Federico Pecetta 1, Gian Domenico Giusti 2,3*, Sara Staffaroni 4, Matteo Ricci 5
- Department of Emergency Medicine, Emergency Health Operations Centre Arezzo, San Donato Hospital, Arezzo, Italy
- Department Teaching and Quality, Hospital of Perugia, Perugia, Italy
- Department of Medicine and Surgery of the University of Perugia, Perugia, Italy
- Department of Maternal and Child Health, San Donato Hospital, Arezzo, Italy
- Department of Anaesthesia and Critical Care Careggi University Hospital, University of Florence, Florence, Italy
* Corresponding author: Gian Domenico Giusti, Department of Medicine and Surgery of the University of Perugia, Piazza Lucio Severi, 1 Edificio B – piano +1 - 06132 Perugia, Italy. ORCID: https://orcid.org/0000-0001-9167-9845. Email: giandomenico.giusti@unipg.it.
Federico Pecetta, Gian Domenico Giusti, Sara Staffaroni, Matteo Ricci
Original Article
DOI:10.32549/OPI-NSC-115
Submitted: 18 October 2024
Revised: 17 January 2025
Accepted: 18 January 2025
Published online: 27 January 2025
License: This article is licensed under the Creative Commons Attribution - Non Commercial - No Derivatives 4.0 (CC BY NC ND 4.0) international license.
Keywords: Pain management, Emergency nurses, Pre-hospital care, Analgesic drugs, Pain assessment
Abstract:
Numerous studies show that the prevalence of pain in pre-hospital emergency setting ranges from 20% to 53%. Additionally, the scientific literature reveals a prevalence of moderate-to-severe pain in 20-64% of patients. According to the latest guidelines, it is essential to ensure proper and effective pain management for all patients experiencing pain. Inadequate pain management can result in complications such as delayed recovery and increased patient distress. In pre-hospital setting, emergency nurses are capable of assessing and treating pain using medications such as fentanyl, ketamine, morphine, NSAIDs and paracetamol.
Cite this article
ABSTRACT
Introduction: Numerous studies show that the prevalence of pain in pre-hospital emergency setting ranges from 20% to 53%. Additionally, the scientific literature reveals a prevalence of moderate-to-severe pain in 20-64% of patients. According to the latest guidelines, it is essential to ensure proper and effective pain management for all patients experiencing pain. Inadequate pain management can result in complications such as delayed recovery and increased patient distress. In pre-hospital setting, emergency nurses are capable of assessing and treating pain using medications such as fentanyl, ketamine, morphine, NSAIDs and paracetamol.
Objective: To evaluate the assessment and treatment of pain by emergency nurses in the pre-hospital setting and assess the potential need for additional training in accordance with the Tuscany region for nurse-staffed ambulances’ analgesia procedure guidelines.
Methods: Retrospective study of 4,738 pre-hospital interventions from September 2022 to September 2023. Data were retrieved from EmMaWeb system and included pain assessment using the Numeric Rating Scale (NRS) and administration of analgesics.
Results: Pain was assessed at least once in 98.3% of the cases. Moderate to severe pain (NRS ≥ 4) was recorded in 14.2% of the patients. Analgesic drugs were administered in 63.6% of patients with NRS ≥ 4, yet the Tuscany region for nurse-staffed ambulances’ analgesia procedure guidelines was not followed in 36.4% of these cases. 79% of the findings with NRS ≥ 7 (severe pain) received analgesic drug treatment. Paracetamol was the most commonly used analgesic, followed by fentanyl, morphine, and ketamine.
Conclusions: Pain assessment practices are well-established in pre-hospital care, but there is still room for improvement in pain management. Pain management does not comply with the Guidelines set by the World Health Organisation and the European Society of Emergency Medicine, a substantial proportion of patients experiencing moderate to severe pain did not receive adequate analgesia. This highlights the need for additional education and training for pre-hospital nurses in pain management and the effective use of analgesic medications to ensure greater adherence to the treatment protocols for nurse-staffed ambulance shared within the Tuscany Region.
Keywords: Pain management, Emergency nurses, Pre-hospital care, Analgesic drugs, Pain assessment
INTRODUCTION
Emergency Nurse can take on the role of Team Leader in a healthcare rescue team during severe criticality or clinical instability situations, even without the immediate presence of medical staff [1].
In the Italian healthcare system, where nursing protocols and algorithms for evaluation and treatment are adopted, it is increasingly common for nurses to apply their skills to achieve better results and ensure the success of the rescue operations [2,3].
One of the key interventions is the accurate assessment of pain, followed by rapid and appropriate treatment [4]. When conducted in and out-of-hospital setting, proper pain assessment can improve rescue interventions, representing a standard of quality and a marker of progress in Emergency Medicine [5,6]. Several studies indicate that the prevalence of acute pain in pre-hospital emergency medicine varies between 20% and 53%. [7-11]. Scientific literature also reveals a prevalence of moderate to severe pain in 20–64% of cases [7,8,12]. According to the latest guidelines, it is essential to ensure proper and effective pain management for all patients experiencing pain, starting from the pre-hospital emergency phase. The primary goal is to reduce pain, maintain functionality, and minimise adverse effects [13]. The WHO pain relief scale serves as a comprehensive guide for managing pain. The Numerical Rating Scale (NRS) is the most commonly used pain scale for assessing pain in adult patients within the pre-hospital setting [14].
The NRS can be administered either verbally or in written form. In both formats, patients are asked to rate the intensity of their pain on an 11-point scale, ranging from 0 (no pain) to 10 (worst pain imaginable [15,16]. Pain is considered mild with a score of 1-3, moderate with a score of 4-7, and severe with a score greater than 7 [17].
To improve the management of acute pain, continuous and accurate assessment is recommended. For adults and children capable of verbalising their pain, the NRS and VAS scales are recommended [14].
