Carpenito-Moyet, la valutazione iniziale durante la fase di accertamento degli stati di paura del paziente, permette un'assistenza basata anche sulla pratica dell'ascolto, competenza fondamentale dell'infermiere. Nei pazienti valutati si è assistito ad una riduzione dello stato di paura nelle osservazioni successive e nelle stesse, ipotizzando un effetto efficace della “presenza”.
Parole Chiave: anziano; paura; presenza; gratitudine; human caring.
Fear in the Elderly
ABSTRACT
Introduction: Frailty in elderly is physical and psychological conditions which could negatively influence their life events. The fears that arise can be determined by stereotypes that the elderly often tend to accept and that lead them to consider themselves unable up to a slow intellectual decline. This research aims to deepen the description of the manifestations of fear in the elderly and “the presence of nurses” as a possible intervention.
Materials and Methods: A qualitative research with participant observation (descriptive study with case series) was carried out within an “Intermediate Care” Department. Data collected was analyzed using the content analysis method.
Results: From content analysis of the collected material, during the participatory observation of the 13 patients enrolled in this research (9 women and 4 men; mean age 71 years), mainly positive contents emerged: "Joy (47)", "Waiting (35)" and "Offer-memory (33)". The content "Fear (16)", unlike the bibliography consulted, was present but not preponderant.
Discussion: From the in-depth analysis of the material it seems to emerge that negative aspects including "Fear" are very closely linked but the large core of suffering is destabilized by the affective aspects (hope, expectation, love) that reaches a positive perspective (joy, pleasure, gratitude). "Listening" and "availability" were main interventions implemented during observation and consistently with what is described in the literature, they made it possible to record a positive impact on patients. An in-depth study was dedicated to the concept of "Offering-gift" understood as an act of active recognition by the patient towards the operator, with its symbolic and psychological implications. In the analysis of the material, aspects related to positive psychology and "human caring" were also taken into consideration, such as the importance and effect of smiling, physical presence, empathy in sharing and the implications in the area of care.
Based on the indicators of Lynda Juall Carpenito-Moyet's Nursing Diagnosis of Fear, the initial assessment during the assessment phase of the patient's states of fear, allows assistance based also on the practice of listening, a fundamental nursing competence. In the patients evaluated there was a reduction in the fear, in the subsequent observations and in the same, hypothesizing an effective effect of "presence".
Keywords: elderly; fear; presence; gratitude; human caring.
INTRODUZIONE
“Uscendo dalla stanza ripenso alla sua risposta, al fatto di aver dichiarato di aver avuto paura e di averlo negato in un secondo momento quando gli è stato chiesto in maniera diretta.” (Paziente 3, osservazione 1)
“Saluto S. e lo ringrazio per le sue parole. Mi sento piccola davanti a tanta sofferenza che ha provato S. e che continua a provare. Credo che dovremmo amare la vita ed ogni singolo giorno perché purtroppo c’è chi ha avuto la sfortuna di avere meno di noi e che soffre in silenzio. Questa chiacchierata con S. mi ha lasciato un mix di emozioni, inizialmente un po' di distacco davanti ad una persona molto espansiva ed io molto più chiusa, poi interesse nelle sue parole, dispiacere, gioia allo stesso tempo nel vedere tanta vita in una persona che soffre così tanto. Incontrare persone con un grande bagaglio così, ci fa sentire tanto piccoli.” (Paziente 4, osservazione 1)
La dichiarazione e poi la negazione della paura da parte del paziente fanno pensare ad una sopraffazione della realtà. Molte volte avvertendo un sentimento forte, come la paura, è l’imbarazzo del proprio giudizio che può portare alla negazione.
Gli eventi negativi nella vita dell’anziano, come la presenza di malattie, morte del partner o dei familiari, povertà, rappresentano un peso sul piano dell’esperienza affettiva e sono inevitabili solitudine, dolore e paura della morte [1–3]. Le conseguenze a livello psicologico delle patologie che possono affliggere la persona anziana, diventano evidenti durante il ricovero nell’ambiente estraneo – ospedaliero [4]. Le capacità intellettuali subiscono dei cambiamenti nell’età senile le quali possono impedire di adattarsi velocemente a situazioni nuove [5]. Molte situazioni provocano sentimenti di paura e spesso tali sentimenti causano conseguenze negli esiti della cura delle patologie con le quali interagiscono [6], il sentimento di sicurezza è un aspetto che necessita di essere curato nell’assistenza [7,8].
Le persone anziane si avvicinano al concetto della paura di morire, data anche dalla presenza di patologie che tendono ad aumentare questo sentimento e spesso rimane difficile per loro affrontare questo argomento [9]. La paura è amplificata anche dall’ambiente ospedaliero, diverso rispetto a quello nel quale la persona solitamente vive, poiché nel nuovo ambiente mancano gli oggetti personali, tutti possono entrare senza bussare ed essa si sente privata della sua libertà. “Il trasferimento di abitazione è considerato un evento stressante a tutte le età e lo è a maggior ragione per i soggetti anziani” [1,4,10]. La comparsa della paura può influire sul benessere psicologico dell'intera persona. Molte volte l'anziano teme di essere inadeguato al contesto e l'operatore che lo percepisce, tende ad allontanarsi creando un distacco o sviluppando ostacoli per una buona relazione. Così facendo si creano degli ostacoli nella relazione che possono incidere sulla qualità dell'assistenza erogata [6].
Obiettivo dello studio
Lo scopo di questa ricerca è stato dunque di approfondire alcuni aspetti della paura nell’anziano e verificare se la “presenza” dell’infermiere è un intervento efficace a ridurre la sensazione di paura.
MATERIALI E METODI
Procedure
Lo studio è iniziato a fine settembre 2017 ed è durato un mese con una cadenza di due/tre sessioni di osservazioni a settimana. Le osservazioni sono state svolte da una studente di infermieristica dopo una preparazione di base alle relazioni di cura infermieristica [11] e sotto la supervisione di due infermieri esperti. Nella Figura 1 è riportata la successione cronologica delle fasi della ricerca. Su richiesta del personale sono state inserite nel campione di studio anche tre persone con età inferiore a 65 anni, identificati come portatori di “problemi relazionali”. I pazienti che hanno manifestato rifiuto alla partecipazione nello studio o alla firma del consenso dati sono stati esclusi dallo studio. Prima di iniziare la ricerca è stato richiesto e ottenuto il parere favorevole della “S.O.S. Etica e cura” della Azienda USL Toscana Centro (rilasciato in data 14.09.2017) e tutti i dati sono stati resi anonimi per garantire la privacy.
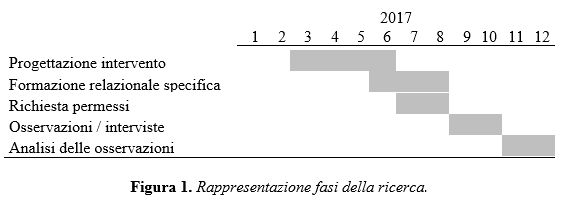
Nella seconda fase sono stati svolti due o tre incontri di osservazione partecipante dei pazienti: sono stati riportati su un diario anche gli indicatori relativi alla diagnosi di paura in collaborazione col personale di reparto. Ad ogni incontro l’osservatore entrava nella stanza dei pazienti selezionati, accompagnato da un operatore del reparto (oss / infermiere) o in modo autonomo; dopo la presentazione veniva spiegato il motivo della ricerca e chiesto la firma per il consenso. Successivamente l’osservatore si tratteneva nella stanza del paziente per compiere le osservazioni che venivano riportate su un diario per un periodo di osservazione di circa 30 minuti: in tale situazione di osservazione partecipe l’osservatore se interrogato o coinvolto dava il suo contributo per evitare una situazione asettica di osservazione. Nel limite del possibile sono state riportate frasi o parole che in seguito sono state sottoposte al processo di analisi; nei casi in cui la redazione delle osservazioni avrebbe compromesso la serenità del setting la trascrizione è avvenuto dopo il periodo di osservazione.
Nella terza fase è stata svolta l’analisi dei dati raccolti assegnando dei codici ad ogni frase o gesto espresso e/o manifestato dai pazienti. Dopo una razionalizzazione dei codici emersi, l’analisi è proseguita attraverso un raggruppamento dei codici tramite “categorie” e lo studio di tabelle e grafici [12].
Popolazione di studio
Lo studio condotto è stato rivolto alla popolazione anziana, ricoverata in strutture sanitarie. La ricerca è stata svolta su un campione di pazienti anziani (età media 71 anni) provenienti da reparti di medicina e ricoverati in una unità di “Cure intermedie”. L’inclusione dei pazienti nello studio è stata svolta da parte del personale infermieristico del reparto, sulla base di una diagnosi infermieristica di “Paura” [13] secondo una modalità di comodo compatibile con le attività istituzionali della struttura ospitante. Nella ricerca sono stati inclusi 13 pazienti, 9 donne e 4 uomini con età superiore o uguale ai 65 anni, con l’eccezione di 3 pazienti che hanno costituito un nucleo di confronto sui dati rilevati (considerando il gruppo di confronto, il gruppo di ricerca ha avuto un’età media di 75 anni). Tutti i pazienti che sono inclusi in questo studio avevano letto, capito e firmato il consenso informato, per coloro che non erano in grado è stato fatto riferimento ai rispettivi caregiver; tutti i dati sono stati resi anonimi; per la partecipazione allo studio non sono stati distribuiti incentivi.
Criteri di inclusione
- età uguale o superiore ai 65 anni;
- Comprensione e firma del consenso informato.
- Un eventuale stato di confusione è stato considerato inseparabile dalla situazione complessa correlata alla paura (per le persone in stato di confusione è stato richiesto il consenso ai propri caregiver).
Criteri di esclusione
- Volontà a non voler partecipare allo studio.
- Impossibilità di far comprendere all’assistito o ai familiari i motivi dello studio.
Strumenti
Per esplorare gli aspetti legati alla paura è stata ideata una ricerca-intervento [14], basata su osservazione partecipante. La rilevazione dei dati è avvenuta attraverso un diario nel quale sono stati descritti gli incontri con frasi dette dai pazienti, dall’osservatore, dai familiari, dagli operatori, anche decifrando le espressioni sul volto dei pazienti stessi. Il report delle osservazioni e interazioni ha costituito il testo base su cui sono state svolte le analisi.
Per la valutazione del livello di paura invece è stata effettuata attraverso le caratteristiche definenti la diagnosi infermieristica di “Paura” [13] e l’attribuzione di un punteggio (0-nessuna, 1-lieve, 2-moderata o 3-elevata). Con la collaborazione del personale di reparto è stato riportato lo stato del paziente rispetto al primo incontro (vedere Tabella 1).
La modalità di osservazione, che prevedeva una disponibilità al colloquio durante i momenti di osservazione sul campo ha reso sicuramente meno obiettiva l’osservazione ma è stata scelta per rendere l’ambiente maggiormente confidenziale e garantire l’agiatezza ai partecipanti.
Analisi qualitativa
La prospettiva teoria considerata alla base dell’analisi svolta si ispira al modello di “grounded theory” [15]; l’analisi sul testo prodotto attraverso i diari delle osservazioni è stata una analisi del contenuto quantitativa [12]. Per l’analisi qualitativa è stata utilizzata una Analisi Qualitativa Computer Assistita (CAQDAS - computer assisted qualitative data analysis software) tramite “R” (16) ed in particolare il modulo “RQDA” [17]. I dati sono presentati tramite una condensazione in tabella e una rappresentazione tramite diagramma network (basato sulla teoria dei grafi). L’analisi qualitativa non si è posta l’obiettivo della completa saturazione dei dati a favore di una maggiore realizzabilità in tempi relativamente brevi della ricerca, comprendendo che una semplificazione del genere non orienta verso dati certi ma almeno la dichiarazione di dati fondati, sui quali confrontare alcuni aspetti dell’assistenza (in particolare l’effetto della presenza).
RISULTATI
Nella tabella 1 sono riportate le caratteristiche del campione analizzato: 9 partecipanti di sesso femminile e 4 di sesso maschile; l’età media del campione è stata 71 anni. Sono state svolte 3 sessioni di osservazione per 2 partecipanti, 2 sessioni per 5 partecipanti e una unica sessione per i rimanenti 6 partecipanti. Nella stessa tabella è riportata la riduzione dello stato di paura avvenuto in 6 casi, ovvero il suo mantenimento in altri 6 casi (di cui 2 risultavano già al grado minimo quando è stata svolta l’osservazione) e l’unico caso in cui si è assistito ad una comparsa dove era assente.
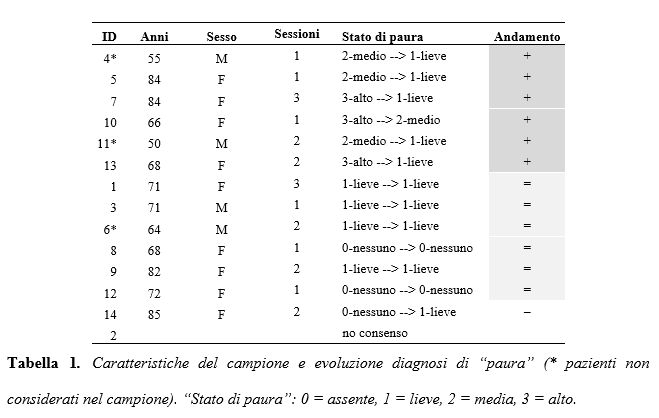
Nella Tabella 2 e nella Figura 2 sono riportati codici e frequenze. “Gioia-felicità” è il codice che appare più volte rispetto a tutti gli altri (47 volte). Seguono: “Attesa” (35 volte), “Offerta-ricordo” (33 volte), “Preoccupazione” (29 volte), “Gratitudine” (23 volte). Il codice “Paura” compare solo 16 volte.