In Europe, the personnel involved in emergency and urgent healthcare consists of various roles: nurses, paramedics, and doctors. These roles have different levels of education, training, and job specifications, which can influence their ability and authority to administer analgesics to patients in pain [18-20]. The choice of the most effective analgesic depends on various factors, such as the context in which it is administered, the skills of the staff, and the guidelines provided by the WHO ladder [21]. The pharmacological options recommended by the European Society of Emergency Medicine (EUSEM) in accordance with the WHO pain relief ladder include: paracetamol, NSAIDs, opioids, and ketamine [14]. In Italy, scientific societies involved in emergency care have issued recommendations on pain management. According to guidelines, in pre-hospital setting, the ideal analgesic should be simple to use, safe, effective, not to interfere with transport time and have a rapid onset and short half-life to allow for dose titration based on the patient’s response [22].
Severe pain in a pre-hospital setting is often poorly and inadequately managed, with the use of analgesic drugs by healthcare professionals reported to be insufficient [23-25].
Nurses can assess and treat pain using drugs such as fentanyl, ketamine, morphine, NSAIDs, and paracetamol [22]. The effectiveness and safety of administering these drugs has been further confirmed by the 2023 recommendations for pain management in pre-hospital settings.
Pharmacological treatment with non-opioid analgesics, such as NSAIDs, Paracetamol, and Ketamine, is a viable alternative to opioid drugs, offering similar efficacy and a more favourable side effect profile [26]. Fentanyl is a rapid and effective analgesic treatment that does not cause significant hypotension, reduction in peripheral oxygen saturation (SpO2) and state of consciousness, therefore, it can be used safely and effectively for pain management in pre-hospital settings [27].
In addition, the safety of Ketamine in low-dose administration was demonstrated with no significant decrease in blood pressure, respiratory rate, heart rate and GCS, and no clinically significant negative events were reported [28]. Numerous studies provide evidence for the safety and efficacy of low-dose (0.1-0.3 mg/kg) Ketamine, whether administered intravenously, intramuscularly, or intranasal. Its use leads to rapid pain relief and causes fewer adverse effects, such as nausea and vomiting, compared to opioids, though it is associated with dizziness, dysphoria, and confusion [29-32].
In the context of prehospital emergency care in the Tuscany Region, various types of basic and advanced rescue vehicles are available: nurse-staffed ambulances, emergency physician cars, basic life support ambulances, and air ambulances. Regarding nurse-staffed ambulances, pain assessment and management are performed by nurses following the Regional Analgesia Procedure.
Pain assessment is performed using the NRS (Numerical Rating Scale), VRS [https://www.fisioscience.it/scale-valutazioni/scala-vrs/]
PAINAD (Pain Assessment in Advanced Dementia), FACES (Faces Pain Scale) and FLACC (Face, Legs, Activity, Cry, Consolability) scales.
The procedure includes the use of analgesic medications based on pain intensity:
- Paracetamol for pain intensity of 4-6
- Ketamine and Morphine for pain intensity ≥ 7
- Fentanyl is used by the operators of the Arezzo Emergency Medical Operations Centre following the implementation of the regional analgesia procedure.
This study was designed to evaluate nursing practices in pain management during pre-hospital care. Specifically, it aims to analyse adherence to international guidelines and the implementation of the Regional Analgesia Protocol by nursing staff affiliated with the Emergency Medical Operations Centre in Arezzo.
Objective:
The main objective of this study is to assess how the territorial emergency nurse evaluates and treats pain. The specific objectives are:
- To verify whether nurses assess pains by completing the relevant section in the rescue report and/or in the patient card filled out by the operational centre operators.
- To determine if a pain assessment with NRS ≥ 4 (moderate to severe pain) leads to appropriate pharmacological treatment.
- To identify the potential need for further training on pain management and analgesic treatment, in accordance with the Tuscany region for nurse-staffed ambulance’s analgesia procedure guidelines.
MATERIALS AND METHODS
A retrospective study was conducted on pain management by nurses on Advanced Life Support vehicles operated by the Local Health Authority of South-East Tuscany, one of the main healthcare providers in Central Italy, at the Emergency Medical Services Dispatch Centre in Arezzo. The regional analgesia procedure guidelines for nurse-staffed ambulances has been used by the healthcare authority.
The advanced life support vehicles involved in the study within the pre-hospital emergency care setting include:
- Ambulances staffed with qualified nurses trained to perform clinical procedures for pain assessment and management.
During pre-hospital care, healthcare professionals complete a standardised emergency care form.
This form includes information about the patient’s physical condition, such as pain intensity rated on a 0-10 Numerical Rating Scale (NRS), the type of event, and the pre-hospital triage colour code.
The NRS is a widely recognised pain assessment tool where 0 represents no pain and 10 represents the worst possible pain. For the pharmacological treatment of pain, a Regional Procedure is in place for nurse-staffed ambulances, allowing the administration of analgesic drugs based on the severity of the pain:
- Moderate pain (NRS: 4–6):
- Intravenous Paracetamol up to 15 mg/kg intravenous in children.
- Paracetamol 1 gr in adults.
- In cases of post-traumatic pain, Methoxyflurane is administered via pre-dosed inhalation.
- Severe pain (NRS≥ 7):
- Intravenous Ketamine 0.2-0.5 mg/kg after prior consultation with the dispatch centre physician via telephone.
- Ketamine intramuscular 0.5-1 mg/kg if venous access is not available.
- Intravenous morphine in children: 0.05 mg/kg
- Intravenous morphine for adult patients under 65 years of age: 4 mg (repeatable with 2 mg).
- Intravenous morphine for adult patients over 65 years of age: 2 mg, repeatable with 1 mg if necessary.
The period covered by the study was from 1 September 2022 to 30 September 2023.
Data were extracted from the EmMaWeb (Emergency Management Web) database used by Arezzo Emergency Medical Service Operative Centre, which includes the “rescue report” filled out by the nurse on board and the “patient card” filled by the healthcare personnel at Emergency Medical Service Operative Centre. The data were accessed using an Excel spreadsheet and selected based on the defined inclusion criteria. To achieve the study’s objective, the following outcomes were evaluated:
- At least one recorded pain score using the pain scale.
- Presence and intensity of pain.
- Adherence to the Regional Analgesia Procedure for Advanced Life Support ambulances with a nurse for the pharmacological treatment of pain.
Inclusion Criteria
- All patients assisted, with no age restrictions.
- Emergency medical care administered by nurses on board ambulances.
- Pre-hospital Emergency Care forms dated between 1 September 2022, and 30 September 2023.
- All pre-hospital colour codes for the dispatch of the rescue vehicle and its return to the destination hospital.
Exclusion Criteria
- Pre-hospital emergency care provided by non-healthcare professionals in non-advanced life support vehicles.
- Pre-hospital emergency care delivered by Medical Cars.
Statistical analysis
Data was extracted from the EmMaWeb (Emergency Management Web) database using the MISEMMA program. Data were collected and analysed to describe the distribution of pain based on intensity levels. The categorical variables were presented as simple and cumulative frequencies, as well as percentages. Additionally, a 95% confidence interval (CI 95%) was provided.
A hypothesis test was conducted as an inferential procedure using a z-test for proportions to evaluate whether the frequency of moderate-to-severe pain observed differed significantly from the lower limit of the expected frequency reported in the literature. Furthermore, the p-value was calculated, with a significance level set at <0.05. For the data analysis, Microsoft 365 Excel version 2411 was used.
Ethical consideration
This study constitutes an integral component of the nursing thesis carried out by the first author, supervised by the second author at the second level degree in Nursing Science, University of Perugia. The thesis was submitted for approval on 24 November 2023.
No formal approval by the Local Ethics Committee (LEC) was required for this study; moreover, as by internal guidelines of LEC, the study has obtained necessary approval from the Directorate General of Local Health Authority Tuscany South-East (‘Arezzo’ Hospital) (18 September 2023).
All clinical data used in this investigation were acquired in a coded and anonymised format, adhering rigorously to the principles and guidelines outlined in the General Data Protection Regulation (2016/679, ‘GDPR’), which encompasses regulations concerning data protection and privacy within the European Union.
Furthermore, the study complies with the tenets of the Privacy Code (Italian legislative decrees 196/2003 and 101/2018) and the study protocol was designed in accordance with Good Clinical Practice, and the study was conducted in accordance with the Declaration of Helsinki.
RESULTS
During the selected period (September 2022 to September 2023), 4,738 rescue interventions were carried out by ambulances with nurses on board (Figure 1).
The number of interventions is related to the extent of the territorial coverage Emergency Medical Service Nurses (in Italian “INDIA”), population density, and whether the territorial emergency medical service provides 24-hour or 12-hour coverage.
In 4,658 out of 4,738 cases (98.3%), pain was recorded at least once by the nurse in the rescue report and/or in the patient card completed by the operations centre staff, while it was not recorded in 80 cases (1.7%). Among the 80 patients whom no pain recording was found, 17 patients (0.37%) still received analgesic treatment.
Pain assessments with NRS (Numerical Rating Scale) ≥ 4 (moderate to severe pain) accounted for 14.2% (n= 660), while those with NRS (Numerical Rating Scale) ≤ 3 (no to mild pain) represented 85.8% (n= 3,998).
Out of the total pain assessments performed (4,658), severe pain (NRS ≥ 7) was observed in 4.30% of cases (n = 200) [95% confidence interval (CI): 3.71–4.87], moderate pain (6 ≥ NRS ≥ 4) in 9.87% of cases (n = 460) [95% CI: 9.01–10.73], while absent or mild pain (NRS ≤ 3) accounted for 85.83% of cases (n = 3998) [95% CI: 84.83–86.83] (Figure 1).