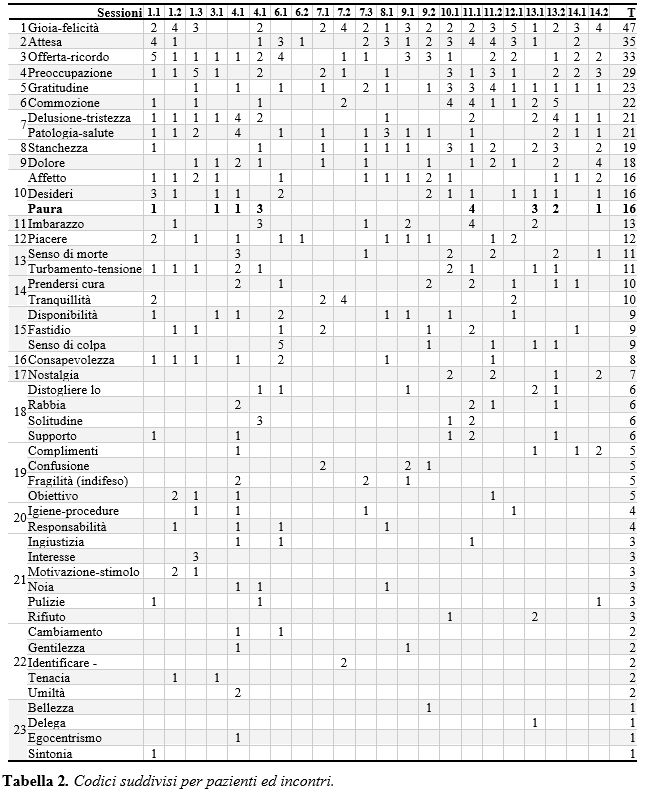
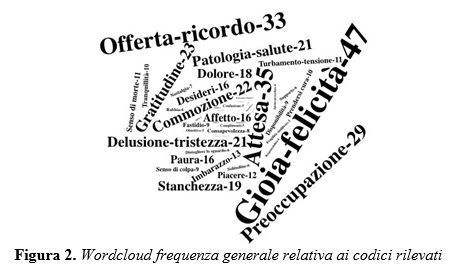
Nella Figura 3 può essere osservato il diagramma network risultato dall’analisi del materiale raccolto. In minuscolo vengono riportati i codici attribuiti durante l’analisi, in maiuscolo le “categorie”, costruzioni dotate di maggiore astrazione.
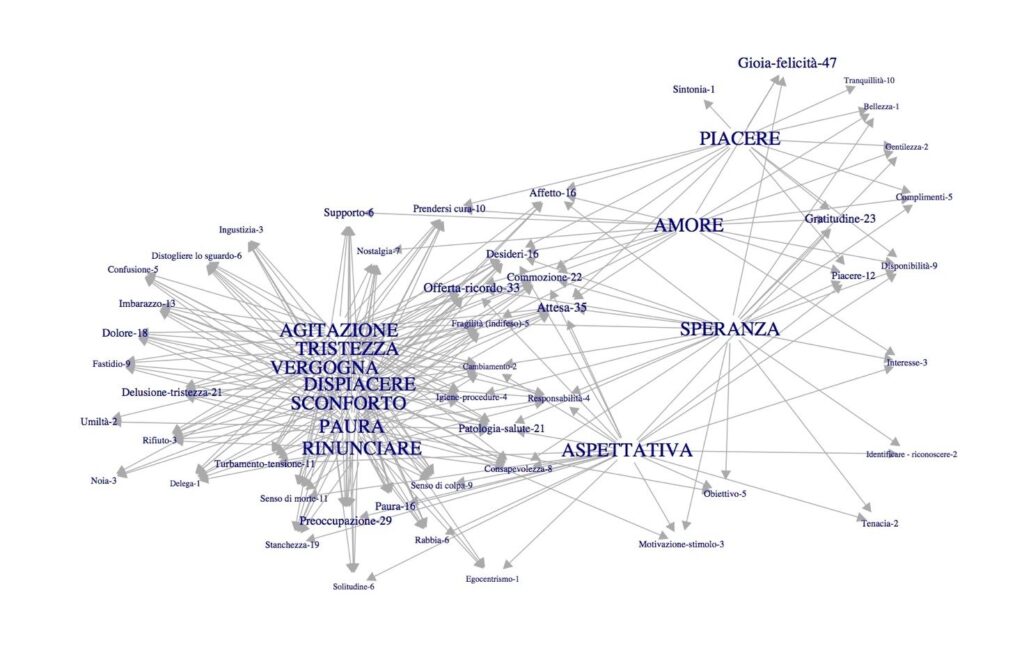
Figura 3. Diagramma network. Relazioni tra codici e categorie (riportate in maiuscolo).
La parte centrale del grafico riporta i codici con molte interazioni quindi più coinvolti nell’oggetto di studio; possono essere notati codici quali: “Offerta-ricordo”, “Fragilità(indifeso)”, “Supporto”, “Attesa”, “Desiderio”, “Cambiamento”, “Patologia”, “Salute”, “Consapevolezza”.
Il grafico è una chiara illustrazione del conflitto paura-stati-correlati versus speranza-amore-piacere, i costrutti sui quali agisce sono in rapporto maggiormente con “Patologia – salute”, “Igiene”, “procedure”, “Fragilità(indifeso)”, “offerta ricordo”, “Comunicazione”, “desideri” e “Affetto”.
Ulteriori temi emersi
Oltre a quelli riportati nella descrizione del diagramma, alcuni temi hanno richiamato una particolare attenzione e sono stati particolarmente stimolanti durante l’analisi del materiale.
Dono e Gratitudine
Questo tema ha messo in luce che pensare la cura come qualcosa che dal sanitario va verso il paziente ha un carattere limitato.
«Vuoi un budino?» Colpisce la semplicità del gesto: dovremmo essere noi a “dare” assistenza al paziente e invece è lei ad “offrire” qualcosa. (Paziente 06, osservazione 1)
«Sì, ho letto altre pagine, poco per volta. Poi te lo passo e lo leggi anche te!» (Paziente 09, osservazione 2)
Nella parte centrale del Grafico Network (Figura 3), emerge come centrale il codice “Offerta-ricordo”. Durante le sessioni di osservazione in quasi tutti i pazienti è emersa l’azione di offrire qualcosa: budini, caramelle, poesie, ricordi.
Paura
“Era la morte all’inizio la mia più grande paura...” (Paziente 13, osservazione 2)
Le emozioni sono strettamente correlate all’ambiente circostante o a quello che è interno alla persona. James dichiara che l’uomo non scappa perché ha paura, ma perché si accorge di averla ed ha già messo in atto il tentativo di fuga [1].
Alcune emozioni mostrano una connessione con paura (Figura 3): sfiducia per la paura dell’abbandono, rabbia per paura di non essere considerato, pregiudizio per paura del confronto, impotenza per la paura di fare, giudizio per paura dell’altro, senso di colpa per paura di aver sbagliato. Infelicità, tristezza e dolore richiamano emozioni negative che possono sovrapporsi con la paura. Tale vicinanza di concetti richiama anche il costrutto di “sindrome migratoria”, che si manifesta quando una persona si trova in un ambiente di vita estraneo [4]. Così potrebbe essere interpretata la sovrapposizione dei concetti negativi osservabile nel Diagramma Network (Figura 3). La paura di non essere amati risale alle cure parentali insieme alle quali veniva trasmesso l’amore. “Amore” è una categoria della parte positiva del Diagramma Network (si veda Figura 3).
Depersonalizzazione
“Ho durato fatica ad accettarlo, lì per lì ho sdrammatizzato con una delle mie solite battute, poi una volta da solo, ci ho riflettuto … non mi riconoscevo più all’inizio … è stata dura da digerire” (Paziente 4, osservazione 1).
La depersonalizzazione si caratterizza dal fatto che il paziente non si sente più la stessa persona che era prima del ricovero.
Contatto
In molte occasioni l’aspetto fisico è risultato centrale, una comunicazione oltre le parole.
“Le accarezzo la mano, mi sorride, le sorrido. Rimaniamo per un po' in silenzio” (Paziente 7, osservazione 2)
“Grazie tesoro, vieni qua, dammi la mano” è stato sufficiente stringere loro la mano, sorridendo in silenzio. Quella stretta ha permesso di comunicare oltre alle parole, l’emozione della “presenza”. (Paziente 14, osservazione 2)
Speranza
Dall’analisi dei dati emerge una categoria centrale nella parte positiva del Diagramma Network (Figura 3), la “Speranza”. Essa è correlata a ottimismo, in quanto si presenta come l’attesa di un esito gradito o al contrario come rimozione di un esito sgradito riguardo un evento futuro [5].
Emozioni Positive
“Mi ripete più volte che sta aspettando la nuora e non sa se avvertire il figlio che si è sentita male ma mi dice «non voglio dargli pensiero»” (Paziente 7, osservazione 1-Stato di paura: 3-elevato)
“Chiude nuovamente gli occhi e noto che respira a bocca aperta, le sue mani sono meno tese e la respirazione è meno accelerata rispetto a prima, forse inizia a rilassarsi un pò” (Paziente 7, osservazione 1-Stato di paura: 1-lieve) […] “Lei guarda davanti a sé in maniera fissa con la bocca leggermente aperta. E' tranquilla, ha una respirazione normale rispetto all'altro giorno” […] “Chiude gli occhi come se si stesse addormentando. Le braccia sempre distese lungo i fianchi, il respiro più profondo e lento. Dorme.” (Paziente 7, osservazione 2-Stato paura: 1-lieve)
Il codice più frequente è stato Gioia-felicità (47 volte). Attesa (N=35), Offerta-ricordo (N=33), Preoccupazione (N=29) e Gratitudine (N=23) sono termini che si evidenziano con maggior frequenza (Tabella 2).
Identificazione ed Empatia
"Sono stata con lei più del previsto, un po' perché ho dato modo alla nipote di stare con lei, un po' perché era piacevole parlare della sua vita, dei suoi ricordi, decido di salutarla per dare spazio anche ad un altro paziente. Sono contenta di questo incontro, di essere entrata in sintonia con lei, il fatto che mi abbia chiamata con un soprannome, credo che ciò sia positivo.” (Paziente 1, osservazione 1)
“Sono stati 20 minuti passati molto velocemente e mi ha fatto piacere aver rivisto R., mi interessa ascoltarla e sono contenta dei progressi che ha fatto in questi giorni. R. ha tanto bisogno di avere qualcuno vicino col quale poter parlare.” (Paziente 1, osservazione 2)
“Sono contenta di aver passato tre giorni con R., di averla ascoltata, delle belle parole ricevute. Nonostante come da lei riferito, qui in reparto abbia trovato dei bravi operatori, lontani dalla famiglia avvertiamo sempre qualcosa che ci manca; sono contenta che R. ritorni a casa con la figlia.” (Paziente 1, osservazione 3)
Durante le interviste si sono manifestate nell’osservatore emozioni, soprattutto legate alla gioia, ma anche di tristezza e di nostalgia alle quali si è sentito il bisogno di rispondere con un sorriso. Il sorriso è risultato essere fondamentale per entrare in sintonia con l’altra persona, guardarla negli occhi per cercare di lasciare un ricordo piacevole. Al “sorriso” la paziente rispondeva con un ulteriore sorriso che ha alimentato una spirale positiva.
DISCUSSIONE
Il ricovero sembra effettivamente costituire un evento che mette a rischio l’equilibrio della persona anziana, costituisce quindi, di per sé, una causa di paura:
“Mi dice di continuo di non farcela più e piange” (Paziente 10, osservazione 1)
“Ho tanta paura … non ne posso più ...” (Paziente 12, osservazione 1)
Naturalmente la paura della morte è una delle più importanti anche se nel materiale raccolto non sembra essere l’unica; altre paure espresse riguardavano: perdere un arto, di sentirsi male e fare male ad altri, di essere a carico familiare, l’incertezza, di non essere più la solita persona, l'ambiente ospedaliero, gli operatori e le loro divise, le procedure di routine, di essere truffata. Tutte paure connesse con lo stato di fragilità.
Il modello espresso dal diagramma network (Figura 3), condensato del lavoro di ricerca svolto, mostra una struttura che vede da un lato la paura collegata ad altri concetti quasi del tutto sovrapponibili dal punto di vista delle connessioni (sconforto, dispiacere, vergogna, tristezza, rinuncia e agitazione) come a formare un costrutto che sembra richiamare la “sindrome migratoria” [4]; dall’altro lato le reazioni di speranza, aspettativa che arrivano fino ad amore e piacere. Le reazioni che hanno sorpreso maggiormente e attratto l’attenzione dei ricercatori sono state appunto quelle relative al piacere, uno stato d’animo sicuramente inatteso, soprattutto perché la selezione dei pazienti è avvenuta sulla base della diagnosi di paura. La sindrome migratoria accennata può facilmente trovare spiegazione nella situazione “estranea” rappresentata dall’ambiente ospedaliero, ma per la parte orientata alla salute (fino al piacere) sembra necessario il ricorso ad una teoria infermieristica che permetta di includere la crescita personale del paziente all’interno degli obiettivi di cura, intendendo l’assistenza infermieristica come strumento per lo sviluppo e il benessere [18,19] e non solo come mezzo assistenziale di supporto. La funzione della assistenza infermieristica in questo senso è quella di “contenere” sia le categorie collegate alla paura sia quelle collegate alla speranza tramite aspetti tipici della professione quali patologia-salute, igiene, procedure.
Partendo dalla rilevazione della maggiore frequenza riscontrata dai codici gioia-felicità, attesa e offerta-ricordo, che riflettono un clima sorprendentemente positivo, i contenuti riportati sotto il codice offerta-ricordo costringono, anche per la loro posizione di centralità nel modello, ad una riflessione. Una possibile spiegazione che è stata posta riguardo a tale risultato di emotività positiva è in relazione con lo “stile” utilizzato per la ricerca: l’intervistatore-osservatore ha svolto delle osservazioni utilizzando una modalità improntata alla gentilezza [19], all’ascolto non direttivo [20] e non in modo asettico (non interagire avrebbe introdotto una variabile “spersonalizzante”).
La diagnosi di “paura” si è ridotta in tutte le diagnosi di paura media / alta e rimasta stabile nei casi lievi / assente (Tabella 1). Solo in un caso è aumentata da assente a lieve durante l’osservazione. La sintesi è che nel campione osservato prevalgono sentimenti di gioia, attesa e la volontà di offrire qualcosa all’operatore, mentre paura compare solo al decimo posto in ordine di frequenza, almeno questo è accaduto nell’ambiente di osservazione attenta realizzato dal dispositivo della ricerca-intervento [14] attuata. Il tema del dono ha portato il coinvolgimento al centro dell’attenzione: accettare o rifiutare? Ovviamente accettare o rifiutare si estende dal dono al paziente e in questo ambito anche un gentile rifiuto costituisce comunque un rifiuto, ma accettare significa diventare “debitori” verso il paziente: il dono è un elemento fondamentale per la nascita dei rapporti sociali e delle comunità umane, in quanto esprime la volontà degli uomini di “creare relazioni”, le quali hanno come conseguenza l'obbligo della restituzione [21]: ad anche l’operatore che si ferma al letto di un paziente per ascoltarlo, gli “dona” il suo tempo e non lo fa in modo gratuito poiché in un certo senso spera di avere in cambio, come restituzione del suo ascolto, un appagamento personale per aver fatto confidare e liberare il paziente dalle preoccupazioni che lo turbavano [22]. Il ricevente si sente obbligato a restituire qualcosa che ha ricevuto.