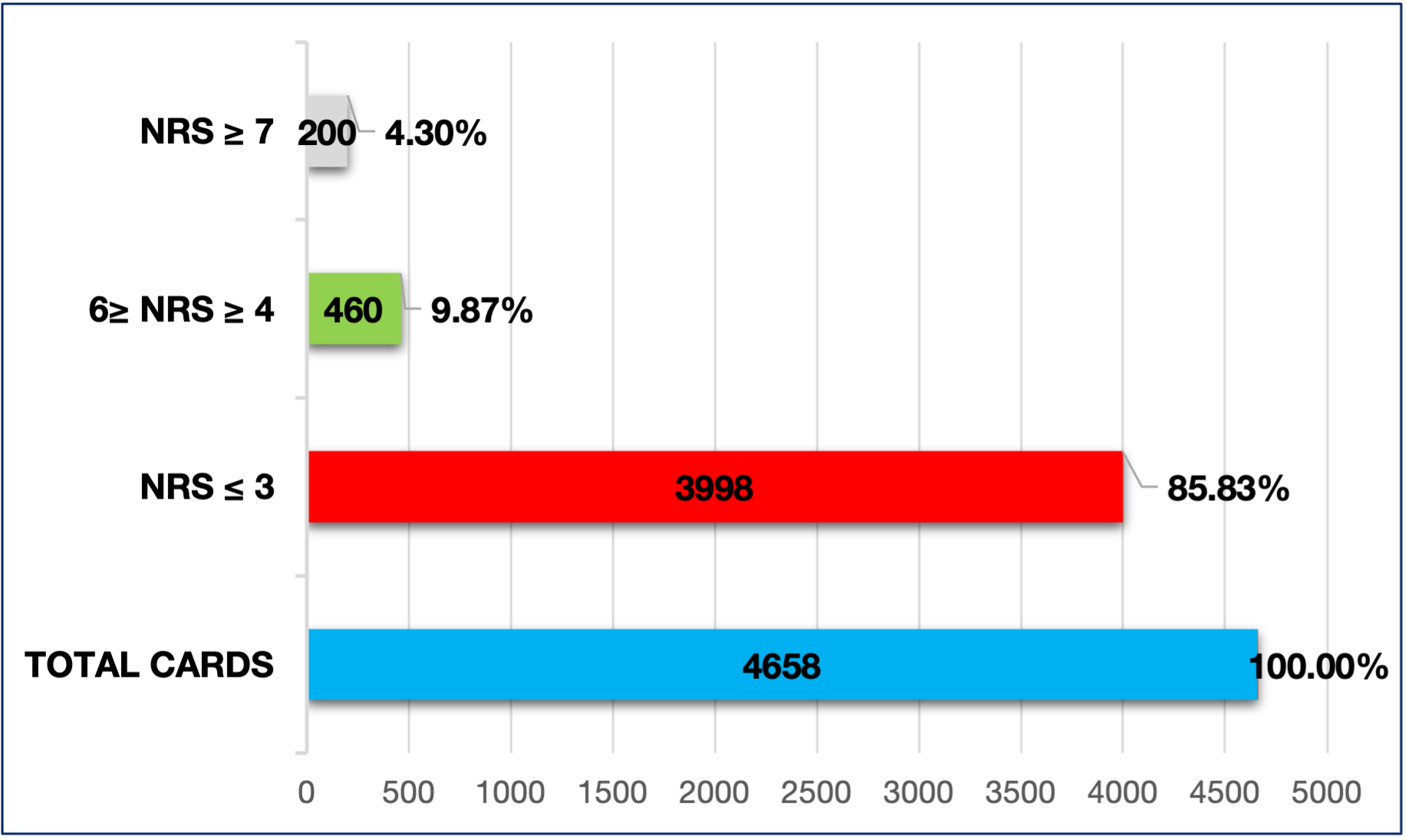 Figure 1. Number of measurements with NRS (Numerical Rating Scale) ≤ 3 (no pain and mild pain); 6 ≥ NRS (Numerical Rating Scale) ≥ 4 (moderate pain), and NRS (Numerical Rating Scale) ≥ 7 (severe pain) on total cards.
Figure 1. Number of measurements with NRS (Numerical Rating Scale) ≤ 3 (no pain and mild pain); 6 ≥ NRS (Numerical Rating Scale) ≥ 4 (moderate pain), and NRS (Numerical Rating Scale) ≥ 7 (severe pain) on total cards.
Cumulative frequency
Total of measurements with NRS (Numerical Rating Scale) between 0 and 10 were 4,658, those with absent or mild pain (NRS ≤ 3) 3,998 (85.83%). The findings with absent-mild-moderate pain (NRS ≤ 6) were 4,458 (95.70%) (Figure 2).
To assess whether the observed frequency of pain with NRS ≥ 4 (moderate-severe) at 14.2% significantly differs from the lower limit of the expected frequency reported in the literature (20%), a z-test for proportions was conducted on a sample of 4,658 subjects.
The null hypothesis (H₀) posits that the observed proportion is equal to the expected proportion, while the alternative hypothesis (H₁) asserts that the observed proportion is lower than the expected proportion.
The z-test for proportions yielded a value of -9.90, indicating that the observed proportion (14.2%) is significantly below the expected proportion (20%). The associated p-value is extremely close to 0, well below the significance threshold (p-value < 0.05).
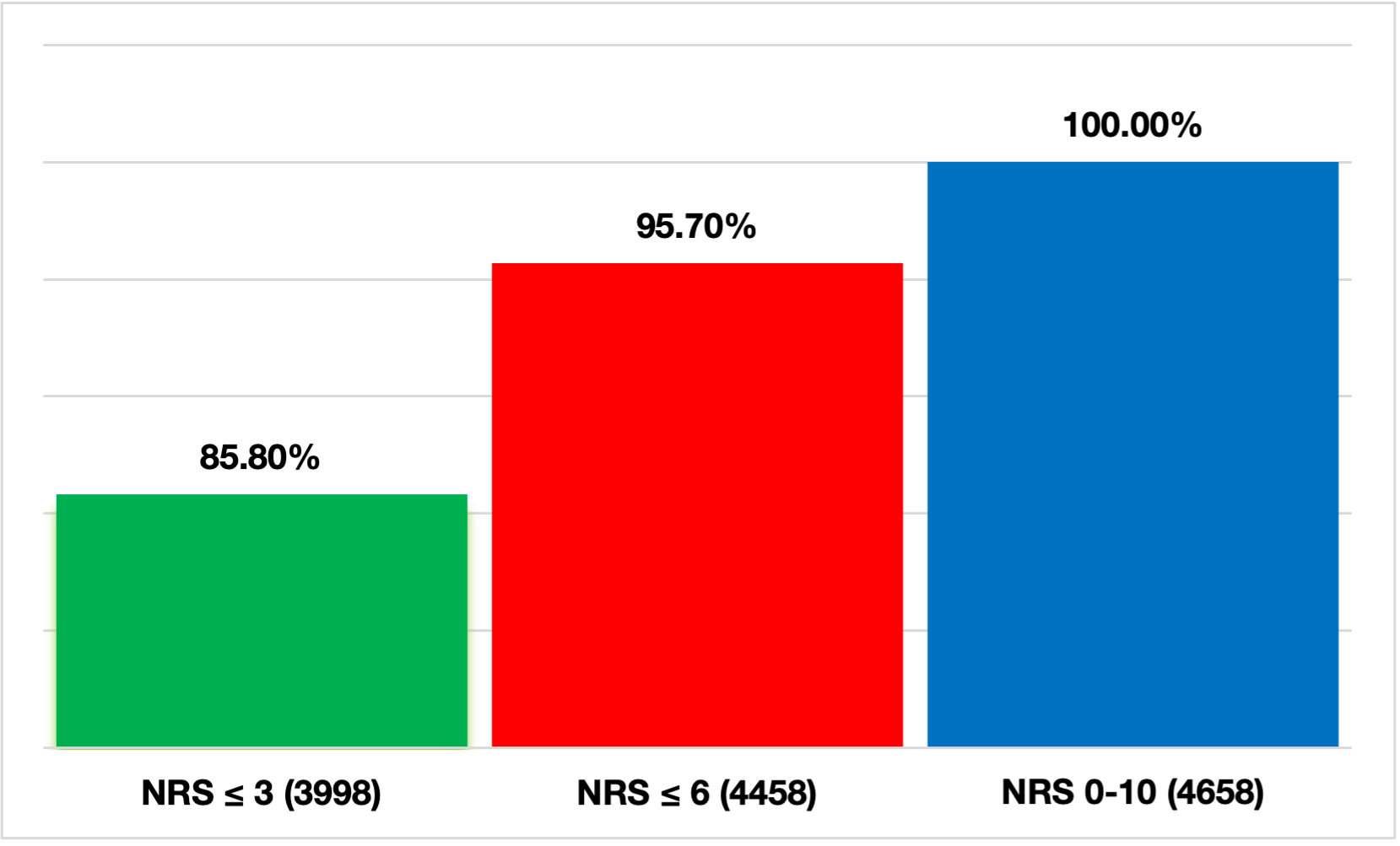 Figure 2. Representation of the cumulative frequency divided by the number and percentages of pain measurements with NRS (Numerical Rating Scale) ≤ 3 (no pain and mild pain), NRS (Numerical Rating Scale) ≤ 6 (no pain, mild pain, moderate pain), and NRS (Numerical Rating Scale) 0-10 (no pain, mild pain, moderate pain, severe pain).
Figure 2. Representation of the cumulative frequency divided by the number and percentages of pain measurements with NRS (Numerical Rating Scale) ≤ 3 (no pain and mild pain), NRS (Numerical Rating Scale) ≤ 6 (no pain, mild pain, moderate pain), and NRS (Numerical Rating Scale) 0-10 (no pain, mild pain, moderate pain, severe pain).
Analgesic drugs were administered following a pain assessment NRS ≥ 4 in 63.6% of cases (420 out of 660 assessments), while the procedure was not applied in 240 cases (36.4%).
Following a pain assessment with NRS ≥ 7 (severe pain), the analgesia procedure was applied in 79% of cases (n = 158), while it was not applied in the remaining 21% of patients (n = 42).
It was highlighted in the study, when pain intensity, as reported by the patient, decreased to a NRS between 4 and 6, there was a significant drop in number of analgesic treatments administered: 262 out of 460 cases (57%) received treatment, while 43% (198 out of 460) did not receive any.