“Mi ha fatto piacere conoscerti, ti ringrazio tanto tanto!” (Paziente 13, osservazione 2) la frase del paziente, in questo caso, ha trasmesso all’osservatore il senso di gratitudine per l’ascolto che le era stato dedicato.
Donando e ricevendo si innesca una spirale di riconoscenza e in effetti la maggior parte dei pazienti del presente studio ha manifestato la gratitudine.
«Grazie tesoro, vieni qua, dammi la mano!» (Paziente 14, osservazione 2)
«Grazie...», Mi prende la mano e la stringe portandola verso la sua guancia... (Paziente 13, osservazione 2)
In questa frase è possibile notare la manifestazione di emozioni controverse: gratitudine verso chi dona, ma anche imbarazzo poiché a questo punto la persona è debitrice nei suoi confronti, si crea dunque uno squilibrio, uno stato di debito, definito da Hochschild “economia della gratitudine” nella quale ogni ricevente è grato al donatore [9].
“Mi avvicino, l’abbraccio e piange” (Paziente 13, osservazione 2)
E’ proprio dalla gratitudine verso il dono ricevuto che può scaturire il pianto nel momento degli abbracci e dei saluti [23]. A proposito di “Gratitudine”, Esopo riteneva: “la gratitudine come segno di anime nobili”, mentre per Cicerone serviva per mantenere l’amicizia ed una giusta società, per Adam Smith rappresenta una delle emozioni di base nella società [22]. Secondo Klein la gratitudine nasce nell'infanzia [1,24], già nei primi scambi relazionali madre-bambino attraverso l’allattamento al seno. Se quest’ultimo viene sottoposto a frustrazioni, proietta sul seno della madre degli impulsi aggressivi e sarà più difficile provare gioia e gratitudine: frustrazione, gioia e gratitudine sono temi sicuramente presenti nei luoghi di degenza. Determinati atti di gratitudine sono in grado di trasmettere a chi li riceve la capacità di offrirne a sua volta, poiché la presenza di feedback positivi da parte di chi riceve, come un abbraccio, un sorriso, permette di rinforzare le motivazioni del donatore. Durante l’osservazione si è creata una spirale di “gentilezza amorevole” [19]: è possibile fare l’ipotesi che questa sia responsabile dei contenuti di gioia, molto frequenti, che sono stati rilevati.
Naturalmente le osservazioni di fenomeni ansiosi e di sofferenza non sono state poche: il codice preoccupazione al 4° posto, delusione-tristezza al 7°, stanchezza 8°, dolore al 9° e paura al 10° (Tabella 2) ne danno piena testimonianza.
La persona sofferente, tende a fuggire:
“Mi dice di continuo di non farcela più e piange” (Paziente 10, osservazione 1)
Ascoltare la persona che soffre, si è dimostrato un intervento utile ad alleviare il suo dolore.
“Dice di non sapere, poi si convince a parlare. Dal colloquio è emersa tutta la sua sofferenza, una sofferenza che, in un primo momento, era stata mascherata […] è bastato sedersi vicino, ed essa si è liberata di un peso che si portava dentro da molto tempo: una serie di lutti di persone a lei care, il marito, la figlia, si sente sola e trova difficoltà nel pensare al futuro, poiché ha dubbi sulla sua guarigione. «è dura […] sono sola»; mi dice di continuo di non farcela più e piange. Agli operatori si era presentata come la più sorridente del reparto (Paziente 10, osservazione 1. Scala paura iniziale = 3, post intervento = 2).
“I drammi più commoventi e più strani non si svolgono a teatro, ma nel cuore di uomini e donne comuni. Questi vivono senza attirare l’attenzione e non tradiscono minimamente i conflitti che imperversano nel loro animo” [25].
Secondo Nhat Hanh, lo scopo della pratica dell’ascolto compassionevole consiste nel permettere alla persona di esprimersi, senza interromperlo o correggerlo, diminuendo così il suo dolore [26].
“Ma, tornerò a casa?” (Paziente 10, osservazione 1)
Il dolore a volte accresce per paura dell’ignoto, ma l’uomo finge di stare bene perché non ama provare solitudine, rabbia o paura. Spesso sono i forti desideri che egli ha ad ostacolare la sua felicità, permettendo così alle emozioni negative di accumularsi. Quando una persona è malata, essa desidera che sia fatto qualcosa per lei e la sensazione di essere curata aumenta le aspettative di guarigione riducendo ansia e depressione connesse all’essere malati [27]. Molte volte viene applicato l’effetto placebo per diminuire uno stato di dolore, di ansia, ma anche la capacità di trasformare la sofferenza in emozioni positive è di grande aiuto.
La guarigione non è solo un placebo, essa condensa l’effetto dell’ambiente, della fiducia e della cura, gli “atti sacri infermieristici”, un contatto profondo dell’essere che avviene alla presenza di un infermiere, supporto e testimone [8,19].
Senza la sofferenza non ci sarebbe la felicità; se la persona è in grado di riconoscere il dolore, allora sarà in grado di riconoscere anche la gioia. La sofferenza del corpo è determinata dal dolore, dalla fame, dalla malattia e dalle lesioni fisiche, invece il tormento della mente è caratterizzato dalla presenza di ansia, gelosia, disperazione, paura e rabbia [26]. Possono coesistere entrambi i due tipi di sofferenza provocando tensione e stress ed è grazie alla consapevolezza che l’uomo è in grado di riconoscerla: «Appena apriamo la bocca per dire sofferenza, sappiamo che nello stesso momento è già presente anche l’opposto della sofferenza. Dove c’è sofferenza, c’è felicità» [28].
“Inspirando, so che la sofferenza è presente. Espirando, saluto la mia sofferenza” [26], un paziente agitato, per essere calmato, viene invitato a respirare lentamente e pian piano il suo turbamento, la sua sofferenza in quel momento si placa lentamente.
L’atteggiamento positivo è sempre benefico e per superare la paura è necessario informarsi sulla malattia, ottimismo e speranza inoltre possono essere trasmesse al paziente dalle persone che lo circondano. “L’ottimismo è la fede che porta al risultato. Senza speranza né fiducia, non si può fare niente.” (Helen Keller), fattori fondamentali per la guarigione e la sopravvivenza del paziente, che non possono essere misurati scientificamente, ma nemmeno ignorati [29], “l’ottimismo sembra avere effetti positivi sulla salute anche in situazioni particolarmente delicate” [30].
“Anche se nella stanza c’è il buio, tu mi porti la luce col tuo sorriso” (Paziente 1, osservazione 3)
“Proprio una bella persona, complimenti per il sorriso” (Paziente 4, osservazione 1)
In queste frasi comuni, troppo poco considerate, si manifestano le indicazioni per comportamenti che il paziente sente di accudimento.
Se la persona pensa di non essere amata abbastanza, è esposta maggiormente alla paura della mancanza di amore. “Il riso, è in alcuni casi, una risorsa vitale che cura, previene, riabilita, educa e libera dalla paura restituendoci una consapevolezza più ampia della nostra esistenza” [23] oltre ad avere documentati effetti terapeutici [31].
In ultimo, si vogliono riportare gli aspetti emotivi di coinvolgimento che seguendo le prospettive teoriche legate alla presenza autentica [19] rappresentano un importante fattore curativo:
“Anche se ripete le solite cose, mi fa piacere stare con lei, provo tanta tenerezza ad ascoltarla. Quei capelli grigi e bianchi sono il segno del tempo che passa, così come la sua memoria è segno del tempo che scorre.” (Paziente 9, osservazione 1)
La tristezza spesso sembra essere l’aspetto più intenso nella comunicazione del paziente, il perdere le cose importanti e dare importanza a cose inutili che spinge a riflettere sulle cose veramente importanti della vita: il grande tema del significato. Ascoltare, anche il silenzio, ha fatto emergere emozioni e riflessioni che potrebbero essere utili alla crescita di ogni operatore.
“Rimango commossa uscendo dalla stanza. È incredibile come un piccolo gesto, una piccola parola di conforto possa far sentire meno sola una persona. È brutto pensare a quanta solitudine e sofferenza possano esistere in una persona.” (Paziente 10, osservazione 1)
“Mi sono sentita in imbarazzo a sentire parlare così suo figlio...mi viene da pensare che quell’inizio di depressione, forse non sia dovuto soltanto alle patologie della signora N., ma anche ad un suo stato emotivo determinato dalle circostanze nelle quali si ritrova. Sono rimasta un po' turbata da questa scena...magari è soltanto un’impressione, ma sembra che N. dipenda molto dal figlio, non tanto per spostarsi dal letto alla sedia, bensì nelle parole.” (Paziente 13, osservazione 1)
Tenerezza, senso di protezione che diventa rabbia per la ridotta considerazione nel paziente hanno caratterizzato molti momenti dell’osservazione. La tenerezza, legata allo stato di fragilità ha anche sostenuto la gran parte degli interventi di ascolto e presenza-vicinanza che sono stati attuati durante l’osservazione.
Conclusioni
Le paure che insorgono nell'anziano possono essere determinate da stereotipi come ad esempio che esso diventi dipendente da un'altra persona. Questi pregiudizi possono portare la persona anziana a ritenersi inutile, malato, priva d’idee e di interessi. A volte gli anziani tendono ad accettare questi stereotipi negativi che li portano a ritenersi incapaci fino ad un lento declino intellettuale. Per invecchiare bene è necessario seguire una buona alimentazione ed esercizio fisico, ma è fondamentale anche mantenere delle relazioni sociali basate su amicizia ed amore per evitare la comparsa di solitudine.
La domanda di ricerca iniziale si proponeva di individuare se l’infermiere durante la fase di accertamento, individuando la paura nell’anziano, può aiutarlo a superarla appena si manifesta; se la “presenza” in particolare potesse essere un intervento efficace a garantire un buon percorso di assistenza. La “presenza” è un fattore di cura capace di produrre cambiamenti di per sé. Le categorie SPERANZA, AMORE, PIACERE, sono risultate l’antidoto.
Differentemente da quanto atteso, in questo studio, il codice paura non è risultato frequente quanto ipotizzato, ma è addirittura stato superato dal codice gioia-felicità. Sulla base dei dati raccolti e delle riflessioni presentate nel capitolo precedente è possibile ipotizzare che per una parte sia stata proprio la sua presenza dell’osservatore, come figura esterna al reparto nel quale si è presentato senza indossare la divisa, proprio per evitare un distacco col paziente dato dalla “paura del camice bianco” e che, per la parte partecipe, si è coinvolto emotivamente e deliberatamente nelle relazioni con i pazienti. Relativamente agli interventi, quelli codificati come modalità di osservazione partecipe, cioè ascolto attento, riformulazione, presenza emotiva espressa anche con gesti di contatto fisico, così come descritti dalla letteratura consultata, si sono dimostrati utili e coerenti con la riduzione della sensazione di paura o di preoccupazione. Come affiora dall’analisi dei dati nella popolazione osservata, sono presenti aspetti negativi quali paure e preoccupazioni, ma la relazione efficace di ascolto ha permesso ai pazienti di far emergere maggiormente le loro emozioni positive, poiché è stato permesso loro di esprimersi, senza interruzioni o correzioni, diminuendo così le loro ansie.
Rispetto agli indicatori forniti dalla diagnosi infermieristica di “paura”, l’osservazione partecipe, utilizzando le tecniche descritte è risultata efficace nella riduzione della paura in tutti i pazienti gli stati iniziali nei quali era presente anche una minima paura, quest’ultima è migliorata con , con diagnosi di paura media o alta, senza effetto nei casi di paura lieve o assente e solo in un caso ha registrato il passaggio da assente a lieve.
Anche l’atteggiamento ottimistico è stato preso in considerazione come strumento terapeutico: “Essere ottimisti non vuol dire essere rassegnati o negare che esistano le malattie, ma ricercare e inseguire il lato buono di tutte le situazioni convinti che esiste”, per affrontare meglio l’età senile, l’accettazione di quest’ultima, non deve arrestare la vita della persona, ma bensì indirizzarla verso nuove aspettative [32].
Tipi Di Paure
Benché non rientrasse negli scopi di questa ricerca l’esplorazione dei differenti tipi di paura manifestati dai partecipanti durante l’osservazione, le paure più frequentemente espresse riguardavano: la paura di perdere un arto, di sentirsi male e fare male ad altri, “di essere a carico familiare … di avere un futuro incerto, paura di non essere più la solita persona”, “dall’ambiente ospedaliero, dagli operatori e le loro divise, dalle procedure di routine”, di non trovare più lavoro, di morire, di essere stata truffata. L’alterazione del concetto di sé, l’ambiente ospedaliero, la perdita di autonomia, sembrano le diagnosi infermieristiche [4] che si correlano maggiormente con l’esperienza di paura dei pazienti osservati.
Human Caring E Relazione D’aiuto
Per la spiegazione degli effetti registrati di riduzione della paura, ma anche di sviluppo di un senso di piacere all’interno dell’esperienza di ricovero, è stato necessario ricorrere ad una teoria infermieristica che consideri la possibilità di facilitare ed attivare il processo di guarigione attraverso la “presenza”: «spostare l’attenzione dalla malattia, dalla diagnosi e dal trattamento al prendersi cura umano, alla guarigione e alla promozione della salute spirituale potenzia la salute stessa, la guarigione e la trascendenza (…). La relazione umana transpersonale ha una dimensione spirituale... che può sfociare nella guarigione». La presa in carico della persona rappresenta un momento delicato, fatto di amore e di una visione globale dell’esistenza umana. Infermiere e paziente determinano insieme la relazione scegliendo quale uso fare di quel momento nel tempo e nello spazio. Il modo in cui l’infermiere si relaziona avrà un impatto significativo sulle opportunità immediate e sui risultati finali [11,19,29]. SPERANZA, PRESENZA e GRATITUDINE sono i contenuti emersi in opposizione a PAURA, nelle sue varie forme.