As regard of analgesic drug usage, both NRS ≤ 3 and NRS ≥ 4, paracetamol was the most commonly administered drug (815 cases), followed by fentanyl (181), morphine (102), and ketamine (94) (Table 1).
| FENTANYL | KETAMINE | MORPHINE | PARACETAMOL | |
| INDIA 1 | 5 | 1 | 1 | 1 |
| INDIA 2 | 26 | 10 | 35 | 128 |
| INDIA 3 | 24 | 14 | 4 | 97 |
| INDIA 4 | 13 | 11 | 4 | 61 |
| INDIA 5 | 14 | 9 | 4 | 52 |
| INDIA 6 | 47 | 25 | 27 | 194 |
| INDIA 7 | 23 | 17 | 17 | 125 |
| INDIA 8 | 6 | 3 | 0 | 49 |
| INDIA 9 | 15 | 3 | 10 | 64 |
| INDIA 10 | 8 | 1 | 0 | 44 |
| TOTALE | 181 (15.2%) | 94 (7.9%) | 102 (8.5%) | 815 (68.4%) |
Table 1. Total number of drugs administered for NRS (Numerical Rating Scale) ≤ 3 and NRS ≥ 4 by Advanced Life Support ambulances staffed with nurses (INDIA).
DISCUSSION
The data shows a high level of awareness about pain, as it was assessed at least once in more than 98% of patients.
Only 1.7% of the examined forms lacked of pain assessment, a significantly better result compared to other studies reported in the literature, where the percentage ranges from 32% to 52% [8,12,20].
The recording of pain data during pre-hospital emergency, as recommended by the European Society of Emergency Medicine (EUSEM) guidelines and constitutes the first step towards effective pain management [13]. An accurate assessment of the patient and their pain symptoms is essential for selecting the appropriate analgesic and determining the most suitable route of administration [22].
A proper pain assessment can significantly enhance emergency care interventions, establishing it as one of the key quality standards in emergency medicine [5,6].
There were 17 out of 80 cases where no pain score was recorded, but patients still received pharmacological analgesic treatment.
For cases where no pain score was documented, several factors could explain this: some patients likely did not experience pain, while in other cases, patients may have had pain, but the data was not recorded for various reasons. This underscores the importance of thorough documentation to ensure accurate pain management practices [12].
From the analysed data, it is clear that about 36% of patients with NRS ≥ 4 (moderate-severe pain) and 21% of patients with NRS ≥ 7 (severe pain) did not receive analgesic treatment.
Numerous studies prove that inadequate pain management is common in pre-hospital Emergency-Urgency setting [33,34]. In another study, only 15.6% of all activations documented the receipt of pre-hospital pain medications [35]. One hypothesis related to 40% of moderate to severe pain cases left untreated by nurses could be from a lack of confidence in using the available analgesic drugs.