LIMITI DELLO STUDIO
Questa ricerca qualitativa è basata sull’osservazione partecipante di un gruppo ristretto di pazienti, 13 in tutto, ricoverati nel Reparto Cure Intermedie, nei quali il metodo applicato è risultato efficace nella riduzione dell’intensità del livello di paura (Tabella 1), ma non vi è la certezza che esso sia applicabile a tutta la popolazione. Soprattutto non è stato possibile raggiungere la saturazione delle osservazioni, proseguendo l’attività di ricerca, le definizioni delle categorie in particolare avrebbero necessitato di ulteriori osservazioni per verificarne la saturazione. Un limite è dato dal fatto che non è stato possibile seguire tutti i pazienti più di una volta, poiché spesso la dimissione avveniva prima del tempo previsto. Un altro limite è dato dalla difficoltà di reperire l’argomento paura, nella produzione scientifica a fronte della facilità di reperimento nella bibliografia umanistica ed esistenziale: la maggior parte degli studi riporta la “paura di cadere”, la “paura di morire” o la “paura nel bambino”; minori quelli sugli aspetti esistenziali della paura o di un senso di paura diffuso nell’esperienza di ricovero dell’anziano.
Una limitazione non prevista è stata creata dal non aver misurato in modo preventivo tutte le emozioni ma solo l’intensità della paura perché non previsto dall’ipotesi iniziale: mentre la presenza e la prevalenza sugli altri costrutti è emersa dall’analisi del contenuto delle frasi raccolte, l’aumento di gioia-felicità è stato inferito sulla base dei resoconti del ricercatore.
Analisi riflessiva
Questa ricerca testimonia il valore della tecnica dell’osservazione partecipe, tramite l’ascolto attento, la riformulazione e la presenza emotiva per ridurre la sensazione di paura o di preoccupazione e tramite la relazione efficace di ascolto, per permettere ai pazienti di far emergere maggiormente le loro emozioni positive. Anche la variabile legata al colore delle divise potrebbe essere oggetto di sperimentazione per valutare se possa contribuire ad un miglioramento dell’umore anche nelle persone anziane [33]. Le competenze ontologiche, nella. Parte relazionale dell’assistenza, sono state il fondamento dell’approccio utilizzato con i pazienti [19].
Un approfondimento dello studio potrebbe essere svolto sull’effetto della divisa (o di una divisa colorata) sulla risposta emotiva che si otterrebbe dai pazienti. L’osservatore avrebbe inoltre cercato di accettare maggiormente ed approfondire gli “Offerta-dono” materiali dei pazienti.
“Apprensione, incertezza, attesa, aspettative, paura delle novità, fanno a un paziente più male di ogni fatica”. (Florence Nightingale)
EVENTUALI FINANZIAMENTI
Questa ricerca non ha ricevuto nessuna forma di finanziamento
CONFLITTI DI INTERESSE
Gli autori dichiarano che non hanno conflitti di interesse associati a questo studio
BIBLIOGRAFIA
- Baroni MR. I processi psicologici dell’invecchiamento. Carocci editore; 2003.
- Mishra N, Mishra AK, Bidija M. A study on correlation between depression, fear of fall and quality of life in elderly individuals. Int J Res Med Sci. 2017;5(4):1456.
- Moreno RP, De La Fuenta Solana EI, Rico MA, Fernández LML. Death anxiety in institutionalized and non-institutionalized elderly people in Spain. Omega J Death Dying. 2008;58(1):61–76.
- Bianucci R, Charlier P, Perciaccante A, Lippi D, Appenzeller O. The “Ulysses syndrome”: An eponym identifies a psychosomatic disorder in modern migrants. Eur J Intern Med [Internet]. 2017;41:30–2. Available from: http://dx.doi.org/10.1016/j.ejim.2017.03.020
- Iandolo C. L’approccio umano al malato. Armando Editore; 1979.
- Lowey SE, Norton SA, Quinn JR, Quill TE. A Place to Get Worse: Perspectives on Avoiding Hospitalization from Patients with End-Stage Cardiopulmonary Disease. J Hosp Palliat Nurs. 2014;16(6):338–45.
- Wassenaar A, Schouten J, Schoonhoven L. Factors promoting intensive care patients’ perception of feeling safe: A systematic review. Int J Nurs Stud. 2014;51(2):261–73.
- Mottola A, Cefalo MG, Di Martino M, Continisio I. La percezione della Qualità di vita del paziente con scompenso cardiaco: indagine sul campo. NapoliSana Camp. 2018;3(2):13–24.
- Murdaca F. Paura d’invecchiare. Sovera edizioni; 2014.
- Besser A, Priel B. Attachment, depression, and fear of death in older adults: The roles of neediness and perceived availability of social support. Pers Individ Dif. 2008;44(8):1711–25.
- Giacomelli G, Bacherini S. La relazione con il paziente. Roma: Carocci; 2006.
- Losito G. L’analisi del contenuto nella ricerca sociale. FrancoAngeli; 1996.
- Carpenito Moyet LJ. Diagnosi Infermieristiche. Casa Editrice Ambrosiana; 2015.
- Lewin K. Teoria e sperimentazione in psicologia sociale. Bologna: Il Mulino; 1972.
- Glaser BG, Strauss AL. La Scoperata della Grounded Theory. Roma: Armando Editore; 2009.
- R-Core-Team. R: A Language and Environment for Statistical Computing [Internet]. Vienna, Austria: R Foundation for Statistical Computing; 2011. Available from: http://www.r-project.org/
- Ronggui H. R-based Qualitative Data Analysis (R package) [Internet]. 2012. Available from: http://rqda.r-forge.r-project.org/
- Peplau H. Rapporti Interpersonali nell’assistenza infermieristica. Padova: Summa; 1994.
- Watson J. Assistenza infermieristica: filosofia e scienza del caring. Torino: Casa editrice ambrosiana; 2013.
- Rogers C. La terapia centrata sul cliente. Firenze: Martinelli; 1994.
- Mauss M. Saggio sul dono. Piccola Biblioteca Einaudi; 1950.
- Farnetti P. Gratitudine, dono, perdono, spiritualità. Franco Angeli; 2016.
- Fioravanti S, Spina L. Anime con il naso rosso. Armando Editore; 2006.
- Klein M. Invidia e gratitudine. Psicoanali. Firenze: Martinelli; 1969.
- Bacchetta R. Effetti del sorriso e della gratitudine con l’applicazione della tecnica del campo GIA in pazienti operati in regime di one day surgery. Prof Inferm Umbria. 2013;21–5.
- Nhat Hanh T. Trasformare la sofferenza. Terranuova Edizioni; 2014.
- Bellani M. Psicologia medica. Armando Editore, editor. 1991.
- Monbourquette J. I lati nascosti della personalità. Come riconoscerli e accettarli. Edizioni Paoline; 2001.
- Pellegrini W. Le radici del futuro: Human caring. Edizioni Medico Scientifiche; 2010.
- Tenzin G, Goleman D. Le emozioni che fanno guarire. Oscar Mondadori; 2009.
- Behrouz S, Mazloom SR, Asgharipour N, Aghebati N, Reza H, Vashani B. The Effect of Humor Therapy on Relieving Quality and Fear of Pain in Elderly Residing Nursing Homes: A Randomized Clinical Trial. Adv Nurs Midwifery. 2019;28(3):53–61.
- De Angelis R. Paura d’invecchiare. Todi Saggistica; 1990.
- Meyer, Le divise colorate degli infermieri giovano ai piccoli malati. 2009; Available from: http://firenze.repubblica.it/dettaglio/meyer-le-divise-colorate-degli-infermierigiovano-ai-piccoli-malati/1612461
Il calo delle prestazioni assistenziali durante il lockdown da Covid-19 in Italia: revisione da Pubmed
Brusini A.1*, De Marco F. 2
- Infermiere in Medicina dello Sport, Ausl Modena
- Dottore magistrale in “Management Pubblico e dei Sistemi Socio Sanitari”
Corresponding author: Brusini A., infermiere in Medicina dello Sport presso Ausl di Modena, laureato magistrale in “Management dello Sport e delle Attività Motorie”
E-mail: antoniobrusini87@outlook.it,
Cita questo articolo
ABSTRACT
Introduzione: La pandemia da Covid-19 ha inevitabilmente avuto un impatto significativo sul nostro stile di vita, stravolgendo e mutando modalità di lavoro, tempo libero e abitudini quotidiane. La più grande e grave pandemia degli ultimi 100 anni ha messo in luce la fragilità dei sistemi sanitari di tutto il mondo. Questo in Italia ha determinato, oltre alle migliaia di morti causate dal virus, anche i “danni collaterali” dovuti al fermo dei ricoveri ospedalieri e delle prestazioni ambulatoriali per tutti gli altri malati.
Materiali e Metodi: Attraverso il motore di ricerca Pubmed, con filtro di ricerca la parola “lockdown” AND “Italy” e considerando il periodo di tempo tra l’01/02/2020 e il 6/11/2020, compaiono 591 risultati. Sono stati presi in considerazione esclusivamente gli articoli e le citazioni che contenessero dati ospedalieri riferiti al periodo gennaio - maggio 2020, per un confronto con lo stesso periodo del 2019
Analisi dei dati: Gli studi selezionati mostrano uniformemente in tutto il territorio italiano un calo di ingressi e di ricoveri per patologie diverse dal Covid-19. Su 40 studi presi in cosiderazione, solo una voce ha mostrato un aumento delle prestazioni rispetto all’anno precedente. Le prestazioni sono calate poiché, durante l’era del Coronavirus, si sono ridotte le risorse per tante patologie croniche e di urgenza e per la loro prevenzione, risorse che sono state invece destinate alla lotta al Coronavirus; inoltre sono calati gli accessi al Pronto Soccorso.
Conclusione: per evitare eventuali future riduzioni di prestazioni ospedaliere causa pandemia occorre trovare soluzioni alternative all’ospedale, come il potenziamento della prevenzione e della medicina nel territorio. Inoltre è indispensabile l’informazione alla cittadinanza su un uso adatto del Pronto Soccorso, anche se il calo di ricoveri per patologie a rischio vita è un chiaro segno di paura al servirsi di tale servizio in caso di emergenza.
Parole Chiave: Covid-19, Care, Lockdown
The reduction in welfare benefits during the lockdown from Covid-19: review by Pubmed
ABSTRACT
Introduction: The pandemic from Covid-19 has had a significant impact on our lifestyle, overwhelming and changing work modes, leisure and daily habits. The largest and most serious pandemic in the last 100 years has highlighted the health systems’s fragility around the world. In Italy, this has determined, in addition to the thousands of deaths caused by the virus, also the "collateral damage" due to the cessation of hospital admissions and outpatient services for all other patients.
Materials and Methods: Through the search engine Pubmed, with search filter the word "lockdown" AND “Italy”, and considering all the articles published from 01/02/2020 to 6/11/2020, have appeared 591 results. The articles and quotations that have been taken into account refer to the period January 2020 - May 2020 with data in the same period of 2019.
Discussion: The selected studies show uniformly throughout the Italian territory a decline in admissions and hospitalizations for diseases other than Covid-19. During the Coronavirus era not just performance has dropped, but also resources that have been reduced for many chronic and urgent diseases and for their prevention for being allocated to the fight against the Coronavirus; furthermore access to emergency room are decreased.
Conclusion: it is important to find alternative solutions to hospital to avoid any reductions in hospital services, it is necessary to strengthen preventive medicine and territorial medicine, with greater participation of general practitioners in the management of the chronic patient to avoid further relapses.
Keywords: Covid-19, Care, Lockdown
Introduzione
Al 24 gennaio 2021, la sindrome Sars Covid 2019 ha provocato 98280844 contagi e 2112750 morti accertati [1]. La pandemia ha avuto origine dalla regione di Wuhan, Cina, e si sparsa in tutto il mondo. Il virus provoca in alcuni soggetti sintomi lievi come mialgia e tosse, ma in soggetti a rischio può portare a una sindrome respiratoria acuta, fino alla morte [2]. Per questo salute ed economia sono legate a doppio filo. La pandemia da Covid-19 ha provocato 85418 morti in Italia al 27/01/2021 [3], con età media dei morti sopra gli 80 anni e con una stima del 66.3 % di tre o più gravi patologie preesistenti, ed ha inevitabilmente avuto un impatto significativo sullo stile di vita occidentale, travolgendo e mutando, sebbene solo temporaneamente, gli stili di vita, il lavoro, il tempo libero e le abitudini del mondo in cui viviamo. Il lockdown dovuto all’emergenza COVID è stato un momento critico a forte impatto, rappresentando un vero e proprio evento traumatico per il tessuto sociale e la salute mentale [4]. Il sistema sanitario ha dovuto affrontare cambiamenti importanti come la trasformazione del lavoro con pressioni e stress fortemente aumentati, cambiamenti di procedure e rischi amplificati [5]. Il Covid-19 è diventato il principale nemico, assorbendo gran parte delle risorse destinate alla cura, alla prevenzione e alla ricerca. Fondamentale per ridurre l’impatto della pandemia è stata la fornitura adeguata di equipaggiamento sanitario, per cui sono state messe in campo politiche di coordinamento internazionale, pianificazione e controllo della supply chain, nonché incentivi pubblici per la produzione. Nonostante gli sforzi effettuati, permangono tuttora delle difficoltà. Bisogna considerare che Martinez-Perez et al (2020), prendendo in esame il periodo tra gennaio e luglio 2020, aveva evidenziato 14335 pubblicazioni e 42374 citazioni che avessero come oggetto di studio il Covid-19, indipendentemente dal tipo di pubblicazione, con lo scopo di evidenziare quanto la ricerca e la medicina si siano quasi completamente indirizzate verso la battaglia contro il Covid-19 [6].
Razionale dello studio
Lo scopo di questo studio è quello di accertare, attraverso una revisione della letteratura, se effettivamente dai dati pubblicati nella letteratura scientifica da colleghi in strutture ospedaliere del territorio italiano, emerga un calo delle prestazioni sanitarie generale durante il primo periodo di lockdown (dal 09/03/2020 al 04/05/2020). In questo modo sarà possibile dimostrare il disagio subito dai pazienti non affetti da Covid-19, comprenderne i possibili motivi ed individuarne le possibili soluzioni.
Materiali e metodi
Attraverso la Banca Dati Pubmed si è ricercata la parola “lockdown” e la parola “Italy”, unite dall’operatore booleano “AND”, mettendo come unico filtro di ricerca tutti gli articoli pubblicati a partire dall’01/02/2020. Al 6/11/2020 comparivano 591 risultati.
Sono stati presi in considerazione esclusivamente i risultati comparse sula banca dati Pubmed (indifferentemente dal tipo di studio, escludendo altri database di ricerca), che contenessero dati riferiti al periodo di lockdown esaminato (gennaio 2020 - maggio 2020) e si rivolgessero verso prestazioni ospedaliere. Nello studio proposto non sono stati esclusi risultati presenti in altre fonti della bibliografia. Ove è stato possibile si è fatto più preciso riferimento al periodo 09/03/2020-04/05/2020; sono stati comunque considerati periodi di studio che in parte coincidessero con il periodo di lockdown o con parte di esso. Nella Tabella 1 è stato indicato il periodo di studio di ogni singola citazione, il campione citato nel 2019 e nel 2020 e la riduzione in percentuale (arrotondata per difetto). Dopo la lettura del titolo sono stati presi in considerazione 137 risultati. Dopo la lettura dell’abstract sono rimaste 56 risultati. 5 articoli riportavano dati parziali o riferiti solo all’anno 2020 (con paragoni con i primi mesi del 2020, tra cui 1 pubblicazione che paragonava i dati dei primi mesi del 2020 con i mesi finali del 2019, oppure medie calcolate tra il 2019 e altri anni ma senza dati singoli), 1 revisione, il restante non riportava dati sull’argomento. Sono state infine considerate un totale di 40 risultati.

Sono stati individuati seguenti studi afferenti a queste discipline mediche:
- 1- 2 studi mostrano i dati relativi ad accessi al PS (pronto soccorso), di cui 1 mostra anche i
- dati relativi ai ricoveri
- 8 studi relativi all’ambito cerebro-cardio vascolare;
- 2 riguardo chirurgia e terapia oncologica;
- 4 riguardo la chirurgia d’urgenza;
- 1 riguardo le visite e i controlli diabetologici;
- 8 riguardo l’accesso al PS e a visite e ricoveri per pazienti pediatrici;
- 1 riguardo i ricoveri di tipo ginecologico e ostetrico;
- 2 riguardo la chirurgia e la diagnostica ortopedica;
- 2 riguardo l’urologia;
- 6 riguardo la diagnostica e l’interventistica dermatologica;
- 3 riguardanti le visite e i controlli d’urgenza in ambito psichiatrico;
- 1 riguardo la diagnostica radiologica.
Risultati
Nel periodo del lockdown italiano, si è riscontrato una diminuzione del numero di accessi e di screening. L’ospedale di Trieste, valutando il periodo 10/03-30/04 del 2019 e del 2020, ha avuto rispettivamente 10424 e 4664 ingressi in pronto soccorso, con una riduzione del 55.5 % [7]. Un altro studio, con dati dell’ASST degli “Spedali Civili” di Brescia, prendendo in esame il periodo dal 23/02/2020 all’01/03/2020 e il periodo 02/03/2020-03/05/2020, mostra la riduzione di accessi al pronto soccorso dagli stessi periodi del 2019 rispettivamente di 67.36 unità giornaliere, il 31.8%, e di 93.17 unità, il 44.7%; i ricoveri invece hanno avuto una riduzione rispettivamente di 6.27, il 12.7%, e di 2.89 unità, il 5.6%) [8]. Si è scelto di dividere l'analisi per tipo di prestazione, e i valori riportati nelle citazioni sono stati elencati nella Tabella 1. Gli studi sono stati inseriti indicando il primo autore, il tipo di prestazione, il tempo di studio per gli anni 2019 e 2020, la percentuale di riduzione delle prestazioni arrotondate per difetto. Per ricoveri o prestazioni di natura cardiovascolare, si sono considerati otto studi. Tarantini [9] mostra la cardiologia interventistica strutturale in Italia dal 16 marzo al 12 aprile: sostituzioni transcatetere transfemorale della valvola aortica, riparazioni percutanea della valvola mitrale, occlusioni dell’auricola sinistra, chiusure del forame ovale pervio; gli interventi totali di queste procedure nel periodo considerato del 2020 sono stati 185 (909 nello stesso periodo 2019). Due studi hanno riguardato l’infarto acuto, e mostrano entrambi una riduzione in termini numerici dei ricoveri; Severino [10] mostra i ricoveri per infarto nel 2020 in otto ospedali italiani e li confronta con lo stesso periodo del 2019; Colivicchi [11] mostra anche i dati relativi agli accessi totali al dipartimento di emergenza del “San Filippo Neri” del 2019 e del 2020; uno studio con i dati di due ospedali di Ravenna e di Rimini confronta i ricoveri per sindrome coronarica acuta [12]; un altro dell’ospedale universitario di Udine [13] mostra i ricoverati per patologie cardiovascolari severe; in Campania, valutando i dati di quattordici ospedali, tra il 10/03/2020 e il 04/05/2020, si è manifestato un calo delle ospedalizzazioni per pazienti con bisogno di impianti per aritmie (367 nel 2020, 584 nel 2019), con un aumento in proporzioni di sincopi aritmogene trattate rispetto ai ricoveri (107 ricoveri trattati nel 2019, 97 nel 2020) [14]. Nappi [15] mostra che anche esami come le scintigrafie miocardiche (eseguite al “Federico II” di Napoli nel periodo febbraio-maggio 2020) sono state meno del 30 % rispetto all’anno precedente. All’ospedale universitario di Trieste, nell’unità adibita agli stroke, tra il 9 marzo e il 9 aprile 2020 hanno avuto una riduzione dei ricoveri del 44.8 % rispetto al 2019 [16].
Per quanto riguarda l’accesso a cure oncologiche, sono stati presi in considerazione due studi.: nella tabella sono mostrati i dati dell’ospedale “Città della Salute e della Scienza” di Torino (gli accessi alla chirurgia oncologica, con trend simili rispetto ai tre anni precedenti nel periodo marzo-maggio 2020, tranne un calo significativo nelle operazioni al seno del 31.9%, 109 nel 2020 e 160 nel 2019, e nelle operazioni non oncologiche come la colecistectomia) [17] e dell’ICS “Maugeri” di Pavia (i pazienti che hanno avuto accesso a cure per tumori sono stati circa il 77% rispetto alla media dei quattro anni precedenti nello stesso periodo di studio) [18].
Riguardo la chirurgia d’urgenza, sono state considerate quattro citazioni: i dati del Policlinico “Tor Vergata” di Roma parlano di una riduzione di ingressi dell’84.45% nel periodo di lockdown rispetto allo stesso periodo dell’anno precedente [19]; una corrispondenza mostra i dati durante l’intero periodo di lockdown del dipartimento di Chirurgia dell’Ospedale Universitario “La Sapienza” di Roma [20]; Rosa [21] mostra gli accessi al PS al Policlinico Gemelli di Roma seguiti da trattamento chirurgico tra il 20 febbraio e il 3 maggio, 120, e li compara al 2018, 226, e al 2019, 229; uno studio mostra i ricoveri in chirurgia d’urgenza all’ospedale di Ferrara tra il 9 marzo del 9 aprile rispettivamente del 2019 (46) e del 2020 (27) [22].
Un solo studio nel distretto municipale di Padova mostra un calo a 660 visite diabetologiche tra il 15/03/2020 e il 14/04/2020, rispetto alle 1208 e 1316 dello stesso periodo negli anni 2018 e 2019 [23].
Otto studi riguardano gli accessi al PS pediatrico e ai ricoveri: uno eseguito al Gaetano Pini di Milano[24], uno studio di due ospedali universitari di Torino (Regina Margherita) e Roma (Policlinico Umberto I) [25]; uno in due ospedali della Campania (San Giovanni di Dio e Ruggi d’Aragona di Salerno e l’A.O.R.N. Santobono-Pausilipon di Napoli) [26]; una corrispondenza mostra i dati della Fondazione IRCCS Policlinico San Matteo di Pavia, evidenziando un calo delle visite in pronto soccorso del 72 %, con solo gli interventi da trauma aumentati dal 2019 [27]; un’altra citazione annota di dati di un ospedale lombardo, con una diminuzione di ingressi per malattie infettive infantili [28]; le ultime fonti evidenziano un calo di ingressi al PS comparando i mesi di marzo 2019 e 2020 negli ospedali “Cesare Arrigo” di Alessandria [29], all’IRCCS materno infatile “Burlo Garofolo” di Trieste [30], e uno dell’ospedale “Degli Infermi” di Biella e del ASL “San Paolo” di Bari [31].
Un solo articolo studia gli accessi al PS di natura ginecologica e ostetrica (compresi parti e complicanze post partum, ed includendo anche i ricoveri per violenza sessuale o domestica), nel periodo 24/02-31/05, nella Clinica “Mangiagalli” del Policlinico di Milano [32].
La chirurgia ortopedica è rappresentata da due fonti: in due ospedali delle Marche è stata ritardata il più possibile la chirurgia ortopedica d’urgenza durante il lockdown, pressochè sospesi tutti gli interventi programmati, e ritardati di notevoli mesi (tra il 09/03/2020 al 09/04/2020 si è riscontrato un calo del 46% da interventi per traumi, del 19% da urgenze e del 100% da interventi programmati rispetto allo stesso periodo del 2019) [33]; in uno studio all’ IRCCS Istituto Ortopedico “Galeazzi” di Milano le ossidensometrie sono state dimezzate nel 2020 tra il 24/01 e il 27/05 rispetto l’anno precedente, con 0 esami fatti nell’aprile 2020 [34].
Due citazioni sono state considerate per mostrare le prestazioni di natura urologica: alla Fondazione IRCCS “Ca’ Granda Ospedale Maggiore” Policlinico di Milano, tra 11/03 e il 09/04 del 2019 e 2020 gli ingressi al pronto soccorso di natura urologica sono stati rispettivamente 195 e 45, con 23 e 8 ricoveri [35]; all’ospedale universitario Padova hanno riscontrato dati simili [36].
Riguardo la branca dermatologica, sono stati considerati tre studi: una lettera che cita dati dell’ IRCCS Policlinico San Matteo di Pavia mostra una riduzione degli interventi per melanoma (durante il lockdown 163 rispetto alle 246 dell’anno prima) e delle diagnosi [37], e un altro studio nello stesso ospedale mostra un minore numero di consulenze dermatologiche al PS [38]; un articolo con i numeri dell’ ospedale Maggiore della Carità a Novara mostra le operazioni fatte tra marzo e aprile del 2019 e del 2020, con anche il confronto con le prenotazioni. Le operazioni eseguite nel 2019 sono 95 (su 97 prenotate) contro le 46 del 2020 (su 87 prenotate) [39]; due studi riguardano invece l’oftalmologia: all’AOU di Pisa le visite per emergenze oftalmiche sono state 246 nel periodo 10/03/2020-04/05/2020, 959 nello stesso periodo 2019, con un calo del 74.3 % [40]; in uno studio di sei ospedali dislocati in tutta Italia (“Spedali Civili” Brescia; l’Istituto Clinico “Humanitas” di Bergamo; l’Ospedale “Sant’Anna” di Ferrara; l’Ospedale “Careggi” di Firenze; l’Ospedale Cardarelli di Campobasso; l’Ospedale Generale Vittorio Emanuele di Catania) comparando il periodo 10/03-09/04 del 2019 e 2020, ci sono state rispettivamente 3624 e 844 interventi di chirurgia oculistica [41]; per quanto riguarda la chirurgia otorinolaringoiatrica, uno studio al Policlinico “Umberto I” di Roma mostra un calo tra il 10 marzo e il 28 aprile 2020 rispetto all’anno prima, tuttavia si attestano su valori molto simili le prestazioni per patologie oncologiche [42].
Sono stati considerati anche tre studi relativi agli accessi psichiatrici: al Dipartimento di Salute Mentale dell’ASST di Monza, tra il 21/02 e il 3/05/2020, si sono riscontrati 225 controlli di natura psichiatrica, il 58 % del periodo 22/02-05/05/2019 (388) [43]; anche l’ospedale universitario San Paolo di Milano ha presentato accessi psichiatrici in calo durante il lockdown rispetto all’anno precedente [44]; un ulteriore studio relativo a 7 reparti psichiatrici di quattro aree italiane (Brescia, Cremona, Melegnano, Monza) mostra i dati relativi ai ricoveri psichiatrici d’urgenza nel periodo di marzo 2019 e 2020, con particolare risalto nella diminuzione dei ricoveri volontari (mentre quelli non voluti rimangono simili, 20 del 2019 contro i 18 del 2020) [45].
Infine, anche la diagnostica per immagini è diminuita: uno studio di Roma comparando le prestazioni radiologiche nel periodo tra il 11/03 e l’08/04 degli anni 2019 e 2020 mostra un calo del 48.2%[46].