From the data examined, the occurrence of pain with NRS ≥ 4 (moderate-severe) is greatly reduced (14.2%) if compared to the 20-64% reported in the medical literature [7,8,12].
The z-test value for proportions, which is highly negative, confirms that the observed proportion of moderate-to-severe pain (14.2%) is significantly below the lower limit of the expected range (20%). The value observed in this study is statistically lower than the expected range reported in the literature, supporting the conclusion that the collected data differs significantly from expectations. Given that the p-value is extremely close to zero, we can reject the null hypothesis that the observed distribution of moderate-to-severe pain is equal to the expected distribution.
Regarding the use of analgesic drugs, paracetamol appears to be the most frequently used medication for both NRS ≥ 4 and NRS ≤ 3 pain levels, suggesting nurses are more comfortable with its use and titration, compared to the lower usage of fentanyl, ketamine, and morphine.
The widespread use of intravenous paracetamol is supported by the recommendations of the “Evidence-Based Guidelines for Pre-Hospital Pain Management”. Compared to the exclusive use of intravenous opioids for the initial management of moderate to severe pain, paracetamol is highlighted for its ease of administration and higher tolerability among patients. This makes it a preferred option in pre-hospital settings where effective, yet patient-friendly analgesic interventions are critical. [26]
In other studies, morphine and fentanyl have been the most commonly administered drugs for pain management [35]. A growing need of a better training on how to use painkiller drug is urgent, in particular about the benefits of a valid analgesia. It’s important, especially in certain provincial areas under the responsibility of Advanced Life Support ambulances with a nurse on board (INDIA), which were found to be less consistent in using analgesic drugs relative to the number of rescue interventions performed.
CONCLUSION
Acute pain is widely documented as one of the most common symptoms experienced by patients in the context of emergency and urgent care. This symptom is frequently encountered in pre-hospital settings, highlighting the importance of effective pain management during emergency interventions. [8,36]. According to Mackenzie, pain should be controlled from the very beginning, immediately after the arrival of emergency services: “The pre-hospital care professional has the first and perhaps the only opportunity to interrupt the pain cascade.” This emphasises the crucial role that early intervention plays in managing pain effectively during emergency care [37].
Early and effective pain treatment has a positive impact on both the physiological and psychological condition of patients. It improves comfort and safety, facilitates complex life-support interventions, and, in the long term, reduces the development of post-traumatic stress disorder (PTSD) [23,38-40].
The recently concluded study provides a realistic snapshot of the management of pre-hospital emergencies handled by the Emergency Medical Operations Centre of Arezzo.
The objectives of the study were met, demonstrating that Emergency Medical Service nurses pay considerable attention to assess and treat pain in patients seeking assistance.
63,6% of patients with moderate to severe pain (NRS ≥ 4) received pharmacological treatment through the application of the Tuscany region for nurse-staffed ambulances’ analgesia procedure guidelines. Pain management, however, does not align with the guidelines set by the World Health Organisation (WHO) and the European Society of Emergency Medicine (EUSEM) [14], a significant proportion of patients with moderate-severe pain did not receive adequate analgesia.
Nevertheless, the study also highlights the need for a further training to raise awareness about the benefits of analgesia. However, the study suggests a need for further education and training for pre-hospital nurses on pain management and the use of analgesic drugs to ensure greater adherence to shared treatment protocols within the Tuscany Region. It would be ideal for personnel working in the emergency and urgent care system to undergo a uniform training path, while maintaining their respective competencies, professional scopes, and specific foundational training for each role. The overall goal is to ensure quality care through the functional and operational integration of each sector within the emergency and urgent healthcare system. [41] Nonetheless, the adoption of the assessment and treatment nursing protocols for assessment at the regional level, including the Analgesia Protocol, represents a positive step towards the standardisation of care.
Study limitations:
The main limitation is the data which were collected from a single Emergency Medical Service Operative Centre.
Data regarding the sex, age, and medical conditions of patients treated by Advanced Life Support ambulances with a nurse on board were not collected. Additionally, the lack of pain assessment prevents us from determining whether this omission was due to a genuine absence of pain evaluation or a failure to record the pain, even though it may have been assessed.
Further investigation is needed using the collected data through a direct review of each individual rescue report, in order to establish the reasons of inapplicable regional analgesia procedure guidelines, despite the patient’s reported pain being classified as moderate to severe.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or non-profit sectors.
Conflict of interest
The authors report no conflict of interest.
Authors’ contribution
F.P.: Conceptualisation, Methodology, Investigation, Software Data curation, Writing-Original draft preparation. G.d.G.: Writing – Reviewing and Editing, Supervision. S.S.: Writing- Reviewing and Editing. M.R.: Writing- Reviewing and Editing.
Acknowledgements
We would like to thank the Medical and Nursing Management of the Department of Emergency Medicine of Local Health Authority South-East Tuscany for allowing us to study inside the COES Arezzo.
REFERENCES
- Yamaguchi Y, Matsunaga-Myoji Y, Fujita K. Advanced practice nurse competencies to practice in emergency and critical care settings: A scoping review. Int J Nurs Pract. 2024 Aug;30(4):e13205. https://doi.org/10.1111/ijn.13205
- Mazzolini, E., Garrino, L., & Calabrò, P. (2006). Integration of nursing staff into Medical Emergency Service 118. Emergency Care Journal, 2(4), 29–35. https://doi.org/10.4081/ecj.2006.4.29
- Campo TM, Comer A, Dowling Evans D, Kincaid K, Norton L, Ramirez EG, et al. Practice Standards for the Emergency Nurse Practitioner Specialty. Adv Emerg Nurs J. 2018 Oct/Dec;40(4):240-245. https://doi.org/10.1097/TME.0000000000000209
- Whitley, G. A., Wijegoonewardene, N., Nelson, D., Curtis, F., Ortega, M., & Siriwardena, A. N. (2023). Patient, family member, and ambulance staff experiences of pre-hospital acute pain management in adults: A systematic review and meta-synthesis. Journal of the American College of Emergency Physicians open, 4(2), e12940. https://doi.org/10.1002/emp2.12940
- Studnek JR, Fernandez AR, Vandeventer S, Davis S, Garvey L. The association between patients’ perception of their overall quality of care and their perception of pain management in the pre-hospital setting. Prehosp Emerg Care. 2013 Jul-Sep;17(3):386-91. https://doi.org/10.3109/10903127.2013.764948.