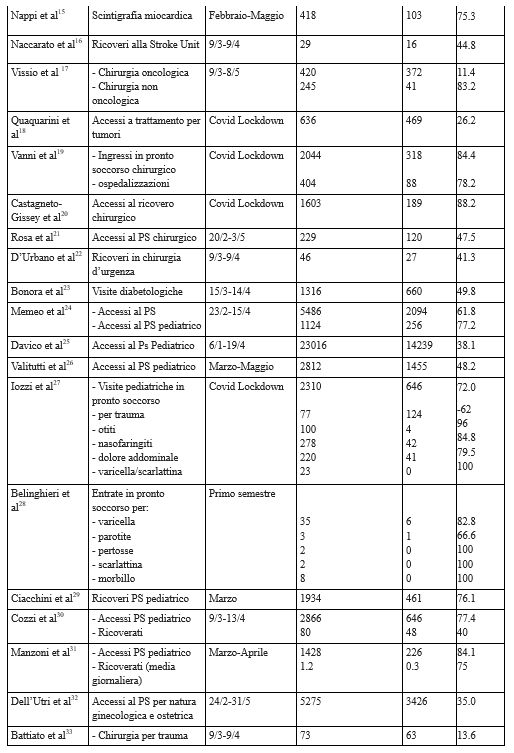
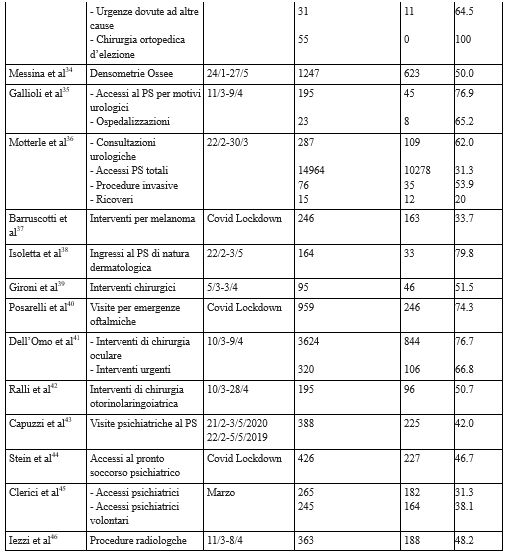
Discussione
Gli studi selezionati mostrano uniformemente in tutto il territorio italiano un calo di ingressi al pronto soccorso e di ricoveri per patologie diverse dal Covid-19. Roscigno M (2020) [47] spiega il calo di prestazioni poiché, durante l’era del Coronavirus, si sono ridotte le risorse per tante patologie croniche e di urgenza e per la loro prevenzione; risorse che sono state invece destinate alla lotta al Coronavirus. È infatti accettabile il fatto che nel breve periodo di lockdown si siano ridotti i controlli di screening, almeno sulla popolazione non a rischio; tuttavia dopo il primo mese di incertezza sarebbe stato opportuno cercare di riprendere in mano la situazione, riportandola ad una normalità assistenziale, considerando le complicazioni di un’ondata successiva senza aver recuperato gli strascichi assistenziali mancati nella prima. E’ inoltre necessario quindi individuare nuove strategie assistenziali, per proteggere il personale sanitario e non esporre il paziente al contagio del virus, e allo stesso tempo non trascurare i malati non Covid-19. Questo discorso è già stato citato in notevoli studi [48].
Anche Grande R (2020) [49] parla delle difficoltà avute dai diabetici di tipo 2 ad avere cure adeguate durante il lockdown; Vanni parla infatti nella sua discussione dello stop degli screening, come quello per il cancro al seno, mostrando i dati delle diagnosi (approssimativamente 53500) effettuate nel corso dell’anno 2019 [50].
Per quanti riguarda gli ingressi in PS, anche questi sono calati notevolmente: la paura del virus potrebbe essere stato un deterrente efficace. Se da un lato è stato utile per diminuire gli ingressi non necessari in PS (gli studi citati mostrano un aumento notevole della percentuale di ingressi in PS seguiti da ricovero, ciò vale sopratutto per quelli di natura pediatrica [30-31], dove si può ritenere che la paura del virus abbia fatto in modo di gestire molte delle patologie infettive dell’infanzia a casa senza necessità di accesso al PS e, in alcuni casi, del ricovero), dall’altro lato si nota comunque anche un calo dei ricoveri in termini assoluti. Ciò significa che anche chi poteva aver necessità dell’ospedalizzazione ha preferito evitare e gestire la propria situazione domiciliarmente. E ciò vale per molte patologie anche gravi a rischio vita. Il fatto che ricoveri per infarto [9,10] e stroke [16] in alcune zone d’Italia siano calati è indice che anche gravi patologie non abbiano avuto la normale assistenza; lo stesso discorso si può fare anche per la chirurgia oncologica [17,18], che ha presentato meno accessi e interventi. Le prestazioni ambulatoriali o non urgenti sono calate drasticamente, addirittura in alcune situazioni azzerate [33-42]. Anche le emergenze di natura psichiatrica sono calate [43-47].
Perciò si può dimostrare che il Covid-19 ha penalizzato, come detto precedentemente, la prevenzione e la cura di tutte le altre patologie. Per invece ridurre gli ingressi con codice verde e bianco al PS, rimuovendo gli ingressi “inutili” (cioè curabili anche con risorse non ospedaliere), e cercare di arrivare a una percentuale migliore di quella precendente al Covid.19, occorre potenziare la medicina nel territorio, con partecipazione maggiore dei medici di medicina generale nella gestione del paziente cronico per evitare ulteriori ricadute, e nel paziente con codice verde e bianco.
Le prestazioni ambulatoriali o non urgenti sono calate drasticamente, addirittura in alcune situazioni azzerate.
È perciò necessario pensare a nuove possibilità per garantire il percorso assistenziale dei malati cronici e di quelli ugenti non Covid, cercando di tutelare il paziente dal contagio, ma senza scoraggiarlo per la presenza del virus.
E’ inoltre importante iniziare a pensare al periodo pandemico come un’opportunità per sperimentare le nuove tecnologie: Ceriello [51] esprime parere positivo sull’uso della telemedicina durante la pandemia da Coronavirus; altri studi concordano sull’efficacia della telemedicina, per lo più positivi [52,53,54]; la telemedicina infatti è stata utile nel controllo dei pazienti diabetici e di alcune patologie cardiache [55,56]. Ciò dimostra quanto possa essere utile favorire questo metodo d’approccio, dove possibile, per tutelare al meglio gli operatori sanitari, e cercare di garantire una continuità assistenziale in molte branche della medicina anche a casa, e, con la diffusione delle tecnologie tra la popolazione di oggi, bisogna implementare la tecnologia e potenziarla, come mezzo anche di prima diagnosi, e come mezzo per un consulto rapido al paziente che si autogestisce.
Conclusione
I dati dimostrano un calo delle prestazioni per il paziente non covid-19, anche quelli gravi, e una diminuzione dei servizi di prevenzione, soprattutto per patologie che, se diagnosticate in ritardo, possono diminuire notevolmente l’aspettativa di vita. A tal proposito si evince la necessità di una maggiore consapevolezza da parte delle istituzioni di maggiori investimenti in ambito sanitario, sia in risorse umane, strutturali e strumentali, sia in ambito preventivo [57]. D’altro canto, si denota come sia anche aumentata considerevolmente la percentuale di ricoveri diretti dopo ingresso da PS per i pazienti non covid, causata da un minor ingresso di persone in PS. Ciò a dimostrazione della meticolosità nella scelta di un eventuale ricovero da parte dei pazienti stessi, cosa che ha portato ad una diminuzione dei cosiddetti ingressi inutili in pronto soccorso, riducendo file e liste di attesa. Tuttavia a questo aspetto positivo è seguita anche una diminuzione in termini assoluti dei ricoverati successivi all’ingresso in Pronto Soccorso, anche per patologie severe, denotando perciò una minor ospedalizzazione anche per patologie a rischio vita. Si evince conseguenzialmente che un aspetto che potrebbe essere sicuramente migliorato è quello informativo, attraverso l’utilizzo di diversi mezzi di comunicazione, quali ad esempio pubblicità o brochure, atte sia a dare maggiore visibilità all’operato dei sanitari, troppo spesso oberati di lavoro, che per fornire informazioni sanitarie in linea con quelle che sono le esigenze sanitarie declarate, in base alla fascia d’età e all’area territoriale presa in considerazione. La pandemia ha esasperato i contrasti tra Stato nazionale e Regioni. È necessario quindi intervenire per riequilibrare l’assetto istituzionale all’origine di questo scontro. Il principio di eguaglianza richiede una tutela uniforme dei diritti e delle prestazioni sociali su tutto il territorio nazionale. È necessario ridefinire una nuova strategia che punti sulla sanità territoriale e che garantisca a tutti l’accesso ai servizi di cura, prevenzione e riabilitazione, che potenzi le strutture ospedalieri pubbliche, che assuma nuovi medici e infermieri, che utilizzi le nuove tecnologie offerte dalla telemedicina, che promuova un’adeguata integrazione dei servizi sociosanitari e che si prenda carico delle persone non autosufficienti.
Limiti dello Studio
I limiti dello studio sono rappresentati dalla selezione dei campioni di notevole eterogeneità per le patologie proposte: una ricerca più approfondita su argomenti precisi, ad esempio una determinata tipologia di prestazioni ospedaliere, avrebbe affinato la ricerca, insieme all’uso di altre banche dati e con l’ausilio di letteratura grigia. I dati possono essere soggetti a bias non avendo avuto riscontro da canali istituzionali, e basandosi su dati in database da medici e operatori sanitari diversi; inoltre bisogna considerare la possibilità di ricoveri per diagnosi errata o solo parzialmente corretta. Anche una selezione geografica (come lo studio in una singola Regione) avrebbe migliorato la ricerca. Infine la mancanza di linee guida e protocolli da attuare immediatamente nelle strutture ospedaliere avrebbe potuto cambiare parzialmente i risultati.
Conflitto di interessi
Gli autori dichiarano l’assenza di conflitti di interesse.
Finanziamenti
Gli autori dichiarano di non aver ottenuto alcun finanziamento e che lo studio non ha alcuno sponsor economico.
BIBLIOGRAFIA
-
- WHO, Weekly Epidemiological Update – 27 January 2021, https://www.who.int/publications/m/item/weekly-epidemiological-update---27-january-2021
- Umakanthan S, Sahu P, Ranade AV, Bukelo MM, Rao JS, et al, Origin, transmission, diagnosis and management of coronavirus disease 2019 (COVID-19), Postgrad Med J. 2020 Dec;96(1142):753-758
- Caratteristiche dei pazienti deceduti positivi all’infezione da SARS-CoV-2 in Italia, Dati al 27 gennaio 2021, Istituto Superiore di Sanità, https://www.epicentro.iss.it/coronavirus/bollettino/Report-COVID-2019_27_gennaio_2021.pdf
- Gualano MR, Lo Moro G, Voglino G, Bert F, Siliquini R, Effects of Covid-19 Lockdown on Mental Health and Sleep Disturbances in Italy, Int J Environ Res Public Health. 2020 Jul 2;17(13):4779
- Rossi R, Socci V, Pacitti F, Di Lorenzo G, Di Marco A, et al, Mental Health Outcomes Among Frontline and Second-Line Health Care Workers During the Coronavirus Disease 2019 (COVID-19) Pandemic in Italy, JAMA Netw Open. 2020 May 1;3(5):e2010185. doi: 10.1001/jamanetworkopen.2020.10185
- Martinez-Perez C, Alvarez-Peregrina C, Villa-Collar C, Sánchez-Tena MA, Citation Network Analysis of the Novel Coronavirus Disease 2019 (COVID-19), Int J Environ Res Public Health. 2020 Oct 21;17(20):E7690. doi: 10.3390/ijerph17207690
- Cheli M, Dinoto A, Olivo S, Tomaselli M, Stokelj D, et al, SARS-CoV-2 pandemic and epilepsy: The impact on emergency department attendances for seizures, Seizure. 2020 Aug 22;82:23-26
- Garrafa E, Levaggi R, Miniaci R, Paolillo C, When fear backfires: Emergency department accesses during the Covid-19 pandemic, Health Policy. 2020 Oct 24;S0168-8510(20)30261-X
- Tarantini G, Fovino LN, Scotti A, Marchese A, Berti S, et al, [Impact of COVID-19 pandemic on structural heart interventions in Italy], G Ital Cardiol (Rome). 2020 Nov;21(11):45-47
- Severino P, D'Amato A, Saglietto A, et al, Reduction in heart failure hospitalization rate during coronavirus disease 19 pandemic outbreak, ESC Heart Fail. 2020 Oct 23. doi: 10.1002/ehf2.1304
- Colivicchi F, Di Fusco SA, Magnanti M, et al, The Impact of the Coronavirus Disease-2019 Pandemic and Italian Lockdown Measures on Clinical Presentation and Management of Acute Heart Failure, J Card Fail. 2020 Jun;26(6):464- 465
- Fileti L, Vecchio S, Moretti C, Impact of the COVID-19 pandemic on coronary invasive procedures at two Italian high-volume referral centers, J Cardiovasc Med (Hagerstown). 2020 Nov;21(11):869-873
- Toniolo M, Negri F, Antonutti M, Masè M, Facchin D, Unpredictable Fall of Severe Emergent Cardiovascular Diseases Hospital Admissions During the COVID-19 Pandemic: Experience of a Single Large Center in Northern Italy, J Am Heart Assoc. 2020 Jul 7;9(13):e017122
- Russo V, Pafundi PC, Rapacciuolo A, D'Andrea A, de Devitiis M, et al, Arrhythmogenic syncope leading to cardiac rhythm management procedures during COVID-19 lockdown, Expert Rev Med Devices. 2020 Oct 22. doi: 10.1080/17434440.2020.1841632
- Nappi C, Megna R, Acampa W, Assante R, Zampella E, et al, Effects of the COVID-19 pandemic on myocardial perfusion imaging for ischemic heart disease, Eur J Nucl Med Mol Imaging. 2020 Aug 11;1-7
- Naccarato M, Scali I, Olivo S, Ajcevic M, Stella AB, et al, Has COVID-19 played an unexpected "stroke" on the chain of survival?, J Neurol Sci. 2020 Jul 15;414:116889
- Vissio E, Falco EC, Collemi G, Borella F, Papotti M, et al, Impact of COVID-19 lockdown measures on oncological surgical activity: Analysis of the surgical pathology caseload of a tertiary referral hospital in Northwestern Italy, J Surg Oncol. 2020 Oct 20. doi: 10.1002/jso.26256
- Quaquarini E, Saltalamacchia G, Presti D, Caldana G, Tibollo V, et al, Impact of COVID-19 Outbreak on Cancer Patient Care and Treatment: Data from an Outpatient Oncology Clinic in Lombardy (Italy), Cancers (Basel). 2020 Oct 12;12(10):E2941
- Vanni G, Legramante JM, Pellicciaro M, DE Carolis G, Cotesta M, et al, Effect of Lockdown in Surgical Emergency Accesses: Experience of a COVID-19 Hospital, In Vivo. Sep-Oct 2020;34(5):3033-3038
- Castagneto-Gissey L, Casella G, Russo MF, Del Corpo G, Iodice A, et al, Impact of COVID-19 outbreak on emergency surgery and emergency department admissions: an Italian level 2 emergency department experience, Br J Surg. 2020 Jul 20;10.1002/bjs.11813
- Rosa F, Covino M, Sabia L, Quero G, Fiorillo C, et al, Surgical emergencies during SARS-CoV-2 pandemic lockdown: what happened?, Eur Rev Med Pharmacol Sci. 2020 Nov;24(22):11919-11925
- D'Urbano F, Fabbri N, Radica MK, Rossin E, Calcoforo P, Emergency surgery in COVID-19 outbreak: Has anything changed? Single center experience, World J Clin Cases. 2020 Sep 6;8(17):3691-3696
- Bonora BM, Morieri LM, Avogaro A, Fadini GP, The Toll of Lockdown Against COVID-19 on Diabetes Outpatient Care: Analysis From an Outbreak Area in Northeast Italy, Diabetes Care. 2020 Oct 30;dc201872
- Memeo A, Priano D, Caldarini C, et al, How the pandemic spread of COVID-19 affected children's traumatology in Italy: changes of numbers, anatomical locations, and severity, Minerva Pediatr. 2020 Oct 5. doi: 10.23736/S0026-4946.20.05910-1
- Davico C, Marcotulli D, Lux C, et al, Where have the children with epilepsy gone? An observational study of seizure-related accesses to emergency department at the time of COVID-19, Seizure. 2020 Oct 5;83:38-40
- Valitutti F, Zenzeri L, Mauro A, Pacifico R, Borrelli M, et al, Effect of Population Lockdown on Pediatric Emergency Room Demands in the Era of COVID-19, Front Pediatr. 2020 Sep 18;8:521
- Iozzi L, Brambilla I, Foiadelli T, Marseglia GL, Ciprandi G, Paediatric emergency department visits fell by more than 70% during the COVID‐19 lockdown in Northern Italy, Acta Paediatr. 2020 Jul 4 : 10.1111/apa.15458
- Belingheri M, Paladino ME, Piacenti S, Riva MA, Effects of COVID-19 lockdown on epidemic diseases of childhood, J Med Virol. 2020 Jul 3;10.1002/jmv.26253. doi: 10.1002/jmv.26253
- Ciacchini B, Tonioli F, Marciano C, et al, Reluctance to seek pediatric care during the COVID-19 pandemic and the risks of delayed diagnosis, Ital J Pediatr. 2020 Jun 29;46(1):87
- Cozzi G, Zanchi C, Giangreco M, Rabach I, Calligaris L, et al, The impact of the COVID-19 lockdown in Italy on a paediatric emergency setting, Acta Paediatr. 2020 Jun 29;10.1111/apa.15454
- Manzoni P, Militello MA, Fiorica L, et al, Impact of COVID-19 epidemics in paediatric morbidity and utilisation of Hospital Paediatric Services in Italy, Acta Paediatr. 2020 Jun 22;10.1111/apa.15435. doi: 10.1111/apa.15435
- Dell'Utri C, Manzoni E, Cipriani S, et al, Effects of SARS Cov-2 epidemic on the obstetrical and gynecological emergency service accesses. What happened and what shall we expect now?, Eur J Obstet Gynecol Reprod Biol. 2020 Nov;254:64-68
- Battiato C, Berdini M, Luciani P, Gigante A, Impact of coronavirus disease 2019 (COVID-19) on the epidemiology of orthopedics trauma in a region of central italy, Injury . 2020 Oct 2;S0020-1383(20)30778-6
- Messina C, Buzzoni AC, Gitto S, Disruption of bone densitometry practice in a Northern Italy Orthopedic Hospital during the COVID-19 pandemic, Osteoporos Int. 2020 Aug 10;1-5
- Gallioli A, Albo G, Lievore E, Boeri L, Longo F, et al, How the COVID-19 Wave Changed Emergency Urology: Results From an Academic Tertiary Referral Hospital in the Epicentre of the Italian Red Zone, Urology. 2020 Oct 1;S0090-4295(20)31186-9
- Motterle G, Morlacco A, Iafrate M, Bianco M, Federa G, et al, The impact of COVID-19 pandemic on urological emergencies: a single-center experience, World J Urol. 2020 May 23;1-5
- Barruscotti S, Giorgini C, Brazzelli V, Vassallo C, Michelerio A, et al, A significant reduction in the diagnosis of melanoma during the COVID-19 lockdown in a third-level center in the Northern Italy, Dermatol Ther. 2020 Jul 26;e14074
- Isoletta R, Vassallo C, Brazzelli V, Giorgini C, Tomasini CF, et al, Emergency accesses in Dermatology Department during the Covid-19 pandemic in a referral third level center in the north of Italy, Dermatol Ther. 2020 Nov;33(6):e14027. doi: 10.1111/dth.14027
- Gironi LC, Boggio P, Giorgione R, Esposito E, Tarantino T, et al, The impact of COVID-19 pandemics on dermatologic surgery: real-life data from the Italian Red-Zone, J Dermatolog Treat . 2020 Jul 7;1-7
- Posarelli C, Maglionico MN, Covello G, Logiudice P, Cipriano A, et al, Ophthalmological emergencies and the SARS-CoV-2 outbreak, Observational Study PLoS One . 2020 Oct 1;15(10):e0239796
- dell'Omo R, Filippelli M, Semeraro F, Avitabile T, Giansanti F et al, Effects of the first month of lockdown for COVID-19 in Italy: A preliminary analysis on the eyecare system from six centers, Eur J Ophthalmol. 2020 Aug 24;1120672120953074
- Ralli M, Minni A, Candelori F, Cialente F, Greco A, de Vincentiis M, Effects of COVID-19 Pandemic on Otolaryngology Surgery in Italy: The Experience of Our University Hospital, Otolaryngol Head Neck Surg . 2020 Jul;163(1):86-88
- Capuzzi E, Di Brita C, Caldiroli A, Colmegna F, Nava R, et al, Psychiatric emergency care during Coronavirus 2019 (COVID 19) pandemic lockdown: results from a Department of Mental Health and Addiction of northern Italy, Psychiatry Res. 2020 Sep 18;293:113463
- Stein H-C, Giordano B, Del Giudice R, Basi C, Gambini O, D'Agostino A, Pre/post comparison study of emergency mental health visits during the COVID-19 lockdown in Lombardy, Italy, Psychiatry Clin Neurosci. 2020 Nov;74(11):605-607
- Clerici M, Durbano F, Spinogatti F, et al, Psychiatric hospitalization rates in Italy before and during COVID-19: did they change? An analysis of register data, Ir J Psychol Med. 2020 May 5;1-8
- Iezzi R, Valente I, Cina A, et al, Longitudinal study of interventional radiology activity in a large metropolitan Italian tertiary care hospital: how the COVID-19 pandemic emergency has changed our activity, Eur Radiol. 2020 Dec;30(12):6940-6949
- Roscigno M, Naspro R, Piccichè A, Muttin F, Angiolilli D, et al, A Snapshot from the Department of Urology in Bergamo Evaluating the Timeline of the SARS-CoV-2 Outbreak: Which Patients Are We Missing?, Eur Urol Focus. 2020 Sep 15;6(5):1120-1123
- Viganò M, Mantovani M, Cozzolino P, Harari S, Treat all COVID 19-positive patients, but do not forget those negative with chronic diseases, Intern Emerg Med. 2020 Jun 9 : 1–4
- Grande R, Fiori G, Russo G, Filamonti P, Campagnol M, di Marzo L, A multistage combined approach to promote diabetic wound healing in COVID-19 era, Int Wound J. 2020 Aug 21;10.1111/iwj.13476. doi: 10.1111/iwj.13476
- Vanni G, Pellicciaro M, Materazzo M, Bruno V, Oldani C, et al, Lockdown of Breast Cancer Screening for COVID-19: Possible Scenario, In Vivo . Sep-Oct 2020;34(5):3047-3053
- Ceriello A, Lessons from COVID-19: How human behaviour may influence the science, Diabetes Res Clin Pract. 2020 Oct 2;169:108491
- Santonicola A, Zingone F, Camera S, Siniscalchi M, Ciacci C, Telemedicine in the COVID-19 era for Liver Transplant Recipients: an Italian lockdown area experience, Clin Res Hepatol Gastroenterol . 2020 Aug 4;S2210-7401(20)30203-5
- Di Carlo F, Sociali A, Picutti E, Pettorusso M, Vellante F, et al, Telepsychiatry and other cutting-edge technologies in COVID-19 pandemic: Bridging the distance in mental health assistance, Int J Clin Pract . 2020 Sep 18;e13716
- De Santis G, Palladino T, Acciaro AL, Starnoni M, The Telematic solutions in plastic surgery during COVID-19 pandemic, Acta Biomed. 2020 Jul 28;91(3)
- Petrelli F, Cangelosi G, Scuri S, Diabetes and technology: A pilot study on the management of patients with insulin pumps during the COVID-19 pandemic, Diabetes Res Clin Pract. 2020 Sep 28;169:108481
- Tini G, Vianello PF, Rizzola G, et al, Telehealth monitoring for hypertrophic cardiomyopathy and amyloid cardiomyopathy patients: lessons from the coronavirus disease 2019 lockdown in Italy, J Cardiovasc Med (Hagerstown). 2020 Aug;21(8):622-623
- Brusini A, An interpretation of preventive care spent in Italy and a new opportunity after COVID-19 pandemia, J Infect DisPrev Med, 2020, 9:2010
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Il rooming in e il contatto pelle a pelle madre-bambino prima e dopo il Covid-19: una riflessione
Anna Arnone1*
- Dipartimento Emergenza e Accettazione, A.O.R.N. ‘’Antonio Cardarelli’’, Napoli (Italia)
* Corresponding Author: Anna Arnone, A&E Department, A.O.R.N. ‘’Antonio Cardarelli’’, Naples (Italy). E-mail: anna.arnone93@live.it
Cita questo articolo
ABSTRACT
Un neonato sano a termine dovrebbe essere tenuto a contatto pelle a pelle con la propria madre che ha avuto un parto vaginale o un taglio cesareo con anestesia epidurale subito dopo la nascita o non appena possibile. Si definisce rooming in la permanenza del neonato e della madre nella stessa stanza in un tempo più lungo possibile durante le 24 ore. Lo scopo di questo articolo di commento è quello di discutere e generare riflessioni sulle conseguenze che il Covid-19 sta generando in quanto sta cambiando la vita e l’esperienza pre- e post-natale di molte madri e neonati nonché delle loro famiglie condizionando il contatto precoce, la diade madre-bambino, l’allattamento.
Parole Chiave: Rooming in, allattamento, benessere materno-neonatale, pandemia, Covid-19, infermieri.
Rooming in and mother-infant skin-to-skin contact: A reflection
ABSTRACT
A healthy full-term newborn should be kept in skin-to-skin contact with their mother who has had a vaginal delivery or caesarean section with epidural anesthesia soon after birth or as soon as possible. Rooming in is defined as the stay of the newborn and the mother in the same room for as long as possible during the 24 hours. The purpose of this commentary article is to discuss and generate reflections on the consequences that Covid-19 is generating ad it is changing the life and pre and postnatal experience of many mothers and babies as well as their families by affecting the early contact, the mother-infant dyad, the breastfeeding.
Keywords: Rooming in, Breastfeeding, Maternal-neonatal well-being, Pandemic, Covid-19, Nurses
INTRODUZIONE
Secondo le Linee Guida del Fondo delle Nazioni Unite per l’Infanzia (UNICEF) del 2012, si afferma che un neonato sano a termine dovrebbe essere tenuto a contatto pelle a pelle con la propria madre che ha avuto un parto vaginale o un taglio cesareo con anestesia epidurale subito dopo la nascita o non appena possibile. [1] A sostegno di quanto detto l’Organizzazione Mondiale della Sanità (OMS) e l’UNICEF hanno promosso il modello del rooming in, che si definisce come la permanenza del neonato e della madre nella stessa stanza in un tempo più lungo possibile durante le 24 ore, eccetto quello dedicato alle cure assistenziali. Il modello è stato incentivato a partire dal 1992 attraverso l’iniziativa ‘’Baby Friendly Hospital’’ al fine di garantire l’assistenza più efficiente ai neonati in tutti gli ospedali e di promuovere l’allattamento al seno [2].
Il modello organizzativo del rooming in viene suggerito in quanto propone alla madre una formazione sulle cure da dedicare al neonato per poter affrontare al meglio le difficoltà e per rilevare in maniera tempestiva eventuali segni patologici, includendo anche il padre e gli altri componenti della famiglia per condividere le cure del neonato [2,4,5]. Il neonato subito dopo la nascita viene asciugato, coperto con un telo e messo a contatto pelle a pelle con la madre per circa un paio d’ore o fino al momento della prima poppata; durante il primo contatto il neonato cerca il capezzolo grazie all’odore percepito della madre dando il via alla prima poppata [5]. Vari studi hanno dimostrato che il contatto con la madre subito dopo la nascita calma il neonato, favorisce il corretto attacco al seno, stabilizza il suo metabolismo e la temperatura corporea, regola la sua respirazione e il battito cardiaco [1,4] e fortifica il legame madre-neonato [4,6,7]. Inoltre, anche sulla salute materna determina notevoli benefici in quanto si sono riscontrati una diminuzione delle perdite di sangue post-partum, una ridotta incidenza di depressione post-partum [8] e la riduzione del cancro al seno e all’ovaio [2,7]. Se il contatto pelle a pelle non avviene in maniera corretta è necessario che gli operatori aiutino la madre attraverso delle indicazioni verbali affinché siano raggiunte la posizione e l’attacco attraverso la tecnica hands-off.
Il contatto pelle a pelle, considerati i vantaggi, può essere protratto anche dopo il periodo postnatale [9] ed è praticato ormai sia nei Paesi industrializzati che nei Paesi in via di sviluppo, assumendo anche il nome di Kangaroo Mother Care per la somiglianza con i marsupiali [10] per favorire anche la salute e il benessere del neonato di basso peso alla nascita o pretermine, che per definizione è il neonato nato prima della 37a settimana completa di gestazione [11] che ha già superato i problemi iniziali e non necessita di cure intensive [12]. Con la diffusione nel 2020 del Covid-19, l’intera salute mondiale è gravemente compromessa [13], ma non le cure rivolte a sostegno della salute materno-neonatale che sono state offerte con nuove modalità di intervento per ridurre le criticità causate dalle nuove misure di sicurezza attivate negli enti ospedalieri e territoriali. L’obiettivo di questo articolo è rivolto a far riflettere sulle conseguenze che inevitabilmente gli obblighi di distanziamento hanno generato anche nel rooming in e nel legame madre-bambino prima e dopo il parto.