- Ariès P, Montelescaut E, Pessey F, Danguy des Déserts M, Giacardi C. Pre-hospital emergency medicine: pain control. Lancet. 2016 Feb 20; 387(10020):747. https://doi.org/10.1016/S0140-6736(16)00325-1.
- Galinski M, Ruscev M, Gonzalez G, Kavas J, Ameur L, Biens D, et al. Prevalence and management of acute pain in pre-hospital emergency medicine. Prehosp Emerg Care. 2010 Jul-Sep;14(3):334-9. https://doi.org/10.3109/10903121003760218.
- McLean SA, Maio RF, Domeier RM. The epidemiology of pain in the pre-hospital setting. Prehosp Emerg Care. 2002 Oct-Dec;6(4):402-5. doi: 10.1080/10903120290938021.
- Ricard-Hibon A, Leroy N, Magne M, Leberre A, Chollet C, Marty J. Evaluation de la douleur aiguë en médecine préhospitalière. Ann Fr Anesth Reanim. 1997;16(8):945-9. French. doi: 10.1016/s0750-7658(97)82142-9.
- Lord B, Cui J, Kelly AM. The impact of patient sex on paramedic pain management in the pre-hospital setting. Am J Emerg Med. 2009 Jun;27(5):525-9. doi: 10.1016/j.ajem.2008.04.003.
- Milojevic K, Cantineau JP, Simon L, Bataille S, Ruiz R, Coudert B, et al. Douleur aiguë intense en médecine d’urgence. Les clefs d’une analgésie efficace. Ann Fr Anesth Reanim. 2001 Nov;20(9):745-51. French. doi: 10.1016/s0750-7658(01)00482-8.
- Friesgaard KD, Riddervold IS, Kirkegaard H, Christensen EF, Nikolajsen L. Acute pain in the pre-hospital setting: a register-based study of 41.241 patients. Scand J Trauma Resusc Emerg Med. 2018;26(1):53. doi:10.1186/s13049-018-0521-2
- Hachimi-Idrissi S, Dobias V, Hautz WE, Leach R, Sauter TC, Sforzi I, et al., Approaching acute pain in emergency settings; European Society for Emergency Medicine (EUSEM) guidelines-part 2: management and recommendations. Intern Emerg Med. 2020 Oct;15(7):1141-1155. Epub 2020 Sep 15. doi: 10.1007/s11739-020-02411-2.
- Guidelines for the management of acute pain in emergency situations, EUSEM (European Society of Emergency Medicine) 2020. Last accessed: November 20, 2024. Available at: https://www.eusem.org/images/EUSEM_EPI_GUIDELINES_MARCH_2020.pdf
- Breivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Hals EK, et al., Assessment of pain. Br J Anaesth. 2008 Jul;101(1):17-24. Epub 2008 May 16. doi: 10.1093/bja/aen103.
- Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis. 1978 Aug;37(4):378-81. doi: 10.1136/ard.37.4.378.
- Hartrick CT, Kovan JP, Shapiro S. The numeric rating scale for clinical pain measurement: a ratio measure? Pain Pract. 2003 Dec;3(4):310-6. doi: 10.1111/j.1530-7085.2003.03034.x.
- Albrecht E, Taffe P, Yersin B, Schoettker P, Decosterd I, Hugli O. Undertreatment of acute pain (oligoanalgesia) and medical practice variation in pre-hospital analgesia of adult trauma patients: a 10 yr retrospective study. Br J Anaesth. 2013 Jan;110(1):96-106. Epub 2012 Oct 11. doi: 10.1093/bja/aes355.
- Motov SM, Khan AN. Problems and barriers of pain management in the emergency department: Are we ever going to get better? J Pain Res. 2008 Dec 9;2:5-11. https://doi.org/10.2147/JPR.S4324.
- Siriwardena AN, Asghar Z, Lord B, Pocock H, Phung VH, Foster T, et al., Patient and clinician factors associated with pre-hospital pain treatment and outcomes: cross sectional study. Am J Emerg Med. 2019 Feb;37(2):266-271. doi: 10.1016/j.ajem.2018.05.041. Epub 2018 May 23.
- World Health Organisation (WHO). Cancer pain ladder. Last accessed: November 10, 2024. Available at: Available at http://www.who.int/cancer/palliative/painladder/en/
- Savoia, G., Coluzzi, F., Di Maria, C., Ambrosio, F., Della Corte, F., Oggioni, R., et al. Italian Intersociety Recommendations on pain management in the emergency setting (SIAARTI, SIMEU, SIS 118, AISD, SIARED, SICUT, IRC). Available at: https://www.siaarti.it/news/371885. Last access: 15 January 2025.
- Akbas S, Castellucci C, Nehls F, Müller SM, Spahn DR, Kaserer A. Präklinische Schmerztherapie: Übersicht und Verbesserungsmöglichkeiten. Praxis (Bern 1994). 2022;111(3):157-162. German. https://doi.org/10.1024/1661-8157/a003810
- Friesgaard KD, Kirkegaard H, Rasmussen CH, Giebner M, Christensen EF, Nikolajsen L. Pre-hospital intravenous fentanyl administered by ambulance personnel: a cluster-randomised comparison of two treatment protocols. Scand J Trauma Resusc Emerg Med. 2019 Feb 7;27(1):11. https://doi.org/10.1186/s13049-019-0588-4.