Discussione
Molto dibattuta durante la pandemia da Covid-19 è stata la gestione della diade madre-bambino dopo il parto così come l’allattamento: è necessario precisare infatti, che il neonato è la categoria più a rischio di infezioni polmonari clinicamente non rilevanti ed è necessario proteggerlo nel caso in cui la madre sia positiva sia prima che dopo il parto [14,15]. Dati incoraggianti sostengono che il virus non sia stato ritrovato nel latte materno, nel liquido amniotico e nella placenta, sebbene alcuni report [16] abbiano riportato tre casistiche di neonati con IgM positive, pertanto andrebbe dimostrata la trasmissione verticale con dati più solidi. Gli altri pochissimi casi, che sono stati descritti in Cina così come nelle principali città italiane colpite dal virus, hanno contratto l’infezione dopo la nascita a domicilio e sono stati poi riospedalizzati [17]. I dati a disposizione attualmente non sono ancora sufficienti e si basano soprattutto su casistiche cinesi, anche se qualche caso è riportato anche in Italia. La Società Italiana di Neonatologia aveva pubblicato le prime indicazioni ad interim il 22 marzo 2020 [17] in accordo con le raccomandazioni di OMS, ISS, UNICEF e CDC, che da subito hanno differito, in base al quadro clinico della madre: se quest’ultima risulta positiva o sospetta ma asintomatica o con sintomi lievi sono raccomandati il rooming in e l’allattamento al seno con l’uso di mascherina, il lavaggio delle mani e la distanza di sicurezza dal neonato per prevenire la trasmissione del virus attraverso la via respiratoria sia durante l’ospedalizzazione che dopo la dimissione precoce, protetta e concordata a domicilio. Qualora, invece, la madre presentasse sintomi respiratori o compromissione della situazione clinica generale [17], sono raccomandate la separazione temporanea dal neonato e la somministrazione di latte estratto con il tiralatte. Occorre in quest’ultimo caso, valutare gli effetti negativi che condizionano il contatto precoce e determinano un fallimento dell’allattamento al seno esclusivo, di una migliore diade madre-bambino e di un calo ponderale significativo nel neonato nonché effetti negativi sulla madre: a prova di quanto detto, i risultati di un recente studio sono confortanti in quanto indicano che la trasmissione del virus da madre a neonato non è frequente e le percentuali di contagio si dimostrano variabili e inferiori rispetto ai benefici del rooming in [18], purché siano rispettati i protocolli per il contatto. Appare quindi necessario garantire la massima attenzione per valutare gli effetti del Covid-19 sulla vita e sull’esperienza pre e post-natale di molte madri, dei loro neonati e delle loro famiglie suggerendo un rooming in ‘’in sicurezza’’ quale efficace modello di assistenza materno-neonatale per facilitare l’allattamento al seno, la relazione madre-bambino e un migliore adattamento dei principali sistemi del neonato.
Eventuali Finanziamenti
Questa ricerca non ha ricevuto nessuna forma di finanziamento.
Conflitti di interesse
L’ autore dichiara di non avere conflitti di interesse associati a questo studio.
BIBLIOGRAFIA
- (2012). Guida all’applicazione dei passi. Retrieved on May, 2015, from http://www.unicef.it/Allegati/Guida_applicazione_Passi_16mag12.pdf.
- OMS & UNICEF. (2009). Manuale del partecipante. Retrieved on May 2015, from http://www.unicef.it/Allegati/Manuale_partecipante_Corso_20_ore1_7ott10.pdf.
- Società Italiana di Neonatologia. (2001). Raccomandazioni sull’allattamento materno per i nati a termine, di peso appropriato, sani. Retrieved on December, 2020, from http://allattamento.sip.it/linee-guida/raccomandazioni-sullallattamento-materno-per-i-natia-termine-di-peso-appropriato-sani/.
- (2005). Linee guida cliniche per l'attuazione dell'allattamento al seno esclusivo. Retrieved on May 2015, from http://www.aicpam.org/wpcontent/uploads/2011/02/Linee_Guida_ILCA_ITA.pdf.
- Mahmood, I., Jamal, M., & Khan, N. (2011). Effect of mother-infant early skin-to-skin contact on breastfeeding status: a randomized controlled trial. Journal of the College of Physicians and Surgeons Pakistan, 21(10), 601-605.
- Lutter, C.K., & Chaparro, C.M. (2009). Neonatal period: linking best nutrition practices at birth to optimize maternal and infant health and survival. Food and Nutrition Bulletin, 30(2), 215-224.
- Zuppa, A.A., Sindico, P., Antichi, E., Carducci, C., Alighieri, G., Cardiello, V., Cota, F. & Romagnoli, C. (2009). Weight loss and jaundice in healthy term newborns in partial and full rooming-in. Journal of Maternal-Fetal and Neonatal Medicine, 22(9), 801-805.
- Soldi A., Tonetto P., Varalda A. & Bertino E., 2011, Neonatal jaundice and human milk. Journal of Maternal-Fetal and Neonatal Medicine, 24(1), 85-87.
- Vasquez, M.J., & Berg, O.R. (2012). The baby-friendly journey in a US public hospital. Journal of Perinatal & Neonatal Nursing, 26(1), 37-46.
- Doyle LW., Kangaroo mother care. Lancet 1997, Dec 13;350(9093):1721-2.
- Department of Reproductive Health and Research, World Health Organization. Kangaroo mother care: a practical guide. 1st ed. Geneva: WHO, 2003.
- Als H, Lester BM, Tronick E and Brazelton TB. (1982) Manual for the assessment of preterm infants' behaviour (APIB). In: Fitzgerald H, Lester BM, Yogman MW eds. Theory and Research in Behavioural Pediatrics, vol. 1. New York: Plenum Press, 65-132.
- Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo CG, Ma W, et al. Risk of Covid-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5(9): e475-e483.
- Zeng L et al. Neonatal Early-OnsetInfection With SARS-CoV-2 in 33 Neonates Born to Mothers With Covid-19 in Wuhan, China. JAMA Pediatr. 2020 Mar 26. doi:10.1001/jamapediatrics.2020.0878.
- Wang S et al. A case report of neonatal COVID-19 infection in China. Clin Infect Dis. 2020 Mar 12. pii: ciaa225. doi: 10.1093/cid/ciaa225.
- Huijun Chen PhD ac et al., Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. The Lancet 395, Issue 10226, 7-13 March 2020, Pages 809-815.
- Società Italiana di Neonatologia, 22 marzo 2020. Allattamento e infezione da SARS-CoV-2. Indicazioni ad Interim della Società Italiana di Neonatologia (SIN).
- Ronchi A et al., Evaluation of rooming-in practice for neonates born to mothers with Severe Acute Respiratory Syndrome Soronavirus 2 Infection in Italy, JAMA Pediatr. 2021;175(3):260-266. doi:10.1001/jamapediatrics.2020.5086
![]() This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Capture the Beauty of Nature through Photography
Many years ago, I worked for my parents who own a video production company. Because it is a family business, you inevitably end up wearing many hats and being the czar of many different jobs. I mainly managed projects and worked as a video editor. On production, there were times that I was called on to work as an audio tech and was made to wear headphones on long production days. In those days, having a really good set of headphones that picked up every nuance of sound was essential to making sure the client got what they needed. Naturally, my first impression of these headphones is based off of the look of them. They have a classic over-the-ear style that is highlighted by a blue light that indicates the power for the noise canceling. The padding on the ear pieces seems adequate for extended usage periods.
They are wired headphones, but the stereo mini-plug cable is detachable. Something else I noticed right of the bat was the very nice carrying case that comes with them. It has a hard plastic exterior with a soft cloth interior that helps to protect the surface of the headphones from scratches. I never truly appreciated cases for headphones until I started carrying them from place-to-place. Now I can’t imagine not having a case. Once I gave the headphones a thorough once-over exam, I tried them on. As I mentioned, they have a classic over-the-ear style and just looking at them, the padding on the ear pieces seem adequate and the peak of the headband seemed to be a bit lacking, but you don’t really know comfort unless you try on the product. So, I slipped the headphones on and found them to be exquisitely comfortable.
If you look at what you have in life, you'll always have more. If you look at what you don't have in life, you'll never have enough.
Oprah Winfrey
Now that I had the headphones on my head, I was finally ready to plug and play some music. I plugged the provided cable into the jack on the headphones and then the one on my iPhone. Then I called up Pandora. I tend to have a very eclectic music purview and have many stations set up for different moods. the sound quality of these headphones was remarkable. There is an amazing depth of sound and incredible highs and lows that make listening to music a truly breathtaking experience. In order to test how voices sounded, and the overall art of mixing, I pulled up Netflix on my iPad Air and watched a few minutes of a movie to hear all the nuances of the film.
None of them were lost. In fact, I ended up hearing sounds that I hadn’t heard before. Echoes…birds chirping…wind blowing through trees…breathing of the characters…it was very impressive what the headphones ended up bringing out for me.
How to Be in the Flow and Create Something Beautiful
Just the other day I happened to wake up early. That is unusual for an engineering student. After a long time I could witness the sunrise. I could feel the sun rays falling on my body. Usual morning is followed by hustle to make it to college on time. This morning was just another morning yet seemed different.
Witnessing calm and quiet atmosphere, clear and fresh air seemed like a miracle to me. I wanted this time to last longer since I was not sure if I would be able to witness it again, knowing my habit of succumbing to schedule. There was this unusual serenity that comforted my mind. It dawned on me, how distant I had been from nature. Standing near the compound’s gate, feeling the moistness that the air carried, I thought about my life so far.
Your time is limited, so don't waste it living someone else's life. Don't be trapped by dogma – which is living with the results of other people's thinking.
Steve Jobs
I was good at academics, so decisions of my life had been pretty simple and straight. Being pretty confident I would make it to the best junior college of my town in the first round itself, never made me consider any other option. I loved psychology since childhood, but engineering was the safest option. Being born in a middle class family, thinking of risking your career to make it to medical field was not sane. I grew up hearing ‘Only doctor’s children can afford that field’ and finally ended up believing it. No one around me believed in taking risks. Everyone worshiped security. I grew up doing the same.
‘Being in the top will only grant you a good life’ has been the mantra of my life. But at times, I wish I was an average student. I wish decisions would have not been so straightforward. Maybe I would have played cricket- the only thing I feel passionate about. Or maybe I would have studied literature (literature drives me crazy). Isn’t that disappointing- me wishing to be bad at academics. It’s like at times I hate myself for the stuff I am good at.
When you step out of these four walls on a peaceful morning, you realize how much nature has to offer to you. Its boundless. Your thoughts, worries, deadlines won’t resonate here. Everything will flow away along with the wind. And you will realize every answer you had been looking for, was always known to you. It would mean a lot to me if you recommend this article and help me improve.
I Like Keep Things Simple to Appreciate the Details
Just the other day I happened to wake up early. That is unusual for an engineering student. After a long time I could witness the sunrise. I could feel the sun rays falling on my body. Usual morning is followed by hustle to make it to college on time. This morning was just another morning yet seemed different.
Witnessing calm and quiet atmosphere, clear and fresh air seemed like a miracle to me. I wanted this time to last longer since I was not sure if I would be able to witness it again, knowing my habit of succumbing to schedule. There was this unusual serenity that comforted my mind. It dawned on me, how distant I had been from nature. Standing near the compound’s gate, feeling the moistness that the air carried, I thought about my life so far.
Your time is limited, so don't waste it living someone else's life. Don't be trapped by dogma – which is living with the results of other people's thinking.
Steve Jobs
I was good at academics, so decisions of my life had been pretty simple and straight. Being pretty confident I would make it to the best junior college of my town in the first round itself, never made me consider any other option. I loved psychology since childhood, but engineering was the safest option. Being born in a middle class family, thinking of risking your career to make it to medical field was not sane. I grew up hearing ‘Only doctor’s children can afford that field’ and finally ended up believing it. No one around me believed in taking risks. Everyone worshiped security. I grew up doing the same.
‘Being in the top will only grant you a good life’ has been the mantra of my life. But at times, I wish I was an average student. I wish decisions would have not been so straightforward. Maybe I would have played cricket- the only thing I feel passionate about. Or maybe I would have studied literature (literature drives me crazy). Isn’t that disappointing- me wishing to be bad at academics. It’s like at times I hate myself for the stuff I am good at.
When you step out of these four walls on a peaceful morning, you realize how much nature has to offer to you. Its boundless. Your thoughts, worries, deadlines won’t resonate here. Everything will flow away along with the wind. And you will realize every answer you had been looking for, was always known to you. It would mean a lot to me if you recommend this article and help me improve.
Thriving for Simplicity and Ease of Use Sharing Knowledge
Just the other day I happened to wake up early. That is unusual for an engineering student. After a long time I could witness the sunrise. I could feel the sun rays falling on my body. Usual morning is followed by hustle to make it to college on time. This morning was just another morning yet seemed different.
Witnessing calm and quiet atmosphere, clear and fresh air seemed like a miracle to me. I wanted this time to last longer since I was not sure if I would be able to witness it again, knowing my habit of succumbing to schedule. There was this unusual serenity that comforted my mind. It dawned on me, how distant I had been from nature. Standing near the compound’s gate, feeling the moistness that the air carried, I thought about my life so far.
import styles from './MyComponent.css';
import React, { Component } from 'react';
export default class MyComponent extends Component {
render() {
return (
<div>
<div className={styles.foo}>Foo</div>
<div className={styles.bar}>Bar</div>
</div>
);
}
I was good at academics, so decisions of my life had been pretty simple and straight. Being pretty confident I would make it to the best junior college of my town in the first round itself, never made me consider any other option. I loved psychology since childhood, but engineering was the safest option. Being born in a middle class family, thinking of risking your career to make it to medical field was not sane. I grew up hearing ‘Only doctor’s children can afford that field’ and finally ended up believing it. No one around me believed in taking risks. Everyone worshiped security. I grew up doing the same.
process.env.NODE_ENV === 'development' ?
'[name]__[local]___[hash:base64:5]' :
'[hash:base64:5]'
)
When you step out of these four walls on a peaceful morning, you realize how much nature has to offer to you. Its boundless. Your thoughts, worries, deadlines won’t resonate here. Everything will flow away along with the wind. And you will realize every answer you had been looking for, was always known to you. It would mean a lot to me if you recommend this article and help me improve.