- Ferri P, Gambaretto C, Alberti S, Parogni P, Rovesti S, Di Lorenzo R, et al. Pain Management in a Pre-hospital Emergency Setting: A Retrospective Observational Study. J Pain Res. 2022 Oct 27;15:3433-3445. https://doi.org/10.2147/JPR.S376586.
- Lindbeck G, Shah MI, Braithwaite S, Powell JR, Panchal AR, Browne LR, et al., Evidence-Based Guidelines for Pre-hospital Pain Management: Recommendations. Prehosp Emerg Care. 2023;27(2):144-153. doi: 10.1080/10903127.2021.2018073. Epub 2022 Jan 25.
- Friesgaard KD, Nikolajsen L, Giebner M, Rasmussen CH, Riddervold IS, Kirkegaard H, et al. Efficacy and safety of intravenous fentanyl administered by ambulance personnel. Acta Anaesthesiol Scand. 2016 Apr;60(4):537-43. https://doi.org/10.1111/aas.12662.
- Bronsky ES, Koola C, Orlando A, Redmond D, D’Huyvetter C, Sieracki H, et al. Intravenous Low-Dose Ketamine Provides Greater Pain Control Compared to Fentanyl in a Civilian Pre-hospital Trauma System: A Propensity Matched Analysis. Prehosp Emerg Care. 2019 Jan-Feb;23(1):1-8. https://doi.org/10.1080/10903127.2018.1469704.
- Shimonovich S, Gigi R, Shapira A, Sarig-Meth T, Nadav D, Rozenek M, et al. Intranasal ketamine for acute traumatic pain in the Emergency Department: a prospective, randomized clinical trial of efficacy and safety. BMC Emerg Med. 2016 Nov 9;16(1):43. https://doi.org/10.1186/s12873-016-0107-0.
- Sandberg M, Hyldmo PK, Kongstad P, Dahl Friesgaard K, Raatiniemi L, Larsen R, et al. Ketamine for the treatment of pre-hospital acute pain: a systematic review of benefit and harm. BMJ Open. 2020 Nov 24;10(11):e038134. https://doi.org/10.1136/bmjopen-2020-038134.
- Ghate G, Clark E, Vaillancourt C. Systematic review of the use of low-dose ketamine for analgesia in the emergency department. Can J Emergency Med. 2018;20(1):36–45. Epub 2017/06/28. https://doi.org/1017/cem.2017.48.
- Ahern TL, Herring AA, Anderson ES, Madia VA, Fahimi J, Frazee BW. The first 500: initial experience with widespread use of low-dose ketamine for acute pain management in the ED. Am J Emerg Med. 2015;33(2):197–201. Epub 2014/11/15.https://doi.org/10.1016/j.ajem.2014.11.010
- Oberholzer N, Kaserer A, Albrecht R, Seifert B, Tissi M, Spahn DR, et al. Factors Influencing Quality of Pain Management in a Physician Staffed Helicopter Emergency Medical Service. Anesth Analg. 2017 Jul;125(1):200-209. doi: 10.1213/ANE.0000000000002016
- Helm M, Hossfeld B, Braun B, Werner D, Peter L, Kulla M. Oligoanalgesia in Patients with an Initial Glasgow Coma Scale Score ≥8 in a Physician-Staffed Helicopter Emergency Medical Service: A Multicentric Secondary Data Analysis of >100,000 Out-of-Hospital Emergency Missions. Anesth Analg. 2020 Jan;130(1):176-186. doi: 10.1213/ANE.0000000000004334.
- Hewes, H. A., Dai, M., Mann, N. C., Baca, T., & Taillac, P. (2017). Pre-hospital Pain Management: Disparity By Age and Race. Pre-hospital Emergency Care, 22(2), 189–197. https://doi.org/10.1080/10903127.2017.1367444
- Jennings PA, Cameron P, Bernard S. Epidemiology of pre-hospital pain: an opportunity for improvement. Emerg Med J. 2011 Jun;28(6):530-1. doi: 10.1136/emj.2010.098954. Epub 2010 Aug 2.
- Mackenzie R. Analgesia and sedation. J R Army Med Corps. 2004;150: S45-S55. https://doi.org/10.1136/jramc-146-02-14
- Shehabi Y, Al-Bassam W, Pakavakis A, Murfin B, Howe B. Optimal Sedation and Pain Management: A Patient- and Symptom-Oriented Paradigm. Semin Respir Crit Care Med. 2021 Feb;42(1):98-111. https://doi.org/10.1055/s-0040-1716736.
- Mc Mullan J, Droege C, Strilka R, Hart K, Lindsell C. Intranasal Ketamine as an Adjunct to Fentanyl for the Pre-Hospital Treatment of Acute Traumatic Pain: Design and Rationale of a Randomized Controlled Trial. Prehosp Emerg Care. 2021 Jul-Aug;25(4):519-529. https://doi.org/10.1080/10903127.2020.1808746.
- Holbrook TL, Galarneau MR, Dye JL, Quinn K, Dougherty AL. Morphine use after combat injury in Iraq and post-traumatic stress disorder. N Engl J Med. 2010 Jan 14;362(2):110-7. https://doi.org/10.1056/NEJMoa0903326
- Zamardi E, Sorrentino D, Inglese L, Beghi M, Gandolfi A, Nani S, et al. La soddisfazione del personale tecnico non sanitario del sistema di emergenza-urgenza territoriale dopo intervento formativo dell’infermiere mediante simulazione: uno studio retrospettivo. Scenario;38(2):35-40.
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
